Definition
The porphyrias are a group of rare disorders that affect heme biosynthesis. Heme is an essential component of hemoglobin as well as of many enzymes throughout the body.
Description
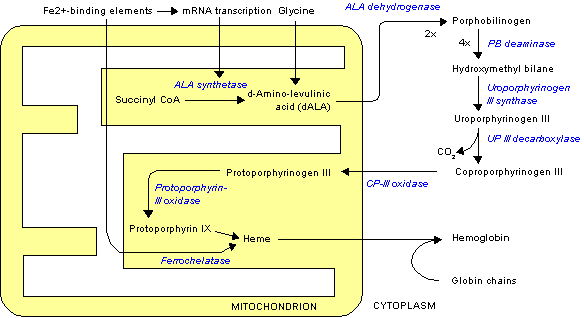
Biosynthesis of heme is a multistep process that starts with simple molecules and ends with a large, complex heme molecule. Each step of the biosynthesis pathway is directed by its own enzyme (a task-specific protein). As a heme precursor molecule moves through each step, an enzyme modifies it in some way. If the precursor is not modified, it cannot proceed to the next step.
The main characteristic of the porphyrias is a defect in one of the enzymes of the heme biosynthesis pathway. The defect prevents protoporphyrins or porphyrin (heme precursors) from proceeding further along the pathway. Symptoms may be debilitating or life-threatening in some cases. Porphyria is an inherited condition, but it may be acquired after exposure to poisonous substances.
Heme
Heme is primarily synthesized in the liver and bone marrow. Heme synthesis for immature red blood cells, namely the erythroblasts and the reticulocytes, occurs in the bone marrow.
Although production is concentrated in the liver and bone marrow, heme is used in various capacities in virtually every tissue in the body. In most cells, it is a key building block in the construction of factors that oversee metabolism as well as transport of oxygen and energy. In immature red blood cells, heme is a featured component of hemoglobin. Hemoglobin is the red pigment that gives red blood cells the ability to transport oxygen as well as their characteristic color.
Heme biosynthesis
The heme molecule is composed of porphyrin and an iron atom. Much of the heme biosynthesis pathway is dedicated to constructing the porphyrin molecule. Porphyrin is a large molecule shaped like a four-leaf clover. An iron atom is placed at its center during the last step of heme biosynthesis.
The production of heme may be compared to a factory assembly line. The heme "assembly line" is an eight-step process, requiring eight different-and properly functioning-enzymes:
- Step 1: delta-aminolevulinic acid synthase.
- Step 2: delta-aminolevulinic acid dehydratase.
- Step 3: porphobilogen deaminase.
- Step 4: uroporphyrinogen III cosynthase.
- Step 5: uroporphyrinogen decarboxylase.
- Step 6: coproporphyrinogen oxidase.
- Step 7: protoporphyrinogen oxidase.
- Step 8: ferrochelatase.
The control of heme biosynthesis is complex. There are various chemical signals that can trigger increased or decreased production. These signals can affect the enzymes themselves or their production, starting at the genetic level.
Porphyrias
Under normal circumstances, when heme concentrations are at an appropriate level, precursor production decreases. However, a malfunction in the biosynthesis pathway-represented by a defective enzyme-means that heme biosynthesis does not reach completion. Because heme levels remain low, the synthesis pathway continues to churn out precursor molecules in an attempt to make up the deficit.
The net effect of this continued production is an abnormal accumulation of precursor molecules and development of some type of porphyria. Each type of porphyria corresponds to a specific enzyme defect and an accumulation of the associated precursor. Although there are eight steps in heme biosynthesis, there are only seven types of porphyrias; a defect in ALA synthase activity does not have a corresponding porphyria.
The porphyrias are divided into two general categories, depending on the location of the deficient enzyme. Porphyrias that affect heme biosynthesis in the liver are called hepatic porphyrias. The porphyrias that affect heme biosynthesis in immature red blood cells are called erythropoietic porphyrias. (Erythropoiesis is the process through which red blood cells are produced.)
Incidence of porphyria varies widely between types and occasionally by geographic location. Although certain porphyrias are more common than others, their greater frequency is only relative to other types; all porphyrias are considered rare disorders.
The hepatic porphyrias, and the heme biosynthesis steps at which enzyme defects occur, are:
- ALA dehydratase deficiency porphyria (step 2). This porphyria type is extraordinarily rare; only six cases have ever been reported in the medical literature. The inheritance pattern seems to be autosomal recessive, which means a defective enzyme gene must be inherited from both parents for the disorder to occur.
- Acute intermittent porphyria (step 3). Acute intermittent porphyria (AIP) is also known as Swedish porphyria, pyrroloporphyria, and intermittent acute porphyria. AIP is inherited as an autosomal dominant trait, which means only one copy of the defective gene needs to be present for the disorder to occur. However, simply inheriting this gene does not necessarily mean that a person will develop the disease. Approximately five to 10 per 100,000 persons in the United States carry the gene, but only 10% of carriers ever develop AIP symptoms.
- Porphyria cutanea tarda (step 5). Porphyria cutanea tarda (PCT) is also called symptomatic porphyria, porphyria cutanea symptomatica, and idiosyncratic porphyria. PCT may be acquired, typically as a result of disease (especially hepatitis C), drug or alcohol abuse, or exposure to certain poisons. PCT may also be inherited as an autosomal dominant disorder, but most people with the inherited form remain latent-that is, symptoms never develop. It is the most common of the porphyrias, but the incidence is not well defined.
- Hereditary coproporphyria (step 6). Hereditary coproporphyria (HCP) is inherited in an autosomal dominant manner. As with all porphyrias, it is an uncommon ailment. By 1977, only 111 cases were recorded; in Denmark, the estimated incidence is two in 1 million people.
- Variegate porphyria (step 7). Variegate porphyria (VP) is also known as porphyria variegata, protocoproporphyria, South African genetic porphyria, and Royal malady (supposedly King George III of England and Mary, Queen of Scots, suffered from VP). VP is inherited in an autosomal dominant manner and is especially prominent in South Africans of Dutch descent. Among that population, the incidence is approximately three in 1,000 persons, and it is estimated that there are 10,000 cases of VP in South Africa. Interestingly, it seems that the affected South Africans are descendants of two Dutch settlers who came to South Africa in 1680. Elsewhere, the incidence is estimated to be one to two cases per 100,000 persons.
The erythropoietic porphyrias, and the steps of heme biosynthesis at which they occur, are:
- Congenital erythropoietic porphyria (step 4). Congenital erythropoietic porphyria (CEP) is also called Günther's disease, erythropoietic porphyria, congenital porphyria, congenital hematoporphyria, and erythropoietic uroporphyria. CEP is inherited in an autosomal recessive manner and occurs very rarely. Onset of symptoms usually occurs in infancy, but may be delayed until adulthood.
- Erythropoietic protoporphyria (step 8). Also known as protoporphyria and erythrohepatic protoporphyria, erythropoietic protoporphyria (EPP) is more common than CEP; more than 300 cases have been reported. In these cases, the onset of symptoms typically occurred in childhood.
In addition to the above types of porphyria, there is a very rare type, called hepatoerythopoietic porphyria (HEP), that affects heme biosynthesis in both the liver and the bone marrow. HEP results from a defect in uroporphyrinogen decarboxylase activity (step 5), but strongly resembles congenital erythropoietic porphyria. Only 20 cases of HEP have been reported worldwide; it seems to be inherited in an autosomal recessive manner.
Causes and symptoms
General characteristics
The underlying cause of all porphyrias is a defective enzyme somewhere along the heme biosynthesis pathway. In virtually all cases, the defective enzyme is a genetically linked factor. Therefore, porphyrias are inheritable conditions. However, an environmental trigger-such as diet, drugs, or sun exposure-may be necessary before any symptoms develop. In many cases, symptoms do not develop, and individuals may be completely unaware that they have a gene for porphyria.
All of the hepatic porphyrias-except porphyria cutanea tarda-follow a pattern of acute attacks interspersed with periods of complete symptom remission. For this reason, they are often referred to as the acute porphyrias. The erythropoietic porphyrias and porphyria cutanea tarda do not follow the same pattern and are considered chronic conditions.
The specific symptoms of each porphyria depend on the affected enzyme and whether it occurs in the liver or in the bone marrow. The severity of symptoms can vary widely, even within the same porphyria type. When the porphyria becomes symptomatic, the common factor between all types is an abnormal accumulation of protoporphyrins or porphyrin.
ALA dehydratase porphyria (ADP)
ADP is characterized by a deficiency of ALA dehydratase. Of the few cases on record, the prominent symptoms were vomiting; pain in the abdomen, arms, and legs; and neuropathy. (Neuropathy refers to nerve damage that can cause pain, numbness, or paralysis.) As a result of neuropathy, the arms and legs may be weak or paralyzed and breathing can be impaired.
Acute intermittent porphyria (AIP)
AIP is caused by a deficiency in porphobilogen deaminase, but symptoms usually do not occur unless an individual with the deficiency encounters a biological trigger. Triggers can include hormones (for example oral contraceptives, menstruation, pregnancy), drugs, and dietary factors. However, most people with the deficiency never develop symptoms.
Attacks occur after puberty and commonly feature severe abdominal pain, nausea and vomiting, and constipation. Muscle weakness and pain in the back, arms, and legs are also typical symptoms. During an attack, the urine takes on a deep reddish color. The central nervous system may also be involved, as demonstrated by hallucinations, confusion, seizures, and mood changes.
Congenital erythropoietic porphyria (CEP)
CEP arises from a deficiency in uroporphyrinogen III cosynthase. Symptoms are often apparent in infancy and include reddish urine and possibly an enlarged spleen. The skin is unusually sensitive to light and blisters easily if exposed to sunlight. (Sunlight induces changes in protoporphyrins in the plasma and skin. These altered molecules can damage the skin.) Increased hair growth is common. Damage from recurrent blistering and associated skin infections can be severe; in some cases facial features and fingers are lost to recurrent damage and infection. Deposits of protoporphyrins sometimes occur in the teeth and bones.
Porphyria cutanea tarda (PCT)
PCT is caused by deficient uroporphyrinogen decarboxylase; it may be an acquired or inherited condition. The acquired form usually does not appear until adulthood. The inherited form may appear in childhood, but often demonstrates no symptoms. Early symptoms include blistering on the hands, face, and arms following minor injuries or exposure to sunlight. Lightening or darkening of the skin may occur along with increased hair growth or loss of hair. Liver function is abnormal but the signs are mild.
Hepatoerythopoietic porphyria (HEP)
HEP is linked to a deficiency of uroporphyrinogen decarboxylase in both the liver and the bone marrow. The symptoms resemble those of CEP.
Hereditary coproporphyria (HCP)
HCP is similar to AIP, but the symptoms are typically milder; the disorder is caused by a deficiency in coproporphyrinogen oxidase. The greatest difference between HCP and AIP is that people with HCP may have some skin sensitivity to sunlight. However, extensive damage to the skin is rarely seen.
Variegate porphyria (VP)
VP is caused by deficient protoporphyrinogen oxidase, and, like AIP, symptoms only occur during attacks. Major symptoms of this type of porphyria involve neurologic problems and sensitivity to light. Areas of the skin that are exposed to sunlight are susceptible to burning, blistering, and scarring.
Erythropoietic protoporphyria (EPP)
Owing to deficient ferrochelatase, the last step in the heme biosynthesis pathway-the insertion of an iron atom into a porphyrin molecule-cannot be completed. The major symptoms of this disorder are related to sensitivity to light-including both artificial and natural light sources. Following exposure to light, a patient with EPP experiences burning, itching, swelling, and reddening of the skin. Blistering and scarring may occur but are neither common nor severe. EPP may result in the formation of gallstones as well as liver complications. Symptoms can appear in childhood and tend to be more severe during the summer when exposure to sunlight is more likely.
Diagnosis
Depending on the array of symptoms presented, the possibility of porphyria may not immediately come to the physician's mind. In the absence of a family history of porphyria, some symptoms of porphyria, such as abdominal pain and vomiting, may be attributed to other disorders. Neurological symptoms, including confusion and hallucinations, may lead to an initial suspicion of psychiatric illness rather than a physical disorder. Diagnosis may be aided in cases in which these symptoms appear in combination with neuropathy, sensitivity to sunlight, or other factors. Certain symptoms, such as urine the color of port wine, are hallmarks of porphyria.
A common initial test measures protoporphyrins in the urine. However, if skin sensitivity to light is a symptom, a blood plasma test is indicated. If these tests reveal abnormal levels of protoporphyrins, further tests are performed to measure heme precursor levels in the stool and in red blood cells. The presence and estimated quantity of porphyrin and protoporphyrins are easily detected in biological samples using spectrofluorometric testing. This procedure involves the use of a laboratory instrument called a spectrofluorometer, which directs light of a specific strength at a fluid sample. Certain molecules in the sample-such as heme precursors-absorb the light energy and fluoresce. When molecules fluoresce, they emit light at a different strength from the absorbed light. The fluorescence can be detected and quantified by the spectrofluorometer. Not all molecules fluoresce, but among those that do, the intensity and quality of the fluorescence is an identifying characteristic. Diagnostic laboratory work, including analysis of blood, urine and stool samples is performed by laboratory technologists.
Heme precursors in the blood, urine, or stool give some indication of the type of porphyria, but more detailed biochemical testing is required to determine their exact identity. Making this determination yields a strong indicator of which enzyme in the heme biosynthesis pathway is defective, which in turn allows a diagnosis of the particular type of porphyria.
Biochemical tests rely on the color, chemical properties, and other unique features of each heme precursor. For example, a screening test for acute intermittent porphyria (AIP) is the Watson-Schwartz test. In this test, a special dye is added to a urine sample. If one of two heme precursors-porphobilinogen or urobilinogen-is present, the sample turns pink or red. Further testing is necessary to determine whether the precursor is porphobilinogen or urobilinogen-only porphobilinogen is indicative of AIP.
Other biochemical tests rely on the fact that heme precursors become less water soluble (able to be dissolved in water) as they progress further through the heme biosynthesis pathway. For example, to determine whether the Watson-Schwartz urine test is positive for porphobilinogen or urobilinogen, a measure of chloroform is added to the test tube. Chloroform is a water-insoluble substance, and even after vigorous mixing, the water and chloroform separate into two distinct layers. Whether the chloroform layer or the water layer becomes pink indicates which heme precursor is present. Porphobilinogen tends to be water soluble, and urobilinogen is slightly water insoluble. Since like mixes with like, porphobilinogen mixes more readily in the water than chloroform; therefore, if the water layer is pink, an AIP diagnosis is probable.
As a final test, measuring specific enzymes and their activities may be done for some types of porphyrias; however, such tests are not done for screening purposes. Certain enzymes, such as porphobilinogen deaminase (the defective enzyme in AIP), can be easily extracted from red blood cells; however, other enzymes are less readily collected or tested. Basically, an enzyme test involves adding a measure of the enzyme to a test tube containing the precursor it is supposed to modify. Both the production of modified precursor and the rate at which it appears are measured in the laboratory. If a modified precursor is produced, the test indicates that the enzyme is doing its job. The rate at which the modified precursor is produced can be compared to a standard to measure the enzyme's efficiency.
Treatment
Treatment for porphyria revolves around avoiding acute attacks, limiting potential effects, and treating symptoms. However, treatment options vary depending on the type of porphyria that has been diagnosed. Given the rarity of ALA dehydratase porphyria (six reported cases), definitive treatment guidelines have not been developed.
Acute intermittent porphyria, hereditary coproporphyria, and variegate porphyria
Treatment for acute intermittent porphyria, hereditary coproporphyria, and variegate porphyria follows the same basic regime. A patient diagnosed with one of these porphyrias can prevent most attacks by avoiding precipitating factors, such as certain drugs that have been identified as triggers for acute porphyria attacks. Individuals must maintain adequate nutrition, particularly in respect to carbohydrates. In some cases, an attack can be stopped by increasing carbohydrate consumption or by receiving carbohydrates intravenously.
When an attack occurs, medical attention is needed. Pain is usually severe, and narcotic analgesics are the best option for relief. Phenothiazines can be used to counter nausea, vomiting, and anxiety; and chloral hydrate or diazepam is useful for sedation or to induce sleep. Intravenously administered hematin may be used to curtail an attack. This drug seems to work by signaling the heme biosynthesis pathway to slow production of precursors. Women, who tend to develop symptoms more frequently than men in response to hormonal fluctuations, may find hormone therapy that inhibits ovulation to be helpful.
Congenital erythropoietic porphyria
The key points of congenital erythropoietic porphyria treatment are avoiding exposure to sunlight and preventing trauma to and infections of the skin. Liberal use of sunscreens and taking beta-carotene supplements can provide some protection from sun-induced damage. Medical treatments such as removing the spleen or administering red blood cell transfusions can have short-term benefits, but do not offer a cure. Oral doses of activated charcoal may offer the potential of remission.
Porphyria cutanea tarda
As with other porphyrias, the first line of defense is the avoidance of precipitating factors, especially alcohol. Regular blood withdrawal is a proven therapy for pushing symptoms into remission. For patients who are anemic or cannot have blood drawn for other reasons, chloroquine therapy may be used.
Erythropoietic protoporphyria
Avoiding sunlight, using sunscreens, and taking beta-carotene supplements are typical treatment options for erythropoietic protoporphyria. The drug cholestyramine may reduce the skin's sensitivity to sunlight as well as the accumulated heme precursors in the liver. Liver transplantation has been used in cases of liver failure, but it has not effected a long-term cure of the porphyria.
Prognosis
Even in the presence of a genetic inheritance for a porphyria, symptom development depends on a variety of factors. In the majority of cases, an individual remains asymptomatic throughout life. Porphyria symptoms are rarely fatal with proper medical treatment, but they may be associated with temporarily debilitating or permanently disfiguring consequences. Measures to avoid these consequences are not always successful, regardless of how diligently they are pursued. Although pregnancy has been known to trigger porphyria attacks, it is not as great a danger as was once thought.
Health care team roles
Patients diagnosed with porphyrias are cared for by an interdisciplinary treatment team that may include primary care physicians, hematologists, and dermatologists. Laboratory technologists are involved during the diagnostic process, and nurses, health educators, and genetic counselors provide instruction about how to recognize triggers and prevent attacks or flares of the condition.
Prevention
For the most part, the porphyrias are attributable to inherited genes; such an inheritance cannot be prevented. However, symptoms can be prevented or limited by avoiding factors that trigger development.
When there is a family history of porphyria, individuals should consider testing to determine whether they carry the associated gene. Even if symptoms are absent, it is useful to know about the presence of the gene to assess the risks of developing the associated porphyria. This knowledge also reveals whether the individual's offspring may be at risk. Theoretically, it is possible to perform prenatal tests. However, these tests would not indicate whether the child would develop porphyria symptoms; only that they might have the genetic predisposition to develop symptoms.
Key Terms
- Autosomal dominant
- An inheritance pattern in which a trait is determined by one gene in a pair (genes are inherited in pairs; one copy from each parent).
- Autosomal recessive
- An inheritance pattern in which a trait is expressed only if both genes in a pair code for that particular characteristic (genes are inherited in pairs; one copy from each parent).
- Enzyme
- A protein molecule that catalyzes a chemical reaction.
- Erythropoiesis
- The process through which new red blood cells are created; it begins in the bone marrow.
- Erythropoietic
- Referring to the creation of new red blood cells.
- Gene
- A portion of DNA (deoxyribonucleic acid) that codes for a specific product, such as an enzyme.
- Hematin
- A drug that is administered intravenously to halt an acute porphyria attack. It inhibits heme biosynthesis, preventing the further accumulation of heme precursors.
- Heme
- A large complex molecule contained in hemoglobin and a number of important enzymes throughout the body. Through these factors, it plays a vital role in metabolism and oxygen and energy transport. Heme is composed of porphyrin and an iron atom.
- Hemoglobin
- A molecule composed of heme and protein that enables red blood cells to transport oxygen throughout the body. Hemoglobin gives red blood cells their characteristic color.
- Hepatic
- Referring to the liver.
- Neuropathy
- A condition characterized by nerve damage. Major symptoms can include weakness, numbness, paralysis, or pain in the affected area.
- Porphyrin
- A large molecule shaped somewhat like a four-leaf clover. Combined with an iron atom, it forms a heme molecule.
- Protoporphyrin
- A precursor molecule to the porphyrin molecule.