The effectiveness of highly active antiretroviral therapy regimens has changed the natural history of human immunodeficiency virus (HIV) infection. (1,2) HIV-related deaths and opportunistic infections have decreased dramatically, and health care providers are focusing on management of increasingly complex drug regimens and their associated interactions and toxicities. (1-3)
Advisory panels recommend that experts care for HIV-infected patients. (4,5) However, as the population of survivors living with acquired immunodeficiency syndrome (AIDS) increases and most of their health care delivery shifts from the inpatient to the outpatient arena, family physicians are likely to be confronted by an increasing array of HIV-related health issues, such as side effects of antiretroviral medications, drug interactions, and patient adherence to treatment regimens. (1,6)
Side Effects of Antiretroviral Drugs
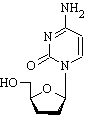
Antiretroviral drugs used in HIV management fall into three major classes: nucleoside reverse transcriptase inhibitors (NRTIs), nonnucleoside reverse transcriptase inhibitors (NNRTIs), and protease inhibitors (PIs). A nucleotide reverse transcriptase inhibitor (NtRTI), tenofovir (Viread), and a newly approved fusion inhibitor, enfuvirtide (Fuzeon), also are available. The protease inhibitors have the most side effects and strictest dosing regimens. Tables 1 through 4 (7-11) summarize the properties of antiviral drugs currently approved for treatment of HIV infection.
The U.S. Food and Drug Administration recently approved three new drugs for treatment of HIV infection. Enfuvirtide represents the first new class of drug approved for HIV treatment in seven years. It works by a different mechanism than all previous classes, inhibiting the fusion of HIV-1 with CD4+ T lymphocytes. (12) The production process is far more complicated than that of other antiretrovirals, making the wholesale cost of the drug approximately $20,000 per patient per year. (12) Enfuvirtide is approved only for use in patients with drug-resistant HIV infection.
The second new drug, atazanavir (Reyataz), is the first once-daily protease inhibitor. It may have little to no adverse impact on serum lipid levels and possibly none on lipodystrophy. (13,14)
Emtricitabine (Emtriva) is an NRTI that was approved for treatment of HIV infection in July 2003.15 As with atazanavir, its once-daily dosing regimen may increase compliance.
METABOLIC EFFECTS
Abnormal accumulation of body fat with truncal gain and peripheral loss; insulin resistance; and elevated cholesterol, triglyceride, and glucose levels can occur with the use of PIs. Retrospective analyses have offered conflicting evidence about whether antiretroviral agents increase the risk of coronary artery disease. (16,17) When intervention is indicated, a lipid-management program emphasizing dietary adjustments should be implemented. Because of the potential for substantial toxicity, the dosages of antihyperlipidemic agents should be reduced when they are taken with PIs.
Ritonavir (Norvir) increases serum levels of simvastatin (Zocor) and can cause myalgias, rhabdomyolysis, renal failure, and liver damage. PIs should not be used concurrently with simvastatin or lovastatin (Mevacor); pravastatin (Pravachol) is the safest statin to use with PIs. (7) Because of the potential for enhanced statin-related toxicity, atorvastatin (Lipitor) and fluvastatin (Lescol) should be used with caution and in lower dosages when taken with PIs. (7)
Serum lipid abnormalities have resolved in some patients after discontinuing PI therapy and starting PI-sparing regimens. (1) However, this step requires a risk-benefit analysis in consultation with an infectious disease or HIV specialist.
Monitoring fasting glucose levels every three to six months is useful in patients taking PIs because of the potential for developing glucose intolerance, insulin resistance, and type 2 diabetes. PIs can aggravate existing diabetes; patients with HIV infection who also have diabetes should be monitored closely when PIs are prescribed. (1) Diet, exercise, and weight loss are preferred over hypoglycemic drug therapy, although agents such as thiazolidinediones or metformin (Glucophage) can be considered. (1)
HEPATIC/GASTROINTESTINAL EFFECTS
Severe hepatotoxicity (i.e., more than a fivefold increase from the upper limit of normal in alanine transaminase or aspartate transaminase levels) can occur in patients treated with PIs (especially if they are taken in combination with other PIs such as saquinavir [Fortovase] and ritonavir) and some NRTIs and NNRTIs such as nevirapine (Viramune) and zalcitabine (Hivid). (1,18) Co-infection with hepatitis C virus is a major risk factor for developing hepatotoxicity after initiation of PI therapy. (19,20)
Lactic acidosis has been associated with NRTI and NNRTI use; although uncommon, it has a high mortality rate. (21,22) Patients taking NRTIs may present with nonspecific gastrointestinal symptoms, diarrhea, and anorexia, with or without abnormal test results such as elevated levels of hepatic transaminases and serum lactate. (23-25) Conversely, liver-function test results and lactate levels may be elevated in asymptomatic patients. (23,24)
The prodromal stage of lactic acidosis may include unexplained onset and persistence of abdominal distention and pain, nausea, vomiting, diarrhea, anorexia, dyspnea, generalized weakness, ascending neuromuscular weakness, myalgias, paresthesias, weight loss, and hepatomegaly. (26) Laboratory evaluation may reveal hyperlactacidemia and an increased anion gap and creatine kinase, lactate dehydrogenase, C-reactive protein, lipase, and amylase levels. (1,7,25,27) Computed tomography or ultrasonography may reveal an enlarged, fatty liver.
Other risk factors for lactic acidosis include female gender, obesity, and prolonged use of NRTIs. Pregnant women taking stavudine (Zerit) or didanosine (Videx) may be at especially high risk,1 although some cases of lactic acidosis have occurred in patients without any known risk factors. (24-26) Early recognition of lactic acidosis is vital so that the NRTI therapy can be stopped. (1,7)
DERMATOLOGIC EFFECTS
The HIV virus itself, co-infections (e.g., syphilis), infestations, and drug reactions can cause rashes in HIV-infected patients. Some HIV-associated dermatoses, including viral exanthem, herpes zoster, early molluscum contagiosum, seborrheic dermatitis, eosinophilic folliculitis, and "itchy red bump" disease, can be difficult to distinguish from drug-related effects.
Rashes can be mild and self-limiting or life-threatening, such as a hypersensitivity reaction to abacavir (Ziagen). Skin rashes occur most commonly with the use of NNRTIs1; they are more frequent and severe when associated with nevirapine therapy. (27) In one study, (27) 15 of 18 patients taking nevirapine had serious cutaneous manifestations such as Stevens-Johnson syndrome and toxic epidermal necrolysis. The mean time from the start of nevirapine therapy to the onset of rash was 11 days, with two thirds of the cases occurring during the first two weeks of therapy. Compared with men, women had a nearly sevenfold higher risk for developing grade 3 or 4 skin rashes. (28,29)
A two-week lead-in dose escalation schedule reduces the incidence of rash in patients who are starting nevirapine therapy. (30) Prophylactic use of systemic corticosteroids or antihistamines has not been proved uniformly effective. (29,30) However, some experts recommend antihistamine therapy for mild to moderate hypersensitivity reactions. (1) Switching to a different NNRTI in patients with a history of mild to moderate drug-associated skin rash is not recommended by most experts and should be done only with close follow-up. (1,7,30) [Reference 1--Evidence level C, consensus/ expert guidelines]
Among the NRTIs and PIs, abacavir and amprenavir (Agenerase) are associated most frequently with skin rash. (1,7,30) Abacavir can cause a severe hypersensitivity syndrome with rash, fever, malaise, and gastrointestinal symptoms. Respiratory manifestations such as pharyngitis, cough, and dyspnea also may occur but are less common. (1,30,31) Patients who become sensitized to abacavir risk hypotension and a life-threatening reaction if they try to use it again. Cases of abacavir hypersensitivity syndrome should be reported to the Abacavir Hypersensitivity Registry (telephone: 800-270-0425).
ORTHOPEDIC EFFECTS
Avascular necrosis and decreased bone density have been reported in patients with HIV infection. (30,32,33) Avascular necrosis may not be associated with a specific antiretroviral regimen, but it has been linked to corticosteroid use in some patients. (33,34) Other factors associated with osteonecrosis include alcohol abuse, hemoglobinopathies, hyperlipidemia, and previous use of antihyperlipidemics. (33) One prospective study (33) found that no single test or combination of tests, including physical examination and plain-film radiography, was predictive of osteonecrosis. However, at the time of magnetic resonance imaging, patients with osteonecrosis also were found to have significantly higher viral loads and platelet counts, and 93 percent had positive anticardiolipin antibodies. (33)
Studies of bone demineralization in a limited number of patients taking antiretroviral therapy have shown that up to 50 percent of patients on a PI-based regimen developed evidence of osteopenia compared with 20 percent of untreated patients and patients on a non-PI-based regimen. (35) Other studies have shown that patients with lipodystrophy and extensive prior PI use had osteopenia (28 percent) or osteoporosis (9 percent). (30)
Interactions
DRUG-FOOD INTERACTIONS
If antiretroviral drugs are not taken correctly with respect to meals and other medications, a reduction of as much as 80 percent in bioavailability is possible. (7,30) Fortunately, an increasing number of antiretroviral drugs have no specific food requirements (Tables 2 through 4). (7-11)
A full meal can reduce serum concentration of indinavir (Crixivan) by up to 80 percent; unlike other PIs such as saquinavir, nelfinavir (Viracept), and ritonavir, this agent should be taken on an empty stomach. Conversely, meals reduce the gastrointestinal side effects and increase the absorption of ritonavir and saquinavir.
Patients taking indinavir or lopinavir/ritonavir (Kaletra) should drink 150 mL (5.1 oz) of water per hour for three hours after each dose. Indinavir can cause interstitial nephritis and renal calcinosis; patients taking this drug should drink at least 1.5 L (50.7 oz) of water per day.
DRUG-DRUG INTERACTIONS
Drug-drug interactions are more common and potentially more severe with PIs than other classes of antiretroviral agents. Many of the drug interactions involving these agents can cause life-threatening reactions or reduced bioavailability of the PI. Even a short exposure to suboptimal levels of antiretroviral agents can lead to irreversible viral resistance and loss of clinical benefit (especially among drugs with a low barrier to resistance, such as lamivudine [Epivir] and NNRTIs). Therefore, knowledge of both types of interaction is extremely important. (1,7,30)
Because they stimulate the cytochrome P450 system, drugs such as phenytoin (Dilantin), rifampin (Rifadin), carbamazepine (Tegretol), phenobarbital, and dexamethasone--and even grapefruit juice--can cause a clinically significant increase in PI metabolism that can reduce serum drug concentrations. (21,30) By inhibiting the same isoform of the cytochrome P450 system that breaks down certain drugs, PIs--especially ritonavir--can increase serum levels of many drugs that are commonly prescribed in primary care. (1,7,30) These drugs should be avoided or used cautiously in patients with HIV infection.
Because they stimulate hepatic glucuronides, PIs can reduce serum concentrations of glucuronated drugs such as codeine and morphine. (1,7,30)
Ritonavir can decrease serum levels of ethinyl estradiol, sulfamethoxazole/trimethoprim (Bactrim, Septra), and zidovudine (Retrovir, formerly called azidothymidine [AZT]) to the point of clinical failure. (30,36) Providers should check product labels for the extensive listing of drug interactions before prescribing additional medications to patients who are taking PIs.
DRUG-HERB INTERACTIONS
In recent years, herbal medicine has grown faster than any other alternative treatment in the United States. (37) However, many patients may not consider herbal remedies to be "medicine" and might not think of telling their physicians that they are taking them. (38)
Garlic is the third leading herbal product in the United States, with total annual retail sales of $84 million. (37) Its reputation as a natural cholesterol fighter has made it popular among patients taking medications, such as PIs, that can increase lipid levels. However, garlic supplements have been shown to dramatically reduce serum concentrations of saquinavir by as much as 50 percent; levels remained lowered even after the patient stopped taking garlic. (39)
St. John's wort can influence serum levels of PIs and NNRTIs. (40,41) By stimulating cytochrome P450 activity, it can lower serum concentration of indinavir by up to 80 percent. (42)
Adherence to Therapy
Adherence to antiretroviral regimens is critical. (7,30) Patients must take 95 percent of their pills to achieve an 80 percent likelihood of HIV suppression below 50 copies per mL. With less than 95 percent adherence, the probability of suppression to undetectable levels drops to less than 50 percent. (43)
Patients must be committed to and capable of adhering to complicated regimens with high pill burdens; some regimens require more than 20 pills per day. Compared with other PI regimens, indinavir and lopinavir/ ritonavir require the fewest number of capsules per day.
To familiarize patients with the rigors of antiretroviral therapy, some centers offer "dry runs" with jellybeans before patients start their first regimen. This exercise has not been proved to improve adherence.
Failure to take medications regularly and reliably causes the virus to be exposed to suboptimal drug serum concentrations and drastically increases the chance that drug resistance will develop. The patient's relationship with the physician has been shown to be one of the greatest determinants of adherence. (43) Even in highly committed patients, adherence wanes over time. A phenomenon described as "pill fatigue" or "treatment fatigue" can occur. (1,7,30) Monitoring adherence at every clinical encounter is essential. Reasonable responses to decreasing adherence include increasing the intensity of clinical follow-up, shortening the follow-up interval, and recruiting additional health team members, depending on the nature of the problem (Table 5). (44)
Depression has been reported in more than one half of HIV-infected patients and in up to 60 percent of HIV-infected women. (4) Cessation of all medications at the same time may be more desirable than uncertain adherence during a short exacerbation of chronic depression.
TABLE 1
Antiretroviral Agents Used to Treat HIV Infection
Class: NRTI
Abacavir (Ziagen)
Abacavir/lamivudine/zidovudine (Trizivir)
Didanosine (Videx)
Emtricitabine (Emtriva)
Lamivudine (Epivir)
Lamivudine/zidovudine (Combivir)
Stavudine (Zerit)
Zalcitabine (Hivid)
Zidovudine (Retrovir)
Class: NtRTI
Tenofovir (Viread)
Class: NNRTI
Delavirdine (Rescriptor)
Efavirenz (Sustiva)
Nevirapine (Viramune)
Class: PI
Amprenavir (Agenerase)
Atazanavir (Reyataz)
Indinavir (Crixivan)
Lopinavir/ritonavir (Kaletra)
Nelfinavir (Viracept)
Ritonavir (Norvir)
Saquinavir (Fortovase) *
Saquinavir mesylate (Invirase) *
Class: FI
Enfuvirtide (Fuzeon)
HIV = human immunodeficiency virus; NRTI = nucleoside reverse transcriptase inhibitor; NtRTI = nucleotide reverse transcriptase inhibitor; NNRTI = nonnucleoside reverse transcriptase inhibitor; PI = protease inhibitor; FI = fusion inhibitor.
*--Saquinavir and saquinavir mesylate are not bioequivalent and are not interchangeable.
TABLE 5
Tips for Improving Adherence to Antiretroviral Regimens
Educate the patient about the goals of therapy and the importance of adherence to the regimen.
Anticipate and treat side effects.
Simplify food requirements.
Reduce dosage frequency and number of pills, if possible.
Recruit the patient's family and friends for support.
Provide a written dosing schedule, pictures of medications, daily or weekly pillboxes, alarm clocks, pagers, or other reminders.
Monitor adherence and intensify management in periods of low adherence.
Consider the impact of new diagnoses on adherence (e.g., depression, wasting, recurrent chemical dependency) and include adherence intervention in the management plan.
Use nurses, pharmacists, peer educators, volunteers, case managers, drug counselors, physician assistants, nurse practitioners, and research staff to reinforce adherence.
Information from reference 44.
The opinions and assertions contained herein are the views of the authors and are not to be construed as official or as reflecting the views of the U.S. Army Medical Department or the U.S. Army at large.
The authors thank Cathy Vickers, R.N., Daniel J. Schissel, M.D., and George W. Christopher, M.D., for review of the manuscript.
The authors indicate that they do not have any conflicts of interest. Sources of funding: none reported.
REFERENCES
(1.) Yeni PG, Hammer SM, Carpenter CC, Cooper DA, Fischl MA, Gatell JM, et al. Antiretroviral treatment for adult HIV infection in 2002: updated recommendations of the International AIDS Society-USA Panel. JAMA 2002;288:222-35.
(2.) Palella FJ Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med 1998; 338:853-60.
(3.) Trachtenberg JD, Sande MA. Emerging resistance to nonucleoside reverse transcriptase inhibitors: a warning and a challenge. JAMA 2002;288:239-41.
(4.) Levine AM. Evaluation and management of HIV-infected women. Ann Intern Med 2002;136:228-42.
(5.) Kitahata MM, Koepsell TD, Deyo RA, Maxwell CL, Dodge WT, Wagner EH. Physicians' experience with the acquired immunodeficiency syndrome as a factor in patients' survival. N Engl J Med 1996;334:701-6.
(6.) Gebo KA, Chaisson RE, Folkemer JG, Bartlett JG, Moore RD. Costs of HIV medical care in the era of highly active antiretroviral therapy. AIDS 1999; 13:963-9.
(7.) Guidelines for the use of antiretroviral agents in HIV-infected adults and adolescents. Accessed May 2003 at: www.cdc.gov/mmwr/preview/mmwrhtml/ 00054080.htm.
(8.) Emtriva [package insert]. Foster City, Ca.: Gilead Sciences, Inc., 2003. Accessed July 2003 at: www. emtriva.com.
(9.) Reyataz [package insert]. Princeton, N.J.: Bristol-Myers Squibb Co., 2003. Accessed July 2003 at: www.reyataz.com.
(10.) Fuzeon [package insert]. Nutley, N.J.: Roche Laboratories Inc., 2003. Accessed July 2003 at: www. rocheusa.com/products/fuzeon.
(11.) Enfuvirtide (Fuzeon) for HIV infection. Med Lett Drugs Ther 2003;45:49-50.
(12.) Steinbrook R. HIV infection--a new drug and new costs. N Engl J Med 2003;348:2171-2.
(13.) Haas DW, Zala C, Schrader S, Piliero P, Jaeger H, Nunes D, et al., for the Protocol AI424-009 Study Group. Therapy with atazanavir plus saquinavir in patients failing highly active antiretroviral therapy: a randomized comparative pilot trial. AIDS 2003; 17:1339-49.
(14.) FDA approves a once daily protease inhibitor for HIV infection. Retrieved July 2003 from: www.fda. gov/bbs/topics/ANSWERS/2003/ANS01233.html.
(15.) Emtriva approved. Retrieved July 2003 from: www.fda.gov/oashi/aids/new.html#emtriva.
(16.) Klein D, Hurley L, Sidney S. Do protease inhibitors increase the risk for coronary heart disease among HIV-positive patients? Additional follow-up. Accessed May 2003 at: www.retroconference.org/ 2000/abstracts/33.htm.
(17.) Coplan P, Cormier K, Japour A, Maradit-Kremers H, Nikas A, Lewis R, et al. Myocardial infarction incidence in clinical trials of 4 protease inhibitors. Accessed May 2003 at: www.retroconference.org/ 2000/abstracts/34.htm.
(18.) Sulkowski MS, Thomas DL, Chaisson RE, Moore RD. Hepatotoxicity associated with antiretroviral therapy in adults infected with human immunodeficiency virus and the role of hepatitis C or B virus infection. JAMA 2000;283:74-80.
(19.) Saves M, Raffi F, Clevenbergh P, Marchou B, Waldner-Combernoux A, Morlat P, et al. Hepatitis B or hepatitis C virus infection is a risk factor for severe hepatic cytolysis after initiation of a protease inhibitor-containing antiretroviral regimen in human immunodeficiency virus-infected patients. The APROCO Study Group. Antimicrob Agents Chemother 2000;44:3451-5.
(20.) Nunez M, Lana R, Mendoza JL, Martin-Carbonero L, Soriano V. Risk factors for severe hepatic injury after introduction of highly active antiretroviral therapy. J Acquir Immune Defic Syndr 2001;27: 426-31.
(21.) Fortgang IS, Belitsos PC, Chaisson RE, Moore RD. Hepatomegaly and steatosis in HIV-infected patients receiving nucleoside analog antiretroviral therapy. Am J Gastroenterol 1995;90:1433-6.
(22.) ter Hofstede HJ, de Marie S, Foudraine NA, Danner SA, Brinkman K. Clinical features and risk factors of lactic acidosis following long-term antiretroviral therapy: 4 fatal cases. Int J STD AIDS 2000;11:611-6.
(23.) John M, Moore CB, James IR, Nolan D, Upton RP, McKinnon EJ, et al. Chronic hyperlactatemia in HIV-infected patients taking antiretroviral therapy. AIDS 2001;15:717-23.
(24.) 3rd International Workshop on Salvage Therapy for HIV Infection. 12-14 April 2000, Chicago, Illinois. Report and abstracts. Antivir Ther 2000;5(suppl 2): 1-35.
(25.) Lonergan JT, Behling C, Pfander H, Hassanein TI, Mathews WC. Hyperlactatemia and hepatic abnormalities in 10 human immunodeficiency virus-infected patients receiving nucleoside analogue combination regimens. Clin Infect Dis 2000;31: 162-6.
(26.) Important drug warning--Zerit and Videx. Accessed May 2003 at: www.fda.gov/medwatch/ SAFETY/2001/Zerit&Videx_letter.htm.
(27.) Fagot JP, Mockenhaupt M, Bouwes-Bavnick JN, Naldi L, Viboud C, Roujeau JC. Nevirapine and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. AIDS 2001;15:1843-8.
(28.) Bersoff-Matcha SJ, Miller WC, Aberg JA, van Der Horst C, Hamrick HJ Jr, Powderly WG, et al. Sex differences in nevirapine rash. Clin Infect Dis 2001; 32:124-9.
(29.) Antinori A, Baldini F, Girardi E, Cingolani A, Zaccarelli M, Di Giambenedetto S, et al. Female sex and the use of anti-allergic agents increase the risk of developing cutaneous rash associated with nevirapine therapy. AIDS 2001;15:1579-81.
(30.) Dybul M, Fauci AS, Bartlett JG, Kaplan JE, Pau AK. Guidelines for using antiretroviral agents among HIV-infected adults and adolescents. Ann Intern Med 2002;137(5 pt 2):381-433.
(31.) Stephenson J. Scientists find some genes a bad omen for anti-HIV drug. JAMA 2002;287:1637.
(32.) Scribner AN, Trioa-Cancio PV, Cox BA, Marcantonio D, Hamid F, Keiser P, et al. Osteonecrosis in HIV: a case-control study. J Acquir Immune Defic Syndr 2000;25:19-25.
(33.) Miller KD, Masur H, Jones EC, Joe GO, Rick ME, Kelly GG, et al. High prevalence of osteonecrosis of the femoral head in HIV-infected adults. Ann Intern Med 2002;137:17-25.
(34.) Report and abstracts of the 2nd International Workshop on Adverse Drug Reactions and Lipodystrophy in HIV. 13-15 September 2000, Toronto, Canada. Antivir Ther 2000:5(suppl 5):1-86.
(35.) Tebas P, Powderly WG, Claxton S, Marin D, Tantisiriwat W, Teitelbaum SL, et al. Accelerated bone mineral loss in HIV-infected patients receiving potent antiretroviral therapy. AIDS 2000;14:F63-7.
(36.) Graziani AL. Drug interactions associated with HIV protease inhibitors. In: Rose BD, ed. UpToDate. Wellesley, Mass.: UpToDate, 2003.
(37.) Ernst E. The risk-benefit profile of commonly used herbal therapies: Ginkgo, St. John's Wort, Ginseng, Echinacea, Saw Palmetto, and Kava. Ann Intern Med 2002;136:42-53.
(38.) Torpy JM. Integrating complementary therapy into care. JAMA 2002;287:306-7.
(39.) Piscitelli SC, Burstein AH, Welden N, Gallicano KD, Falloon J. The effect of garlic supplements on the pharmacokinetics of saquinavir. Clin Infect Dis 2002;34:234-8.
(40.) James JS. St. John's wort warning: do not combine with protease inhibitors, NNRTIs. AIDS Treat News 2000;(337):3-5.
(41.) De Maat MM, Hoetelmans RM, Mathot RA, van Gorp EC, Meenhorst PL, Mulder JW, et al. Drug interaction between St John's wort and nevirapine. AIDS 2001;15:420-1.
(42.) Piscitelli SC, Burstein AH, Chaitt D, Alfaro RM, Falloon J. Indinavir concentrations and St. John's wort. Lancet 2000;355:547-8.
(43.) Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med 2000;133:21-30.
(44.) Sherer R. Adherence and antiretroviral therapy in injection drug users. JAMA 1998;280:567-8.
Richard W. Sloan, M.D., R.PH., coordinator of this series, is chairman of the Department of Family Medicine at York (Pa.) Hospital and clinical associate professor in family and community medicine at the Milton S. Hershey Medical Center, Pennsylvania State University, Hershey, Pa.
EMIL P. LESHO, LTC, MC, USA, is an infectious diseases fellow at the National Capital Consortium, Uniformed Services University of the Health Sciences, National Naval Medical Center, Bethesda, Md., and Walter Reed Army Medical Center, Washington D.C. Dr. Lesho received his medical degree from Philadelphia College of Osteopathic Medicine and completed an internal medicine residency at Madigan Army Medical Center, Tacoma, Wash.
DANIELA C. GEY, M.D., is a dermatology resident at the human immunodeficiency virus (HIV)/sexually transmitted disease clinic affiliated with the University of Heidelberg School of Medicine, Heidelberg, Germany, where she received her medical degree. She is an investigator in two international, multicenter studies of immune augmentation with interleukin-2 in patients with HIV and has participated in other research projects investigating experimental protease inhibitors.
Address correspondence to Emil P. Lesho, LTC, MC, USA, 611 Forest Glen Rd., Silver Spring, MD 20901 (e-mail: emillesho@yahoo.com). Reprints are not available from the authors.
COPYRIGHT 2003 American Academy of Family Physicians
COPYRIGHT 2003 Gale Group