To the Editor:
With great interest, I read the article by Kodama et al[1] (May 2000), which provided an important message concerning coronary vasospasm inducing subendocardial ischemia after intracoronary acetylcholine injection in patients with hypertrophic cardiomyopathy (HCM). The authors did not remark that intracoronary injection of acetylcholine is a standard stressor testing endothelium-dependent coronary vasomotor reactivity.[2] Accordingly, the coronary vasoconstrictor response to acetylcholine instead of normal vasodilatation is considered to be a marker of coronary endothelial dysfunction.[2] Thus, Kodama et al[1] demonstrated abnormal endothelium-dependent coronary vasomotor reactivity in some HCM patients, 'although this evident endothelial dysfunction was not discussed in the article. In our study,[3] asymptomatic and mildly symptomatic HCM patients had an abnormal vasoconstrictor response of the coronary artery to the cold pressor test (another stressor testing endothelium-dependent vasomotor reactivity). Verapamil treatment was able to reverse this vasoconstrictor response to vasodilation.[3] We studied changes in coronary blood flow velocity that reflect vasomotor response of coronary resistance vessels, while Kodama et al[1] assessed changes in the diameter of the coronary epicardial artery. Iida et al[4] measured both coronary artery diameter and flow changes after acetylcholine infusion, and they showed impairment of endothelium-dependent coronary vasodilation both at epicardial and resistance vessels.
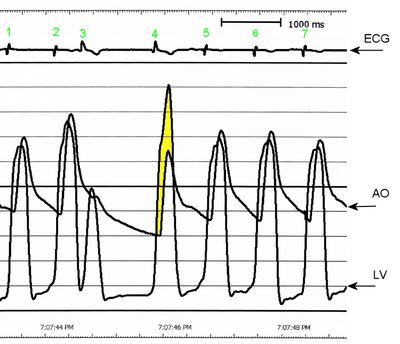
Kodama et al[1] showed depression rather than elevation of ST-segment as predominate abnormalities in ECG during acetylcholine injection, importantly, ischemic ST-segment depression may lead to life-threatening arrhythmia in patients with HCM.[5] Verapamil decreased or eliminated exercise-induced ischemia in young patients with a history of cardiac arrest or syncope.[5] At the follow-up, therapy for ischemia with verapamil was protective because only patients who temporally discontinued verapamil treatment had further unfavorable events.[5]
Taking into account the above-mentioned findings, an important question to the authors arises, as to whether treatment with calcium antagonists (especially verapamil) is able to prevent episodes of vasospastic angina. According to the data in the article, the majority of HCM patients (9 of 12) had chest pain that developed at midnight or early in the morning. Had these patients been treated with calcium antagonists previously? Another question regards data from a possible follow-up. Did anginal attacks recur even with treatment with calcium antagonists, or did any unfavorable events occur in the follow-up? In previous study,[6] the ECG signs of myocardial ischemia elicited by stressor-tested endothelium-independent coronary vasomotion identified HCM patients at higher risk of cardiac events. Thus, the prognostic value of an abnormal endothelium-dependent coronary vasomotor response seems desirable to determine.
Pawel Petkow Dimitrow, MD Collegium Medicum Jagiellonian University Cracow, Poland
Pawel Petkow Dimitrow, MD, 2nd Department of Cardiology, Collegium Medicum Jagiellonian University, Cracow, Poland 31-501; e-mail: dimitrow@mp.pl
REFERENCES
[1] Kodama K, Shigematsu Y, Hamada M, et al. The effect of coronary vasospasm on the direction of ST-segment deviation in patients with both hypertrophic cardiomyopathy and vasospastic angina. Chest 2000; 117:1300-1308
[2] Ludmer PL, Selwyn AP, Shook TL, et al. Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N Engl J Med 1986; 315:1046-1051
[3] Dimitrow PP, Krzanowski M, Nizankowski R, et al. Verapamil improves of coronary vasomotion to cold pressor test in asymptomatic and mildly symptomatic patients with hypertrophic cardiomyopathy. Cardiovasc Drug Ther 1999; 13: 259-264
[4] Iida H, Fujii T, Miura T, et al. Assessment of endothelium dependent coronary vasodilatation in hypertrophic cardiomyopathy [abstract]. Circulation 1996; 94:I-502
[5] Dilsizian V, Bonow RO, Epstein SE, et al. Myocardial ischemia detected by thallium scintigraphy is frequently related to cardiac arrest and syncope in young patients with hypertrophic cardiomyopathy, J Am Coll Cardiol 1993; 22: 796-804
[6] Lazzeroni E, Picano E, Morozzi L, et al. Dipyridamole-induced ischemia as prognostic marker of future adverse cardiac events in adult patients with hypertrophic cardiomyopathy. Circulation 1997; 96:4268-4272
To the Editor:
We appreciate the opportunity to respond to the comments of Dr. Dimitrow regarding our recent article (May 2000),[1] in which we compared the direction of the ST-segment shift during anginal attacks induced by intracoronary injection of acetylcholine in 12 patients with both hypertrophic cardiomyopathy (HCM) and vasospastic angina (VSA) with that in 28 patients with VSA alone. Acetylcholine-inducible vasospasm leads to anginal attacks associated with ST-segment elevation, which usually shows a transmural injury pattern on the ECG, less frequently in patients with both HCM and VSA than in those with VSA alone.
The effects of intracoronary acetylcholine injection on human coronary arteries are very complex.[2-5] Acetylcholine has two potentially opposing effects: vasodilatation mediated by the release of endothelium-derived relaxing factor, and vasoconstriction by direct stimulation of vascular smooth muscle. The net coronary vasomotor response, either vasodilatation or vasoconstriction, depends on the balance between these two effects. In normal coronary arteries with a functionally intact endothelium, acetylcholine administration at a low concentration will induce vasodilatation, because endothelial stimulation occurs at acetylcholine concentrations lower than those required to produce contraction of smooth muscle. Acetylcholine causes vasoconstriction at higher concentrations because endothelium-dependent vasodilatation can no longer oppose the direct vasoconstrictor effect. In diseased coronary arteries with dysfunctional endothelium, on the other hand, intracoronary administration of acetylcholine is expected to induce vasoconstriction even at lower concentrations. Heterogeneity in the response of coronary arteries to acetylcholine with regard to coronary segments is also shown. For example, acetylcholine could have differing effects on proximal and distal segments of the same coronary artery branch, such as epicardial conduit and resistance vessels. However, vasoconstriction does not equal vasospasm. As stressed by Maseri et al,[6] coronary vasoconstriction in which total occlusion or subtotal occlusion with delayed distal filling of contrast material in response to vasoactive agents is documented by coronary angiography is defined as epicardial coronary artery spasm. Inducible coronary vasospasm often develops the pathophysiologic consequences of myocardial ischemia, that is, chest pain and ECG changes such as ST-segment deviation. Physiologic (mild-to-moderate) vasoconstriction and even severe vasoconstriction without associated myocardial ischemia are all merely vasoconstriction, not vasospasm.
In our article,[1] we used the strict definition of acetylcholine-inducible vasospasm. In short, we considered that coronary vasospasm occurred when angiography revealed severe vasoconstriction of grade 0 to 2 flow (determined using the classification of the Thrombolysis in Myocardial Infarction trial[7]) in the epicardial coronary arteries associated with angina and/or ischemic ECG changes after intracoronary injection of acetylcholine. Thus, we think that nearly all the HCM patients studied definitely had VSA, although some patients without VSA might be included, as neither the specificity nor the sensitivity of the acetylcholine tests for detecting coronary vasospasm is 100%. Certainly, we performed provocative tests for coronary vasospasm, using a relatively high concentration of acetylcholine.[3,4,8] However, acetylcholine at the same dose would be unlikely to cause coronary vasospasm in patients without pathologic vasomotor tone of the coronary arteries. Hodgson and Marshall[2] demonstrated that the percentage reduction in the cross-sectional area of the epicardial coronary artery was up to 75% in 64 patients without VSA after intracoronary bolus injection of 100 [micro]g of acetylcholine, which is the maximum dose that we used. On the other hand, we previously reported that most HCM patients without VSA have various degrees of vasoconstriction in response to intracoronary injection of acetylcholine.[9] Approximately 42% (11 of 26) of those patients had chest pain or ECG changes suggestive of myocardial ischemia during the inducible vasoconstriction. This might represent the fact that in patients with HCM, myocardial ischemia results from even lesser degrees of coronary vasoconstriction of the large epicardial coronary arteries when there is endothelial dysfunction.[10] Moreover, functional abnormalities at the level of the coronary microvasculature leading to myocardial ischemia might be present, although we did not measure coronary blood flow.[9] However, the mean [+ or -] SD age of 26 patients was relatively high (61 [+ or -] 11 years), and 69% (18 of 26) of those patients had one or more risk factors for coronary artery disease that would be expected to cause endothelial dysfunction, such as cigarette smoking, hypertension, hypercholesterolemia, or diabetes mellitus. It has been demonstrated that coronary risk factors, including advanced age, are closely associated with abnormal endothelial function, even in patients with "normal" findings on coronary arteriography.[3] Thus, we cannot conclude from our two studies[1,9] that this dysfunction is an abnormality intrinsic to coronary artery system in HCM patients.
Of the 12 patients with HCM and VSA who we studied,[1] 9 patients had chest pain typical of angina pectoris and another patient had atypical angina. The remaining two patients did not have chest pain. After cardiac catheterization, including provocative tests for coronary vasospasm using acetylcholine, all but one patient without chest pain were treated with calcium antagonists (diltiazem, four patients; amlodipine, three patients; verapamil, two patients; and nisoldipine, one patient), although treatment was withheld in one of these patients (receiving nisoldipine) because of hypotension. In addition, two patients with typical angina were given the potassium channel opener nicorandil and long-acting nitrates, because their anginal attacks did not subside with calcium antagonists alone. A third patient was treated with both a calcium channel blocker and a long-acting nitrate for the same reason. The one patient who had no angina and did not receive calcium antagonists took the class Ia antiarrhythmic drug cibenzoline because of paroxysmal atrial fibrillation. Ultimately, this patient was given the calcium antagonist (nilvadipine) because of hypertension. Cibenzoline was given to another patient in order to prevent paroxysmal atrial fibrillation and to a third patient in whom nonobstructive HCM converted to obstructive HCM during follow-up.[11] The latter patient received a [Beta]-adrenergic blocking agent (metoprolol) in addition to a calcium antagonist (amlodipine) and cibenzoline. [Beta]-Blockers were given to three other patients (bisoprolol, two patients; propranolol, one patient) who had palpitations or dyspnea on effort, although the [Beta]-blocker (propranolol) was discontinued in one patient because of recurrent anginal attacks. After treatment, the occurrence of chest pain decreased markedly in 10 patients with typical or atypical angina, and did not appear in 2 patients who had no chest pain. During the follow-up period (mean, 61 [+ or -] 24 months), two patients died. One patient who did not have angina but had several episodes of paroxysmal atrial fibrillation died suddenly; and the remaining patient, who had typical angina, died of colon cancer. An autopsy was not performed for either patient.
Koji Kodama - Takahashi, MD Yawatahama General Hospital Ehime, Japan Yuji Shigematsu, MD Mareomi Hamada, MD Kunio Hiwada, MD Ehime University School of Medicine Ehime, Japan Yukio Kazatani, MD Ehime Prefectural Central Hospital Ehime, Japan Keisuke Matsuzaki, MD Eiki Murakami, MD Kinki Central Hospital Hyogo, Japan
Correspondence to: Koji Kodama-Takahashi, MD, The Department of Internal Medicine, Yawatahama General Hospital, 1-638 Ohira, Yawatahama-shi, Ehime 796-8502, Japan; e-mail: koji0911@sage.ocn.ne.jp
REFERENCES
[1] Kodama K, Shigematsu Y, Hamada M, et al. The effect of coronary vasospasm on the direction of ST-segment deviation in patients with both hypertrophic cardiomyopathy and vasospastic angina. Chest 2000; 117:1300-1308
[2] Hodgson JM, Marshall JJ. Direct vasoconstriction and endothelium-dependent vasodilatation: mechanisms of acetylcholine effects on coronary flow and arterial diameter in patients with nonstenotic coronary arteries. Circulation 1989; 79: 1043-1051
[3] Vita JA, Treasure CB, Nabel EG, et al. Coronary vasomotor response to acetylcholine relates to risk factors for coronary artery disease. Circulation 1990; 81:491-497
[4] Zeiher AM, Drexler H, Saurbier B, et al. Endothelium-mediated coronary blood flow modulation in humans: effects of age, atherosclerosis, hypercholesterolemia, and hypertension. J Clin Invest 1993; 92:652-662
[5] El-Tamimi H, Mansour M, Wargovich TJ, et al. Constrictor and dilator responses to intracoronary acetylcholine in adjacent segments of the same coronary artery in patients with coronary artery disease: endothelial function revisited. Circulation 1994; 89:45-51
[6] Maseri A, Davies G, Hackett D, et al. Coronary artery spasm and vasoconstriction: the case for distinction. Circulation 1990; 81:1983-1991
[7] The TIMI Study Group. The Thrombolysis in Myocardial Infarction (TIMI) trial: phase 1 findings. N Engl J Med 1985; 312:932-936
[8] Yasue H, Matsuyama K, Matsuyama K, et al. Responses of angiographically normal human coronary arteries to intracoronary injection of acetylcholine by age and segment: possible role of early coronary atherosclerosis. Circulation 1990; 81:482-490
[9] Kodama K, Hamada M, Kazatani Y, et al. Clinical characteristics in Japanese patients with coexistent hypertrophic cardiomyopathy and coronary vasospasm. Angiology 1998; 49: 849-855
[10] Dimitrow PP, Krzanowski M, Nizankowski R, et al. Verapamil improves the response of coronary vasomotion to cold pressor test in asymptomatic and mildly symptomatic patients with hypertrophic cardiomyopathy. Cardiovasc Drugs Ther 1999; 13:259-264
[11] Hamada M, Shigematsu Y, Ikeda S, et al. Class Ia antiarrhythmic drug cibenzoline: a new approach to the medical treatment of hypertrophic obstructive cardiomyopathy. Circulation 1997; 96:1520-1524
COPYRIGHT 2001 American College of Chest Physicians
COPYRIGHT 2001 Gale Group