Rationale: Oxidative stress may increase the risk of asthma, contribute to asthma progression, and decrease lung function. Previous research suggests that use of acetaminophen, which is hypothesized to reduce antioxidant capacity in the lung, is associated with an increased risk of asthma. We hypothesized that acetaminophen use may also be associated with chronic obstructive pulmonary disease (COPD) and decreased lung function. Objectives: To investigate the associations between use of pain medication, particularly acetaminophen, and asthma, COPD, and FEV^sub 1^ in adults. Methods: A cross-sectional analysis using the Third National Health and Nutrition Examination Survey. Measurement and Main Results: Increased use of acetaminophen had a positive, dose-dependent association with COPD (adjusted odds ratio for increasing category of intake, 1.16; 95% confidence interval [CI], 1.09-1.24; p value for trend
Keywords: acetaminophen; asthma; COPD; FEV^sub 1^
Over recent decades, there has been an increase in asthma and other respiratory diseases, and the reasons for these increases are not fully understood (1, 2). Oxidative stress appears to play an important role in the development and progression of these diseases: this hypothesis is supported by studies showing that individuals with a diet high in antioxidants are less likely to develop asthma and have higher lung function (3-6). One endogenous antioxidant, glutathione, is found in high concentrations in the airway epithelial lining fluid (7), and evidence suggests that decreased glutathione levels are associated with oxidant damage in the lung (8, 9). In addition to its antioxidant properties, glutathione plays a role in drug detoxification, particularly in the metabolism of acetaminophen (10). Animal studies have demonstrated that high doses of acetaminophen reduce levels of glutathione in lung tissue (11, 12). Therefore, regular users of acetaminophen may, through depletion of glutathione, be at an increased risk of lung tissue damage and ultimately of respiratory disease.
Epidemiologic evidence from both cross-sectional (13, 14) and longitudinal (15, 16) studies demonstrates an association between increased use of acetaminophen and an increased risk of asthma in both children and adults. However, no prior studies have considered the effects of acetaminophen on other respiratory diseases or on lung function. We have therefore examined the relation between use of simple analgesics and prevalence of obstructive airways diseases, where the pathophysiology may comprise effects mediated through oxidative stress/and or inflammatory pathways. We hypothesized that acetaminophen use is associated with an increased risk of chronic obstructive pulmonary disease (COPD), and with lower lung function, and that these effects are independent of any effects demonstrated for asthma. Thus, we investigated the relation between use of analgesics and prevalence of COPD, asthma, and level of lung function in adults.
METHODS
This research was conducted using data from the Third National Health and Nutrition Examination Survey (NHANES III), which is a cross-sectional survey of the U.S. noninstitutionalized population conducted between 1988 and 1994. Full details of the examination and survey procedures are published by the National Center for Health Statistics (17). Included in this analysis are all participants aged between 20 and 80 years, with complete data for relevant exposures, outcomes, and confounding factors.
Data Collection
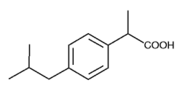
Questionnaire data were collected by trained interviewers who gathered information on race/ethnicity, medical history, socioeconomic status, use of medication, and smoking history. Participants were also asked whether they had taken any of the following pain medications in the last month and, if so, how often they had used each: aspirin (including Anacin, Bufferin, Ecotrin, Ascriptin, or Midol), acetaminophen (including Tylenol, Anacin-3), and ibuprofen (including Advil, Nuprin, Medipren). Participants attended a mobile examination unit where all physical measurements were taken, including height and weight. Lung function tests were completed, providing data on FEV^sub 1^ and FVC. Skin-prick testing using the prick-puncture technique was performed with 10 allergens. Detailed methods for these assessments are included in an online supplement and are published elsewhere (17).
Statistical Analyses
Using self-reported smoking history, participants were classified as never smokers, ex-smokers, and current smokers, and lifetime cigarette consumption was quantified in pack-years. Before analyses, analgesic use was arbitrarily divided into categories comprising never users, occasional users (1-5 times in the past month), regular users (6-29 times in the past month), and daily users (> 29 times in the past month). Asthma was defined as self-report of ever having physician-diagnosed asthma. COPD was defined as self-reported physician-diagnosed emphysema and/or chronic bronchitis, or by Global Initiative for Chronic Obstructive Lung Disease spirometry criteria (FEV^sub 1^/FVC
The association between use of analgesics and lung disease or allergic sensitization was analyzed using multiple logistic regression, with analgesics initially modeled as set of categoric variables, and then as a trend using a single, ordered categoric variable, where appropriate. To explore effects from possible overlap in the diagnoses of asthma and COPD, analyses were repeated after eliminating participants with one or the other respiratory diagnosis, and with both diagnoses. We sought to establish whether any association of asthma with acetaminophen use was from systematic avoidance of nonsteroidal antiinflammatory drugs, particularly aspirin, by examining the dose-response effect of acetaminophen in those who used and did not use aspirin.
The relation between use of analgesics in the last month and FEV^sub 1^, adjusted for age, sex, height, smoking (status and pack-years), and race/ethnicity, was explored using linear regression. Analyses were also conducted excluding participants with asthma.
All regression analyses were investigated for possible interactions between exposure and confounding factors, particularly sex, age, smoking, and antioxidant intake. Because of the complex, multistage probability sample design of NHANES III, estimates were calculated accounting for the survey design, using the specialized survey command within Stata SE 8.0 (Stata Corporation, College Station, TX). Further details on the methods are located in the online supplement.
RESULTS
The demographics and other characteristics were similar in subjects included in the study compared with those excluded because of missing data, with the exception that excluded participants were slightly older (Table 1). Among study participants, the prevalence of asthma and COPD were 6.9 and 11.8%, respectively, and 2.8% had both respiratory diseases. About 4% of participants were daily users of acetaminophen as compared with 8.2 and 2.5% for aspirin and ibuprofen, respectively. Approximately 3% of the population reported use of all three pain medications in the last month and 16% of the population used two different types of pain medications (see Figure E1 in the online supplement).
An increased use of acetaminophen was associated with an increased prevalence of asthma in a dose-dependent manner. The odds ratio (OR) for increasing category of intake was 1.20 (95% confidence interval [CI], 1.12-1.28; p value for trend
Next, we examined whether the acetaminophen-asthma association might differ according to asthma phenotype (p value for interaction, 0.09). We found no association of acetaminophen use and atopic asthma (OR for trend, 1.02; 95% CI, 0.85-1.21), whereas there was a significant association for acetaminophen use and nonatopic asthma (OR for trend, 1.41; 95% CI, 1.06-1.86). Regarding the question of whether pain medications were associated with allergic tendency, we also investigated the association between pain medication use and allergic skin sensitization. Neither ibuprofen nor aspirin was associated with allergic sensitization, but acetaminophen use had an inverse association with atopic sensitization (OR for trend, 0.89; 95% CI, 0.82-0.97). In contrast to the findings for asthma and COPD, the point estimates did not show a clear dose-response trend (OR: never, 1.00; occasional, 0.84; regular, 0.89; data presented in the online supplement).
In analyses considering the acetaminophen-asthma association stratified by aspirin use, the trend among nonusers of aspirin was similar to the overall result (OR trend, 1.23; 95% CI, 1.14-1.32; p value for trend
Acetaminophen use was also associated with an increased prevalence of COPD (OR for increasing category of intake, 1.16; 95% CI, 1.09-1.24; ρ value for trend
When considering the outcome as a diagnosis of both COPD and asthma versus neither condition, the results were comparable to models with the asthma outcome (OR for increasing category of intake, 1.28; 95% CI, 1.13-1.43; p value for trend
FEV^sub 1^ levels were inversely associated with acetaminophen use, and the association was nonlinear (Table 4). Daily users of acetaminophen had a mean adjusted FEV^sub 1^ that was 61.5 ml (95% CI, -97.5 to -25.4) lower than nonusers, and the regression coefficient was only slightly attenuated after adjusting for use of other pain medication (-54.0 ml; 95% CI, -90.3 to -17.7), and after exclusion of subjects with asthma (-46.9 ml; 95% CI, -89.4 to -4.5). When analyses were extended to further exclude participants with COPD, the regression coefficient was attenuated to about half the original value, and was no longer statistically significant (-27.2 ml; 95% CI, -66.5 to +12.3). The use of aspirin was unrelated to lung function, but ibuprofen use had an inverse U-shaped association with FEV^sub 1^. Adjusting for other potential confounders, such as level of education, poverty index, body mass index, comorbidities, or serum antioxidants (vitamin C, vitamin E, or selenium), did not notably alter the results, and there was no evidence of effect modification by smoking status, antioxidant status, age, BMI, or sex. Similar effects as demonstrated for FEV^sub 1^ were found for FVC (Table E4 in the online supplement); however, there was little or no association between use of pain medication and FEV^sub 1^/FVC ratio (data not shown).
DISCUSSION
The current study results are consistent with previous research demonstrating a positive association between acetaminophen use and prevalence of asthma. We also investigated the relation of acetaminophen with the prevalence of COPD and found a significant dose-response relation, which was of about the same magnitude as the association for asthma. Increased use of acetaminophen also was associated with decreased lung function, although this effect was seen only in participants reporting daily (or greater) use of acetaminophen. Finally, we found that regular use of ibuprofen was associated with higher lung function.
One strength of this study is the use of the NHANES III data, which comprise a large study sample representative of the U.S. population. Participants were unaware of the study hypothesis at the time of data collection, thus eliminating potential response bias in answering the pain medication questions. In addition, the use of lung function data provided an objective assessment of respiratory health.
The interpretation of these data is limited by the cross-sectional design of the study. The result may be explained by uncontrolled confounding or by the tendency for persons with disease to use more analgesics (i.e., reverse causality). The specificity of the association with acetaminophen lends support for a cause-effect relation. Other caveats include incomplete characterization of the exposure, as ideally one might wish to measure quantitative dose (milligrams of drug vs. number of times used), variation in use, and duration of use to more fully explore these relations. In this study, we assumed that reported use in the prior month is representative of long-term use. There are also difficulties in defining respiratory outcomes, particularly in the elderly, and there are often misdiagnoses between asthma and COPD. Excluding the other comorbid respiratory disease in the analyses did reduce the size of the effects, but the associations remained statistically significant, thus supporting the hypothesis that acetaminophen use increases the risk of respiratory disease.
In addition, there is the possibility of confounding by indication caused by the design of the study (19): subjects with asthma may avoid aspirin because of sensitivity or physician recommendation, and therefore may preferentially use acetaminophen. We stratified the participants into users and nonusers of aspirin and reanalyzed the acetaminophen-asthma association. The doseresponse trend for acetaminophen-asthma was observed only among the nonusers of aspirin. However, among aspirin users, the regular users of acetaminophen still had a significantly increased risk of asthma (both statistically significant and biologically significant effect size). There was no reason to expect that acetaminophen use was the end result of aspirin avoidance in participants with COPD. In summary, the findings for asthma are not likely explained by confounding by indication, and the consistent association of acetaminophen use with COPD risk and with lower FEV^sub 1^ suggests these associations are worthy of further investigation.
Our findings in the NHANES III data confirm several past reports of an association of acetaminophen with asthma risk, although the effect sizes reported in the literature vary. The first study that reported an acetaminophen-asthma association was a case-control study of asthma in adults (adjusted OR for daily users of acetaminophen compared with never users, 2.4; 95% CI, 1.2-4.6) (13). An ecologic study found a positive association of acetaminophen sales and prevalence of asthma and wheeze in children and adults (14), and two cohort studies confirmed a relation of acetaminophen use with respiratory disease in children exposed in utero and in adult women, respectively (15, 16). The first study found that acetaminophen used late in pregnancy increased the risk of wheezing in the child (OR, 2.10; 95% CI, 1.30-3.41) (15). The other cohort study of adult women found that use of acetaminophen for at least 22 days/month on average was associated with a 1.5-fold increase in the incidence of asthma (95% CI, 0.95-2.46; p trend, 0.0006) (16). Finally, a recent double-blind, randomized, controlled trial of acetaminophen or ibuprofen to treat fever in children found that children with asthma in the study randomized to ibuprofen were less likely to have an outpatient visit for asthma (risk ratio, 0.56; 95% CI, 0.34-0.95) (20). Our results from the cross-sectional NHANES III data support these findings, and taken together, the combined results support the hypothesis that acetaminophen use causes an increase in asthma risk, with potential effects on both the onset and the progression/severity of disease.
Furthermore, our data suggest that use of ibuprofen may be beneficial for lung function, although a linear dose-response relation was not observed: among daily users the association was attenuated. This pattern of effect may be explained by a threshold above which there is no effect, or by random variation in the very small subset of daily users (~2% of total population). Ibuprofen has antiinflammatory properties; specifically, it has been demonstrated to inhibit the migration, swelling, and accumulation of neutrophils and lysosomal enzyme release (21-26). A randomized trial in patients with cystic fibrosis supports this finding; participants randomized to receive ibuprofen compared with placebo had a reduction in annual rate of decline in lung function over 4 years (27). The possible association of ibuprofen with lung function deserves further attention.
Allergic sensitization has an inverse association with pain medication use in these data: there is not strong evidence for a dose response, and this finding is not readily explained. However, allergic sensitization itself is not a lung outcome per se, and our interest in allergic tendency was as a precursor to asthma. For example, asthma in a person with atopy suggests a disease mechanism related to allergic tendency: other causal mechanisms, such as depletion of antioxidant capacity, may not be contributing factors. Thus, the finding of a stronger acetaminophen-asthma association for the subgroup of subjects with nonatopic asthma is of interest. This finding is consistent with the acetaminophenallergic sensitization finding, and suggests that depletion of antioxidant function contributes to nonatopic asthma, but not to atopic asthma where allergic tendency may be the principal factor.
Evidence is beginning to emerge about the potentially harmful effects of consistent use of acetaminophen on respiratory health. We found that increased acetaminophen use was associated with greater prevalence of both asthma and COPD, and with lowered lung function in this large, cross-sectional study. To put these results in context, aspirin avoidance is important in people who have severe, persistent asthma or a history of aspirin sensitivity, and aspirin avoidance in children is important to prevent Reyes syndrome (28). The potential risk of acetaminophen must ultimately be estimated through a balanced consideration of the positive benefit and the potential harm if these medications were substituted with others. Nevertheless, this association provides further evidence of the broader importance of oxidant and antioxidant processes in the pathogenesis of asthma and COPD, and points to a possible overlap in the pathogenesis. Further research, ideally longitudinal investigations, is needed to confirm or refute the findings, particularly the novel findings of an association between acetaminophen use and COPD, and between acetaminophen use and lung function.
Conflict of Interest Statement: T.M.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; S.A.L. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; H.A.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; P.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; j.R.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; P.A.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
1. Anto JM, Vermeire P, Vestbo J, Sunyer J. Epidemiology of chronic obstructive pulmonary disease. Eur Respir J 2001;17:982-994.
2. Maziak W, Behrens T, Brasky TM, Duhme H, Rzehak P, Weiland SK, Keil U. Are asthma and allergies in children and adolescents increasing? Results from ISAAC phase I and phase III surveys in Munster, Germany. Allergy 2003;58:572-579.
3. Fogarty A, Britton J. The role of diet in the aetiology of asthma. Clin Exp Allergy 2000;30:615-627.
4. Smit HA, Grievink L, Tabak C. Dietary influences on chronic obstructive lung disease and asthma: a review of the epidemiological evidence. Proc Nutr Soc 1999;58:309-319.
5. Smit HA. Chronic obstructive pulmonary disease, asthma and protective effects of food intake: from hypothesis to evidence? Respir Res 2001; 2:261-264.
6. Romieu I, Trenga C. Diet and obstructive lung diseases. Epidemiol Rev 2001;23:268-287.
7. Cantin AM, North SL, Hubbard RC, Crystal RG. Normal alveolar epithelial lining fluid contains high levels of glutathione. J Appl Physiol 1987;63:152-157.
8. Jenkinson SG, Black RD, Lawrence RA. Glutathione concentrations in rat lung bronchoalveolar lavage fluid: effects of hyperoxia. J Lab Clin Med 1988; 112:345-351.
9. Smith LJ, Anderson J, Shamsuddin M, Hsueh W. Effect of fasting on hyperoxic lung injury in mice: the role of glutathione. Am Rev Respir Dis 1990;141:141-149.
10. Ketterer B, Coles B, Meyer DJ. The role of glutathione in detoxication. Environ Health Perspect 1983;49:59-69.
11. Chen TS, Richie JP Jr, Lang CA. Life span profiles of glutathione and acetaminophen detoxification. Drug Metab Dispos 1990;18:882-887.
12. Micheli L, Cerretani D, Fiaschi AI, Giorgi G, Romeo MR, Runci FM. Effect of acetaminophen on glutathione levels in rat testis and lung. Environ Health Perspect 1994;102(Suppl 9):63-64.
13. Shaheen SO, Sterne JA, Songhurst CE, Burney PG. Frequent paracetamol use and asthma in adults. Thorax 2000;55:266-270.
14. Newson RB, Shaheen SO, Chinn S, Burney PG. Paracetamol sales and atopic disease in children and adults: an ecological analysis. Eur Respir J 2000;16:817-823.
15. Shaheen SO, Newson RB, Sherriff A, Henderson AJ, Heron JE, Burney PG, Golding J. Paracetamol use in pregnancy and wheezing in early childhood. Thorax 2002;57:958-963.
16. Barr RG, Wentowski CC, Curhan GC, Somers SC, Stampfer MJ, Schwartz J, Speizer FE, Camargo CA Jr. Prospective study of acelaminophen use and newly diagnosed asthma among women. Am J Respir Crit Care Med 2004;169:836-841.
17. National Center for Health Statistics. Plan and operation of the Third National Health and Nutrition Examination Survey, 1988-94. Hyattsville, MD: National Center for Health Statistics; 1994. Vital and Health Statistics, Series 1: Programs and collection procedures, No. 32. DHHS Publication No. (PHS)94-1308; GPO No. 017-022-01260-0.
18. Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general US population. Am J Respir Crit Care Med 1999;159:179-187.
19. Signorello LB, McLaughlin JK, Lipworth L, Friis S, Sorensen HT, Blot WJ. Confounding by indication in epidemiologic studies of commonly used analgesics. Am J Ther 2002;9:199-205.
20. Lesko SM, Louik C, Vezina RM, Mitchell AA. Asthma morbidity after the short-term use of ibuprofen in children. Pediatrics 2002;109:E20.
21. Brown KA, Collins AJ. Action of nonsteroidal, anti-inflammatory drugs on human and rat peripheral leucocyte migration in vitro. Ann Rheum Dis 1977;36:239-243.
22. Higgs GA, Eakins KE, Mugridge KG, Moncada S, Vane JR. The effects of non-steroid anti-inflammatory drugs on leukocyte migration in carrageenin-induced inflammation. Eur J Pharmacol 1980;66:81-86.
23. Shimanuki T, Nakamura RM, Dizerega GS. Modulation of leukotaxis by ibuprofen: a quantitative determination in vivo. Inflammation 1985; 9:285-295.
24. Rinaldo JE, Pennock B. Effects of ibuprofen on endotoxin-induced alveolitis: biphasic dose response and dissociation between inflammation and hypoxemia. Am J Med Sci 1986;291:29-38.
25. Maderazo EG, Breaux SP, Woronick CL. Inhibition of human polymorphonuclear leukocyte cell responses by ibuprofen. J Pharm Sci 1984;73:1403-1406.
26. Flynn PJ, Becker WK, Vercellotti GM, Weisdorf DJ, Craddock PR, Hammerschmidt DE, Lillehei RC, Jacob HS. Ibuprofen inhibits granulocyte responses to inflammatory mediators: a proposed mechanism for reduction of experimental myocardial infarct size. Inflammation 1984;8:33-44.
27. Konstan MW, Byard PJ, Hoppel CL, Davis PB. Effect of high-dose ibuprofen in patients with cystic fibrosis. N Engl J Med 1995;332:848-854.
28. Surgeon General's advisory on the use of salicylates and Reye syndrome. MMWR Morb Mortal Wkly Rep 1982;31:289-290.
Tricia M. McKeever, Sarah A. Lewis, Henriëtte A. Smit, Peter Burney, John R. Britton, and Patricia A. Cassano
University of Nottingham, Nottingham; King's College, London, United Kingdom; National Institute of Public Health, Bilthoven, The Netherlands; and Cornell University, Ithaca, New York
(Received in original form September 24, 2004; accepted in final form February 13, 2005)
Supported by the Wellcome Trust.
Correspondence and requests for reprints should be addressed to Tricia McKeever, Ph.D., Division of Epidemiology and Public Health, Clinical Science Building, City Hospital, Hucknall Road, Nottingham NG5 1PB, UK. E-mail: tricia.mckeever@nottingham.ac.uk
This article has an online supplement, which is accessible from this issue's table of contents online at www.atsjournals.org
Am J Respir Crit Care Med Vol 171. pp 966-971, 2005
Originally Published in Press as DOI: 10.1164/rccm.200409-1269OC on February 25, 2005
Internet address: www.atsjournals.org
Copyright American Thoracic Society May 1, 2005
Provided by ProQuest Information and Learning Company. All rights Reserved