IT'S a call that sends chills down a parent's spine: The day care center says the baby is sick, come quickly. When Kristina and Shannon Smith-Ross reached their then 2-yehr-old daughter, Karmyn, she was in the middle of a massive asthma attack.
"It came out of nowhere," says Kristina Smith-Ross of south suburban Chicago. And that is the most insidious thing about the new asthma--this isn't your mother's asthma, this is new-school asthma. And what the Smith-Ross family learned in their continuing and successful struggle against the disease is a matter of life and death to Black parents to understand the difference between the old and the new asthma.
What is asthma? It is an incurable chronic inflammatory disease of the airways to the lungs, and it is the most common chronic disease of childhood, affecting an estimated 5 million children. Why is it increasing? Experts can't pinpoint why the disease is exploding in cases and severity, but they point to a combination of more air pollution, earlier exposure to irritants that trigger the disease, like food allergies or cigarette smoke, and better methods of diagnosing the disease.
Asthma rates increased 160 percent in the United States among children 4 and younger since 1980 and 80 to 90 percent of children who develop asthma experience symptoms before 5 years of age.
It is the leading cause of school absences, accounting for more than 10 million missed school days a year in 1999.
Asthma can sometimes be a fatal disease; more than 5,000 people die of asthma annually. Children and minorities suffer most. In fact, death rates for asthma are highest among Black youth ages 15 to 24 years old. In 1997, 65 percent of the asthma deaths in the Chicago area occurred in Blacks. "Nationally, asthma hospitalization rates are also highest among Blacks and children," says Dr. James W. Mitchell, a fellow of the American Academy of Pediatrics and currently an assistant professor of clinical pediatrics at the University of Chicago. A recognized expert in children's asthma, Dr. Mitchell says he sees at least one asthma patient daily at his pediatric practice on Chicago's South Side. "I'm considered an aggressive asthma manager," he says. "If treated properly, asthma can almost always be kept under control."
The good news is that children with asthma are now able to live fully active lives without many of the physical limitations they experienced in the past. More than 16 percent of all of the U.S. athletes in the 1996 Summer Olympics in Atlanta had a history of asthma.
The biggest obstacle for treating asthma in children is re-educating parents and health professionals about modern asthma and replacing old notions and beliefs.
Despite the common old wives' tale, children do not "grow out of asthma." Although some children's asthma may improve over time, Dr. Mitchell says "it is also true that if left untreated, many asthmatic children will develop irreversible lung damage in only a few years." That is why it is so important to diagnose asthma as soon as possible and begin treatment.
The major change in modern asthma is that the new primary symptom is not a wheeze but a cough. The cough sounds more like a dry, hacking cough and does not produce much mucus, says Dr. Anne C. Beal, co-author of The Black Parenting Book: Caring for Our Children in the First Five Years and currenfiy senior program officer for the Commonwealth Fund in New York.
The major problem is inflammation of the airways in asthma. Too many parents and caregivers think of everything but asthma when they hear their child coughing, Mitchell adds. "Often by the time the cough first appears there has been at least several days of inflammation developing," he says.
Children, Dr. Beal says, need immediate attention if a parent notices any of the following, "breathing faster than normal, flaring of the nostrils, sucking in of the stomach or pulling in between the ribs."
She says asthma is very sensitive and tricky to diagnose in the first year of life. One reason for this, she says, is that the disease is often confused with other respiratory conditions common at this age, such as respiratory syncytial virus (RSV), which can cause a type of pneumonia in young children, bronchitis and croup (a cold virus that causes a barking cough).
Dr. Beal says there is a strong connection between asthma and allergies, including both hay fever and eczema. She advises African-American mothers in particular to breast feed as long as possible--up to 12 months. "It's a very, very simple thing, but we feed our babies too early and that is likely to contribute to allergies," she says. She advises holding off on solid foods until the baby is 6 months, which is difficult to do, she says, because well-meaning relatives and friends push feeding a baby solids almost from birth. "Even as a physician, my mother would ask me, `When are you going to start giving the baby cereal?'" she says. "It's difficult, but hold off as long as possible."
Once asthma has been diagnosed, parents should check their homes and eliminate all known triggers. Indoor triggers include dust mites, molds, pet dander, cockroaches and cigarette smoke. Mitchell says there is a common misperception that blowing the smoke in another direction or smoking in another room of the house eliminates the effects of smoke on asthmatics. "If smoking takes place anywhere in the house, it can have a negative impact on an asthmatic child," he says.
Outdoor triggers may include molds, pollen from grasses, weeds or trees, cold air and even exercise. Parents should search for the most common triggers and remove them.
Some suggestions:
* To reduce exposure to dust mites, consider hypoallergenic pillow, mattress and box-spring covers. Feather or down pillows should be changed to foam.
* Keep humidifiers off during the spring and summer months.
* Make the child's room a safe place. Dressers, blinds, stuffed animals all hold dust and require weekly cleaning. Also keep the bedroom closet door closed as much as possible, it is another dust haven.
* If the family pet remains, keep it out of the room of the asthmatic child.
* Keep cigarette smoke out of the home.
* Keep the child out of a freshly vacuumed room for at least 30 minutes and away from any strong fumes such as scented cleaners, nail polish remover and paints.
* Once the child is 5 or older, obtain a peak flow meter--a small, portable device that measures how rapidly the child can get air out of the lungs. If measured and recorded daily, the information can provide an early warning system, alerting parents hours to days before the child has symptoms.
* Have a written Asthma Action Plan. Document the daily dose of medication, the child's asthma symptoms and peak flow measurements.
Both Dr. Beal and Dr. Mitchell encourage parents to get regular medical attention for your child and develop a cooperative relationship with the child's doctor to help control the disease.
Managing asthma requires constant consultation with the child's doctor to learn how to use the prescribed medications and how to monitor his breathing.
The disease can change in severity as the child gets older, and it can change intensity from season to season, Dr. Mitchell says. In modern asthma therapy, children are routinely given two types of medications, quick relief medications and control medications. Bronchodilators are still the main class of drug used to treat acute asthma attacks. Medications such as Albuterol and Proventil can be given by mouth, breathing treatment via nebulizer machine or a small, hand-held device called a metered-dose inhaler, or "puffer," Dr. Mitchell adds.
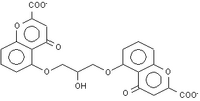
Anti-inflammatory drugs like Cromolyn/Intal have been used to control the inflammation, Dr. Beal says, and new classes of anti-inflammatory drugs, leukotrienne modifiers such as Singulair, block some of the chemical pathways that cause inflammation, Dr. Mitchell adds.
Steroids are still the "most powerful medication for controlling the inflammation of asthma," Mitchell says, and Prednisone or Prednisolone are taken by mouth. "These drugs are taken in a 3- to 7-day burst," Mitchell adds. "This burst is intended to quickly reduce the inflammation of the airways, allow normal breathing and significantly reduce any asthma cough." If the child has more severe asthma and needs the steroids for longer periods of time, physicians use inhaled steroids, taken either by a spray puffer device, dry powder puffer or more recently with a nebulizer.
Navigating the complicated world of asthma with their daughter has been simplified by working with one pediatrician, says Kristina Smith-Ross. Shortly after their daughter was hospitalized, the Smith-Ross family began aggressive management of the disease, and now 5-year-old Karmyn is healthy and virtually symptomfree, her parents say. And that's the goal: controlling the disease so that no child is benched by asthma, either at school or at play.
COPYRIGHT 2002 Johnson Publishing Co.
COPYRIGHT 2003 Gale Group