Clinical question Does the addition of ipratropium bromide to [Beta]-agonist therapy improve outcomes in adults with acute asthma exacerbations?
Background The role of anticholinergic bronchodilators is unclear in the treatment of asthma exacerbations, and existing studies of their effectiveness have mixed results. This meta-analysis synthesizes the evidence.
Population studied The patients included in the studies in this meta-analysis were adults presenting to a hospital emergency department (ED) with an acute asthma exacerbation. Studies evaluating only children, or adults with chronic obstructive pulmonary disease exacerbations, were excluded.
The authors identified 54 studies for possible inclusion. Ten studies involving 1530 patients met the final criteria. Seven studies used albuterol as the [Beta]-agonist; 3 used fenoterol. In 4 studies, all patients received steroids; in 3, some proportion did (though it was not noted which patients received what proportion); and in 3 others, no patients received steroids. Quality scores ranged from 2 to 5 (maximum score = 5), with 60% rating 4 or higher.
Study design and validity The authors conducted a comprehensive search of MEDLINE, EMBASE, the CINAHL database, the Cochrane Controlled Trials Register, Current Contents, and Biological Abstracts to identify articles for this review. They contacted the drug manufacturer for unpublished data. (No unpublished studies were found, this is an unlikely source of bias given the distribution of the funnel plot.)
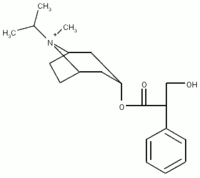
A study was included if it met the population and outcome criteria noted and was a placebo-controlled randomized trial evaluating ipratropium bromide (by nebulizer of meter-dose inhaler) as an adjunct to [Beta]-agonist therapy. The authors restricted inclusion to articles published in English, French, or Italian, which may introduce a bias.
Two nonblinded independent reviewers applied inclusion criteria, critically appraised the articles using an appropriate prevalidated scale, and abstracted data. There was good agreement between the reviewers for each step.
The results of the included studies were heterogeneous, or not statistically similar, raising the question of the appropriateness of combining them in a meta-analysis. A qualitative look at the studies showed an outlying study that had patients with a much lower peak expiratory flow rates (PEFR) at baseline, perhaps accounting for their greater proportional improvement. Excluding this study from the analysis produced homogeneity and did not significantly change the review results.
Overall, this was a well-conducted meta-analysis, and the potential biases are unlikely to have a concerning effect on the results.
Outcomes measured The primary outcome for this meta-analysis was some measurement of airflow obstruction, either forced expiratory volume in 1 second ([FEV.sub.1]) or PEFR. The authors also reported outcomes for hospitalization rates, length of ED stay, concurrent medication use, and adverse effects of the medication when reported by the original studies.
Results Spirometry measurements were taken from 30 to 90 minutes after medication dosing. Pooling the 6 studies measuring [FEV.sub.1] demonstrated a 7.3% improvement (95% confidence interval [CI], 3,8 - 10.9), equivalent to an average absolute flow improvement of 100 mL. Four studies measuring PEFR were pooled, resulting in a 22.1% improvement (95% CI, 11.0% - 33.2%), equivalent to an average absolute flow rate improvement of 32 L per minute. The clinical significance of these results is unclear. Those with more severe airflow obstruction at baseline had the greatest effect.
No studies reported ED length of stay or the influence of the intervention on other medication use. Only 3 studies evaluated hospitalization rates (n = 1064); those receiving ipratropium bromide were 27% less likely to be hospitalized (relative risk = 0.73; 95% CI, 0.53-0.99) Rates were not given, thus precluding a number-needed-to-treat calculation. No trial reported serious adverse effects. There were no differences in adverse effects between the 2 groups.
Recommendations for clinical practice The addition of ipratropium bromide to the standard regimen of [Beta]-agonists in adults with acute asthma exacerbations improves intermediate outcomes and modestly decreases hospitalization rates. Since this benefit seems greatest in those with more severe asthma attacks, the use of ipratropium bromide may be especially warranted in this group. Further study, including cost analysis, is needed before this becomes standard asthma treatment.
Stoodley RG, Aaron SD, Dales RE. The role of ipratropium bromide in the emergency management of acute asthma exacerbation: a meta-analysis of randomized clinical trials. Ann Emerg Med 1999; 34:8-18.
COPYRIGHT 1999 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group