Schools in Pharmacology is a new feature in that will appear periodically. It will explicate the dermatologic uses and side effects of new medications and devices. It follows medications mentioned in the Pipeline Previews into their approval and use in clinical practice.
Erlotinib, Voriconazole, Omalizumab, Tigecycline, and Zeno
This article will provide a brief review of 5 medications and devices approved in the last several years that touch on cutaneous medicine, which have not been extensively reviewed in the dermatology literature. The following medications and devices will be discussed (1) Zeno--a new over-the-counter device used to treat acne, (2) erlotinib (Tarceva) an oral epidermal growth factor receptor (EGFR) inhibitor for treatment of advanced non-small cell lung cancer which causes an acneiform eruption and whose eruptions tracks its efficacy, (3) voriconazole (Vfend) is a broad-spectrum azole antifungal agent, which can treat deep fungal infections and induce cutaneous eruptions and photosensitivity (4) omalizumab (Xolair) a recombinant humanized monoclonal antibody approved to treat asthma, and (5) tigecycline (Tygacil), a novel intravenous antibiotic with a broad spectrum of antimicrobial activity that can treat complicated skin structure infections even if caused by antibiotic resistant bacteria. Each of these medications and devices is important for dermatologists to be aware of because of their cutaneous uses and/or side effects.
Zeno
Zeno is an acne clearing device that is available without a prescription. It is a hand-held, portable electronic medical device approved by the FDA in 2005 to treat patients with mild to moderate acne. (1,2) The treatment tip is made from a biocompatible material and delivers a specific low-level heat to the individual acne blemish. The device is powered by rechargeable AAA nickel-metal hydride batteries. In an FDA-reviewed, controlled clinical trial, 90% of acne papules treated with Zeno disappeared or faded within 24 hours. No peer-reviewed studies have been published regarding Zeno.
As mentioned above, Zeno applies a precisely controlled heat dose directly to acne papules through a metal pad. One treatment lasts 2.5 minutes. Two to three treatments spread over 24 hours help clear acne papules. Some experts recommend treating acne papules 2 to 4 times, at least 1 hour apart, over the first 4 to 12 hours of the acne papules appearance. It is thought that the mechanism of Zeno involves thermally induced destruction of bacteria and induction of anti-inflammatory effects. It is also possible that Zeno increases blood flow in the area of the acne papules and promotes quicker healing. It works best when used in the early stages of development. Zeno can induce transient erythema. Experts state that Zeno does not replace normal skin care programs and is completely compatible with prescription and over-the-counter acne treatments.
Erlotinib (Tarceva)
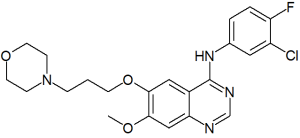
Erlotinib (Tarceva, Genentech/OSI) is the second oral epidermal growth factor receptor (EGFR) inhibitor approved by the FDA for treatment of advanced non-small cell lung cancer (NSCLC). (3) Gefitinib (Iressa) was the first oral EGFR inhibitor approved. Erlotinib and gefitinib were approved only for patients who have failed at least one prior chemotherapy regimen. On December 17, 2004, the FDA noted that it had learned that a large clinical trial comparing gefitinib with placebo in patients with non-small cell lung cancer who had failed other courses of cancer therapy showed no survival benefit. Nevertheless, the FDA stated patients currently taking Iressa should consult with their physicians as soon as possible and not change their therapy without first consulting with their physicians. Cetuximab (Erbitux), the only other EGFR inhibitor available in the US, is approved for intravenous treatment of metastatic colon cancer.
Erlotinib was evaluated in a randomized, double-blind, placebo-controlled trial in 731 patients with locally advanced or metastastic NSCLC who had failed at least one chemotherapy regimen. (3) The response rate was 8.9%, with a median response duration of 34.3 weeks. Median survival in patients taking the drug was 6.7 months, compared to 4.7 months in those taking placebo, a statistically significant difference. Patients who had never smoked and those with at least 10% of tumor cells testing positive for EGFR survived longer. Two additional studies compared platinum-based combination chemotherapy alone or plus erlotinib in previously untreated patients with advanced NSCLC; the addition of erlotinib to chemotherapy did not improve the response rate or overall survival.
A considerable number of patients treated with these EGFR inhibitors develop dermatological side effects, most frequently an acneiform eruption but also xerosis, eczema, fissures, telangiectasia, hyperpigmentation, hair changes, and paronychia with pyogenic granuloma. (4) These skin effects appear to be mechanism-based linked to the inhibition of EGFR action, but the exact pathophysiology is unclear. Mild cases of acneiform eruption respond well to topical anti-inflammatory acne therapy, whereas tetracyclines are needed to treat moderate to severe cases.
Interestingly, the rash associated with HER1/EGFR inhibition can be used as a marker of treatment outcome. (5) Analysis of phase II trials of erlotinib in non-small-cell lung cancer, head and neck cancer, and ovarian cancer shows a significant association between rash severity and objective tumor response. Rash severity was highly significantly associated with survival in patients with non-small-cell lung cancer receiving erlotinib; median survival in patients with no rash was 46.5 days, compared with 257 days in those with grade 1 rash (P < .0001) and 597 days in those with grade 2/3 rash (P < .0001). Similarly, for the combined non-small-cell lung cancer, head and neck cancer, and ovarian cancer studies, median survival in patients with no rash was 103 days, compared with 191 days in those with grade 1 rash (P = .0001) and 266 days in those with grade 2/3/4 rash (P = .0001).
Voriconazole (Vfend)
Approved for use in 2002, voriconazole (Vfend, Pfizer) is a broad-spectrum azole antifungal agent structurally derived from fluconazole that is orally administered. (6,7) Voriconazole works by preventing fungi from producing a substance called ergosterol. It is indicated for the treatment of invasive aspergillosis and serious fungal infections caused by Scedosporium apiospermum and Fusarium species in patients who are unable to tolerate, or are refractory to, other antifungal therapy. It is likely an effective treatment for chromomycosis and other deep fungal and serious yeast infections.
In head-to-head comparative trials, voriconazole appeared to be as efficacious as amphotericin B for the treatment of invasive aspergillosis and the empiric treatment of fungal infections in patients with febrile neutropenia. In clinical studies, voriconazole was as efficacious as fluconazole for the treatment of oropharyngeal and esophageal candidiasis. The results of in vitro susceptibility studies and case reports suggested that voriconazole may be useful against fluconazole and/or itraconazole-resistant strains of Candida.
Although voriconazole may be associated with a lower incidence of serious systemic adverse effects compared with amphotericin B (13.4% vs. 24.3% in 1 pivotal clinical study; P = NS), major adverse effects associated with voriconazole include visual abnormalities (approximately 30%), and elevations in hepatic enzymes ([less than or equal to]20%). Voriconazole is available as oral and intravenous formulations. Pharmacokinetically, it has widespread distribution, including penetration into cerebral tissue.
Voriconazole has a high potential for drug interactions. This is because 80% of voriconazole is hepatically eliminated, primarily via the cytochrome P450 (CYP) isozymes CYP2C19, CYP3A4, and CYP2C9. Therefore, dose reduction is recommended in patients with mild to moderate hepatic dysfunction (Child-Pugh class A or B).
Voriconazole causes skin reactions in approximately 20% of patients. In clinical trials, these were described as "rash on trunk and arms," "facial erythema," "exanthema," "generalized erythema," "head, neck and shoulder erythema," "neck redness," "dermatitis," and "allergic skin reaction." (8) Voriconazole may cause cutaneous photosensitivity reactions. In trials, these were described as "photosensitivity skin reaction," "photosensitization of face," "photosensitivity rash," "skin rash in sun exposed regions," and "sunburn." As it can cause hepatic failure, it can make skin and eyes yellow. (8) These cutaneous side effects mandate that dermatologists remain vigilant in patients who use voriconazole.
Omalizumab (Xolair)
Omalizumab (Xolair, Novartis Pharmaceuticals, East Hanover, NJ; Genentech Inc., South San Francisco, CA) is a recombinant humanized monoclonal antibody that blocks immunoglobulin E's (IgE) high-affinity Fc receptor. Omalizumab stops free-serum IgE from attaching to mast cells and other immune cells and prevents IgE-mediated inflammatory changes. (9)
Omalizumab is used to treat asthma, which is part of the atopic triad with atopic dermatitis and allergic rhinitis. As such, omalizumab is of interest to dermatologists because (1) patients might be taking it, (2) its immunological effects on IgE, and (3) it might be a treatment of atopic dermatitis. Its promise as a treatment for atopic dermatitis has not been borne out. A recent report noted the failure of omalizumab to improve atopic dermatitis in 3 patients when administered for 4 months. (10) It seems then that the blockage of IgE does not directly and substantially impact on the development and continuation of atopic dermatitis.
Tygacil (Tigecycline)
On June 15, 2005, the FDA approved tigecycline (Tygacil, Wyeth Pharmaceuticals), a novel intravenous antibiotic with a broad spectrum of antimicrobial activity, including activity against the drug-resistant bacteria methicillin-resistant Staphylococcus aureus (MRSA). (11,12) Tigecycline is indicated for the treatment of complicated intra-abdominal infections (cIAI) and complicated skin and skin structure infections (cSSSI) in adults. A cSSSI involves deeper soft tissue or requires significant surgery and includes infected ulcers, burns, or bites; major abscesses; and superficial infections or abscesses with a high risk of infection by anaerobic or Gram-negative bacteria. It is a glycylcycline, a class of antibiotic discovered in 1993 by modification of the structure of the tetracycline molecule.
Tigecycline successfully completed phase III trials in which it was found to be at least equal to intravenous vancomycin and aztreonam in treating cSSSI, and to intravenous imipenem and cilastatin in treating complicated intraabdominal infections (cIAI). (11) Tigecycline side effects are primarily digestive upset. It should be a valuable addition to the armamentarium to treat even the most resistant pathogens. For cSSSI as compared with vancomycin and aztreonam in which about 12% of patients had skin eruptions, only about 7% of patients developed eruptions using tigecycline.
References
1. Medical News Today. New Zeno 'Zit Zapper': First Home Acne Treatment Device Gets FDA Approval. Available at: http://www.medicalnewstoday.com/medicalnews.php?newsid=25679. Accessed September 14, 2005.
2. Department of Health and Human Services. Available at: http://www.fda.gov/cdrh/pdf4/K043377.pdf. Accessed Sepember 14, 2005.
3. Erlotinib (Tarceva) for Advanced Non-Small Cell Lung Cancer; The Medical Letter. 2005;47(1205):25-28.
4. Segaert S, Van Cutsem E. Clinical signs, pathophysiology and management of skin toxicity during therapy with epidermal growth factor receptor inhibitors. Ann Oncol. 2005;16(9):1425-33.
5. Perez-Soler R. Can rash associated with HER1/EGFR inhibition be used as a marker of treatment outcome? Oncology (Williston Park). 2003;17(11 Suppl 12):23-8.
6. Jeu L, Piacenti FJ, Lyakhovetskiy AG, Fung HB. Voriconazole. Clin Ther. 2003;25(5):1321-81.
7. Voriconazole. The Medical Letter. 2002;(1135):63-65.
8. Reinhard B. Voriconazole in vitro in-house and external data. Available at: http://www.fda.gov/ohrms/dockets/ac/01/slides/3792s2_01_1-Pfizer-main.ppt. Accessed September 14, 2005.
9. Scheinfeld N. Omalizumab: a recombinant humanized monoclonal IgE-blocking antibody. Dermatol Online J. 2005;11(1):2.
10. Krathen RA, Hsu S. Failure of omalizumab for treatment of severe adult atopic dermatitis. J Am Acad Dermatol. 2005;53(2):338-40.
11. McConnell J. Results of tigecycline trials announced. Lancet Infect Dis. 2004;4:717.
12. Tucker ME. Tigecycline promising for serious skin infections. Skin & Allergy News. 2005;36(2):2.
Noah Scheinfeld MD
St. Lukes-Roosevelt Hospital Center, New York, NY
COPYRIGHT 2005 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2005 Gale Group