Electrical stimulation over the motor cortex, base of the skull, and cervical spine motor roots was performed in 9 male rats (410 86 g) before and after induction with isoflurane at 1 MAC concentration. The mean latency and amplitude of descending spinal evoked potential (DSEP) from spinal cord and motor evoked potentials (MEPs) from forearm muscles obtained after motor cortex, brainstem, and cervical root stimulations were calculated and compared. The electrical current intensity to elicit the MEPs after cortical, brainstem, and spinal roots stimulation were 23.4 + 7.6, 7.0 A 3. 1, and 1.4 + 0.8 mA, respectively. The brainstem stimulation activated descending motor pathways with a latency midway between that produced by electrical stimulation over the motor cortex, and by electrical stimulation over the cervical enlargements. The latency difference between cortical (8.8 +/- 3.2 msec) and brainstem (5.7 i 1.2 msec) stimulation was 3.1 i 2.3 msec in all forearm extensor muscles. The latency difference between cervical (3.6 0.9 msec) and brainstem stimulation (5.7 +/- 1.2 msec) was 2.3 1.1 msec for the same muscles, suggesting the brainstem stimulation activates the descending motor neurons at the level of cervicalmedullary junction. The amplitudes were 189 +/- 141, 672 +/- 354, and 765+ 389,uV for cortical, brainstem, and cervical root stimulations. The inhalation anesthesia isoflurane at 1 MAC (1.2%) completely abolished the cortical and brainstem MEPs within minutes, while the MEPs elicited by direct stimulation of the cervical spinal roots remained unchanged. Our results indicate synaptic-dependent MEPs elicited at motor cortex or brainstem levels are highly sensitive to isoflurane anesthesia. [Neurol Res 1998; 20: 555-558]
Keywords: Compound muscle action potential; isoflurane; motor evoked potentials; spinal motor root
INTRODUCTION
Motor evoked potential (MEP) is a response evoked in a target muscle after transcranial or transcortical motor cortex stimulation'-. MEP recording is an important technique in clinical neurophysiology and a unique monitor of descending motor pathways in man . Central motor conduction time (CMCT) is calculated by subtracting the latency of the muscle response to spinal root stimulation from the latency of the response produced by motor cortex stimulation. Prolongation of the CMCT is an indication of slowing of neuronal conduction within the brain or spinal cord tissue9'10. The corticospinal tract can also be activated at the level of the cervical-medullary junction where the pyramidal decussation lies using high intensity electrical or magnetic stimulation across the skull base9-". Regardless of the site of stimulation, motor cortex or brainstem, many factors can affect the MEP response, including surgical maneuvers, core body temperature, systemic hypotension, hypoxia, and anesthetic agents . Isoflurane anesthesia is commonly used in neurosurgical anesthesiology, with or without nitrous oxide and with added analgesics such as fentanyl2'. The effects of isoflurane on electroencephalogram (EEG), sensory evoked potentials and cerebral metabolism, and hemodynamic values have been reported22-25. Several investigations presented evidence that isoflurane can also have a profound effect on MEPs26'27.
The present study investigates the differential effects of isoflurane on MEPs elicited by motor cortex, brainstem, and cervical spinal root stimulation in the mechanically ventilated rat.
MATERIALS AND METHODS
Nine Sprague-Dawley male rats weighing 410i 86 g were anesthetized by a single intraperitoneal injection of sodium pentobarbital (35 mg kg-'). After tracheal cannulation, catheters were inserted into the left femoral artery and vein for blood pressure monitoring and administration of fluids. The animals were immobilized in a stereotaxic head holder (Model 1404, Kopf Instruments, Tujunga, CA, USA) and placed on a heating blanket (Aquamatic K-model, Gorman Rupp Industries, Belteville, OH, USA). The rectal body temperature was monitored and maintained at 36 +/- 0.5oC by a temperature controller unit (CMA/150, CMA Microdialysis, Stockholm, Sweden). Heart rate was continuously monitored using a standard electrocardiograph machine. Mean arterial blood pressure was determined from a pressure transducer and a chart recorder (Model RS 3400, Gould Instruments, Cleveland, OH, USA). Animals were ventilated by a small animal respirator (Motor 683, Harvard Rodent Ventilator, Harvard Apparatus, South Natick, MA, USA). The respiratory rate was 75 cycles min-1, and the tidal volume was adjusted to 3 ml. A 4-cm rostro-caudal incision was made in the midline scalp. The periosteum was scraped laterally, and the skull was cleaned and dried to reveal the suture lines. A left-sided craniotomy (==10 mm in diameter) was performed overlying the motor cortex. The dura was left intact and warm mineral oil (36-38C) was applied to the dura to prevent tissue desiccation. A wide cervical laminectomy was performed at C1-C6 levels which included removal of bone at the occipitocervical junction. A two-level midthoracic laminectomy was performed for placement of a bipolar platinum recording electrode.
Animals underwent cortical, brainstem, and cervical spinal root stimulation using bipolar platinum ball electrodes with a tip separation of 3 mm. Single shock stimulation was used to elicit an isolated compound muscle action potential (CMAP) from forelimb extensors or a descending spinal evoked potential (DSEP) from the thoracic spinal cord. The stimulus parameters were a single pulse square wave of 0.2 msec in duration with the intensity ranging from 10-35 mA. Two recording needle electrodes were inserted into the forelimb muscles to obtain the CMAPs. A ground electrode was placed on the temporalis muscle. A signal averager (Model Quantum 84, Cadwell Laboratories, Kennewick, WA, USA) was used for amplification and filtering of the responses. Time base was 30 msec, and low- and highcutoff filters were set at 10 and 3,000 Hz, respectively. Electrode impedance was maintained at
RESULTS
Representative DSEP and CMAP evoked by corticomotor, brainstem, and cervical spinal root stimulation before and after isoflurane anesthesia are illustrated in Figure 1. The DSEP recorded from mid-thoracic (T8-9) segment was composed of a positive-negative wave with a mean duration of 6.2 +/- 0.4 msec (n = 9). The CMAP consisted of a multiphasic wave form with a mean duration of 7.4 + 0.8 msec (n = 9). Table 1 demonstrates the values in DSEP and CMAP latency and amplitude after cortical, brainstem, and cervical root stimulation prior to isoflurane anesthesia. The electrical intensities used to elicit these responses were 23.4 i 7.6 mA (cortical), 7.0 i 3.1 mA (brainstem), and 1.4 0.8 mA (cervical root). At 1.2% concentration of isoflurane (1 MAC), 9/9 animals (100%) lost the responses to corticomotor and brainstem stimulation. Figure 1 illustrates the recovered DSEP and CMAP tracings after isoflurane was discontinued for 30 min. The brainstem stimulation activated descending motor pathways with a latency midway between that produced by electrical stimulation over the motor cortex, and by electrical stimulation over the cervical enlargements. The latency difference between cortical (8.8 + 3.2 msec) and brainstem (5.7 i 1.2 msec) stimulation was 3.1 +/- 2.3 msec in all forearm extensor muscles. The latency difference between cervical (3.6 + 0.9 msec) and brainstem stimulation (5.7 i 1.2 msec) was 2.3 +/- 1.1 msec for the same muscles, suggesting the brainstem stimulation activates the descending motor neurons at the level of cervicomedullary junction. The amplitudes were 1894141, 672:354, and 765 + 389 uV for cortical, brainstem, and cervical root stimulations.
Isoflurane at 1 MAC concentration completely abolished the MEPs elicited after cortical or brainstem stimulation within minutes of induction, while the MEPs from the cervical spinal root stimulation remained unchanged.
DISCUSSION
Descending motor tracts can be activated directly or indirectly at several levels using high intensity electrical or magnetic stimulation29-3 . Ugawa et al. reported activation of corticospinal tract at the pyramidal decussation level by the use of high intensity electrical or magnetic stimulation. According to these authors, only selected patients could be studied with the electrical stimulation because of the pain induced by this techniqueg. Cervical and lumbar spinal motor roots can also be activated using electrical or magnetic stimulation. At the cervical level, it has been suggested that motor axons are likely to be activated about 4 cm distal to the anterior horn cells3'. Regardless of the method of stimulation, the resultant response, known as MEPs, can be subject to alterations independent of any injuries or insults to the motor pathway. We studied the effect of isoflurane on the DSEP and CMAP after sequential electrical stimulation of the motor cortex, brainstem, and cervical spinal roots innervating forelimb extensors. Previous experimental and clinical reports have indicated the deleterious effect of inhalation anesthesia on EEG3233, auditory evoked potentials34, visual evoked potentials25, somatosensory evoked potentials24, and MEPs15,16. The present study compared sensitivity of MEPs elicited after the corticomotor and brain stem stimulation under general inhalation anesthesia. Our results indicate that, regardless of the site of stimulation, cortex or brainstem, the MEPs demonstrate similar sensitivity to the anesthetics. A similar finding was reported by Hicks et al. in which withdrawal of isoflurane dramatically increased the number as well as the amplitude of indirect (I) waves recorded at the spinal level26. According to a previous experimental study, an increase in isoflurane concentration resulted in a progressive increase in the evoked muscle response latency, and decreases in the amplitude and the duration. The level of significant change (p = 0.01) in these three variables started at concentrations as low as 0.5%35. The MEPs evoked after spinal root stimulation were not sensitive to isoflurane. These responses remained essentially unchanged throughout the anesthesia period.
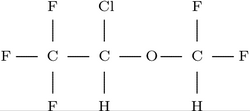
Isoflurane is a structural isomer of enflurane with a different arrangement of halogens on the ethyl group. This compound is the least soluble of inhalation anesthetic agents in blood and body tissues. This accounts for its rapid induction time and its very rapid recovery time36. As is true of other halogenated anesthetic agents, the exact site of action of isoflurane is not definitively known. Most evidence is consistent with inhibition of synaptic transmission produced by an action of inhaled anesthetics at a hydrophobic site on biologic membranes. A single theory to explain the mechanism of anesthesia seems unlikely. Various theories have been proposed, but none is conclusive 21.37.
In conclusion, our study shows that the MEP rat is affected by isoflurane anesthesia. Although in the rat is affected by isoflurane has many qualities which suggest Although advantages for use in neurosurgical ane has many qualities which suggest it has study demonstrates that continued research in neurosurgical anesthesia, our study demonstrates than agent compatible with clinued research is necessary to discover an agent compatible with clinical MEP monitoring.
REFERENCES
1 Marsden CD, Merton PA, Morton HB. Percutaneous stimulation of spinal cord and brain: Pyramidal tract conduction velocities in man. J Physiol 1982; 328: 6
2 Barker AT, Jalinous R, Freeston IL. Non-invasive magnetic stimulation of human cortex. Lancet 1985; 2: 1106-1107 3 Hallett M, Cohen LG. Magnetism. A new method for stimulation of nerve and brain. /AMA 1989; 262: 538-541 4 Merton PA, Morton HB. Stimulation of the cerebral cortex in the intact human subject. Nature 1980; 285: 227 5 Boyd SG, Rothwell JC, Cowan JMA, et al. A method of monitoring function in corticospinal pathways during scoliosis surgery with a note on motor conduction velocities. J Neuro/ Neurol Neurosurg Psychiatry 1986; 49: 251-257
6 Edmonds HL, Paloheimo MPI, Backman MH, et al. Transcranial magnetic motor evoked potentials (tc MMEP) for functional monitoring of motor pathways during scoliosis surgery. Spine 1989; 14: 683-686
7 Morota N, Deletis V, Constantini S, et al. The role of motor evoked potentials during surgery for intramedullary spinal cord tumors. Neurosurgery 1996; 41: 1327-1336
8 Pechstein U, Cedzich C, Nadstawek J, et al. Transcranial highfrequency repetitive electrical stimulation for recording myogenic motor evoked potentials with the patient under general anesthesia. Neurosurgery 1996; 39: 335-343
9 Ugawa Y, Rothwell JC, Day BL, et al. Percutaneous electrical stimulation of corticospinal pathways at the level of the pyramidal decussion in humans. Ann Neurol 1991; 29: 418-427 10 Ugawa Y, Genba K, Mannen T, et al. Stimulation of corticospinal pathways at the level of the pyramidal decussation in neurological disorders. Brain 1992; 155: 1947-1961
11 Ugawa Y, Uesaka Y, Terao Y, et aL Magnetic stimulation of corticospinal pathways at the foramen magnum level in humans. Ann Neurol 1994; 36: 618-624
12 Oro JJ, Haghighi SS. Effects of altering core body temperature on somatosensory and motor system evoked potentials. Spine 1992; 17: 498-503
13 Haghighi SS, Oro JJ. Effects of hypovolemic hypotensive shock on somatosensory and motor evoked potentials. Neurosurgery 1989; 24: 246-251
14 Haghighi SS, Keller BP, Oro JJ, et al. Motor evoked potential changes during hypoxic hypoxia. Surg Neurol 1993; 39: 399-402
15 Zentner J, Ebner A. Nitrous oxide suppresses the electromyographic response evoked by electrical stimulation of the motor cortex. Neurosurgery 1989; 24: 60-62
16 Zentner J, Kiss I, Ebner A. Influence of anesthetics-nitrous oxide in particular-on electromyographic response evoked by transcranial electrical stimulation of the cortex. Neurosurgery 1989; 24: 253-256
17 Hicks R, Burke D, Stephen J, et al. Corticospinal volleys evoked by electrical stimulation of human motor cortex after withdrawal of volatile anaesthetics. I Phvsiol 1992:456: 393-404
18 Jellinek D, Platt M, Jewkes D, etal. Effects of nitrous oxide on motor evoked potentials recorded from skeletal muscle in patients under total anesthesia with intravenously administered propofol. Neurosurgery 1991; 29: 558-563
19 Woodforth IJ, Hicks RG, Crawford MR, et al. Variability of motorevoked potentials recorded during nitrous oxide anesthesia from the tibialis anterior muscle after transcranial electrical stimulation. Anesth Analg 1996; 82: 744-749
20 Kalkman CJ, Drummond JC, Kennelly NA, et al. Intraoperative monitoring of tibialis anterior muscle motor evoked responses to transcranial electrical stimulation during partial neuromuscular blocka e. Anesth Anal,e 1992; 75: 584-589
21 Michenfelder JD. Anesthesia and the Brain. New York: Churchill Livingstone, 1988: pp. 79-91
22 Newberg LA, Milde JH, Mickenfelder JD. The cerebral metabolic effects of isoflurane at and above concentrations that suppress cortical electrical activity. Anesthesiology 1983; 59: 23-28 23 Todd MM, Drummond JC. A comparison of the cerebrovascular and metabolic effects of halothane and isoflurane in the cat. Anesthesiology 1984; 60: 276-282
24 Pathak KS, Amaddio MD, Scoles PV, et al. Effects of halothane, enflurane, and isoflurane in nitrous oxide on multilevel somatosensory evoked potentials. Anesthesiology 1989; 70: 207-212
25 Domino EF. Effects of preanesthetic and anesthetic drugs on visually evoked responses. Anesthesiology 1967; 28: 184-191 26 Hicks RG, Burke D, Stephen J, et al. Corticospinal volleys evoked by electrical stimulation of human motor cortex after withdrawal of volatile anaesthetics. J Physiol 1992; 456: 393404 27 Hicks RG, Woodforth II, Crawford MR, et al. Some effects of isoflurane on I waves of the motor evoked potential. J Anesthesia 1992; 69: 130-136
28 Merton PA, Morton HB. Stimulation of the cerebral cortex in the
intact human subject. Nature 1980; 284: 227 29 Marsden CD, Merton PA, Morton HB. Percutaneous stimulation of spinal cord and brain: Pyramidal tract conduction velocities in man. J Physiol (Lond) 1982; 328: 61
30 Ugawa Y, Uesaka Y, Terao Y, et aL Magnetic stimulation of the descending and ascending tracts at the foramen magnum level. Elect and Clin Neurophys 1997; 105: 128-131 31 Ugawa Y, Rothwell JC, Day BL, et al. Magnetic stimulation over the spinal enlargement. I Neurol Neurosurg Psychiatry 1989; 52: 1025-1032
32 Clark DL, Rosner BS. Neurophysiologic effects of general anesthetics. Anesthesiology 1973; 38: 564-581 33 Hosick EC, Clark DL, Adam N, et al. Neurophysiological effects of different anesthetics in conscious man. J Appl Physiol 1971; 31: 892-897
34 Thornton C, Heneghan CP, James MF, et aL Effects of halothane or enflurane with controlled ventilation on auditory evoked response. Br J Anaesth 1984; 56: 315-323
35 Haghighi SS, Green D, Oro JJ, et al. Depressive effect of isoflurane anesthesia on motor evoked potentials. Neurosurgery 1990; 26: 993-997
36 Paddleford RR. General anesthesia. In Paddleford RR, ed. Manual of Small Animal Anesthesia, New York: Churchill Livingstone 1988: pp. 62-73
37 Roth SH. Mechanisms of anesthesia. A mystery. Can J Anaesth 1988; 35: S1-S3
38 Lockhart SH, Cohen Y, Yasuda N. Cerebral uptake and elimination of desflurane, isoflurane and halothane from rabbit brain: An in vivo NMR study. Anesthesiology 1991; 74: 575-580
Section of Neurosurgery, Department of Surgery, University of Nebraska Medical Center, Omaha, NE, USA
Correspondence and reprint requests to: Siavash S. Haghighi, DVM, PhD, Section of Neurosurgery, UNMC, 600 S. 42nd Street, Omaha, NE 68198, USA. Accepted for publication April 1998.
Copyright Forefront Publishing Group Sep 1998
Provided by ProQuest Information and Learning Company. All rights Reserved