Study objectives: To establish a murine model of pneumothorax-associated pleural eosinophilia and to examine the role of interleukin (IL)-5 and IL-13 in the pathogenesis of this reaction.
Design: An animal study.
Interventions: One hundred thirty-seven C57/Bl-6 mice were used in this study. Wild-type animals were injected intrapleurally with 0.4 mL of air and were killed at different time points (30 min to 7 days) after the injection. IL-5 knockout and IL-13 knockout animals were killed 24 h and 48 h after the injection. Pleural inflammation was assessed by pleural lavage (PL).
Measurements and results: PL cells were significantly increased following the induction of pneumothorax. The peak number of neutrophils, observed at 12 h, was 900 times higher than the control. The peak number of eosinophils, observed at 48 h, was 700 times higher than the control. Lymphocytes and mononuclear cells increased threefold and fourfold, respectively. IL-5 knockout mice had significantly less PL eosinophils than that the wild-type or the IL-13 knockout mice at 24 h (150 [+ or -] 46/[micro]L, 903 [+ or -] 244/[micro]L, and 912 [+ or -] 168/[micro]L, respectively; p = 0.013) and 48 h (181 [+ or -] 45/[micro]L, 1,587 [+ or -] 212/[micro]L, and 1,379 [+ or -] 364/[micro]L, respectively; p = 0.003).
Conclusion: Pneumothorax induces an inflammatory reaction of the mouse pleura, mainly characterized by increased neutrophils and eosinophils. IL-5 but not 1L-13 is required for pneumothorax-associated pleural eosinophilia.
Key words: animal model; eosinophils; interleukin-5; interleukin-13; pleura; pneumothorax
Abbreviations: EPE = eosinophilic pleural effusion; IL = interleukin; PL = pleural lavage; Th2 = T-helper type 2
**********
Eosinophilic pleural effusions (EPEs) are most commonly due to the presence of air or blood in the pleural space. (1) Although EPEs account for 5 to 16% of exudative pleural effusions, (1) it is still unclear how different stimuli result in eosinophilic pleural inflammation.
The tissue accumulation of eosinophils requires increased production of, migration and extended survival of these cells in the tissue. (2) Interleukin (IL)-5 enhances eosinophil survival and contributes to their development, differentiation, chemoattraction, and activation. (3,4) The observation that pleural fluid IL-5 levels are higher in EPEs than in non-EPEs and are correlated with the percentage of pleural eosinophilss (5,6) supports the hypothesis that this cytokine is important in the pathogenesis of EPE. IL-13 plays a major role in T-helper type 2 (Th2)-dependent eosinophilic inflammation. (7) IL-13 induces the expression of eotaxin, (8) a potent eosinophil chemoattractant and vascular cell adhesion molecule-1, (9) which mediates tissue migration of eosinophils. Since eotaxin (10) and vascular cell adhesion molecule-1 (5) levels have been reported to be higher in EPEs than in the non-EPEs, it is reasonable to hypothesize that IL-13 plays a role in pneumothorax-associated pleural eosinophilia.
The purpose of the present study was to establish a routine model of pneumothorax-associated pleural eosinophilia. Moreover, we wished to examine the effect of IL-5 and IL-13 deficiency on this reaction. We hypothesized that after the induction of a pneumothorax, IL-5 and IL-13 knockout mice would have significantly less pleural eosinophilia than wild-type mice.
MATERIALS AND METHODS
The study protocol was approved by the Animal Care Committee of the Vanderbilt University Medical Center. Eight- to 10-week-old C57/BL6 mice of both sexes were used. Wild-type and IL-5 knockout mice were purchased from Jackson Laboratory (Bar Harbor, ME). IL-13 knockout mice have been previously described. (11)
Induction of Pneumothorax
After the mice were lightly anesthetized with isoflurane, 0.4 mL of air was injected intrapleurally using a 1-mL syringe and a 26-gauge needle. The needle was inserted immediately below the costal margin midway between midline and the anterior axillary line. The needle was inserted parallel to and immediately under the ribs to a depth of approximately 0.5 cm.
It is possible that intrapleural injection of air with the above-described technique causes lung injury and/or bleeding into the pleural cavity. The presence of blood in the pleural space may influence the degree pleural inflammation. To assess this possibility, a set of experiments was done in which pneumothorax was induced using an open technique that permits injection of air under direct observation of the lung. Using this technique, lung injury and bleeding were avoided. For surgery, mice were anesthetized by ketamine, 85 mg/kg, plus xylazine, 15 mg/kg injected IM. The skin overlying the lateral chest wall was shaved and disinfected. A 5-mm transverse skin incision 1 cm laterally to the spine was made at the xiphoid level. Fascia and muscle were retracted by a forceps, and 0.4 mL of air was injected into the pleural cavity through an intercostal space under direct observation. The skin was dosed using a suture. The animals were breathing spontaneously when they were anesthetized. To assess the role of IL-5 and IL-13 in the pneumothorax-associated eosinophilia in our model, we injected air intrapleurally to IL-5 knockout, IL-13 knockout, and wild-type mice.
Assessment of the Pleural Inflammation
Wild-type mice were killed at 30 min, 12 h, 24 h, 48 h, 72 h, and 7 days after the injection. Control mice received no injection but were anesthetized with isoflurane in order to rule out any possible effect of the drug on pleural eosinophil accumulation. The mice injected with air using the open technique (n = 8) and their matched controls injected with the blind technique (n = 6) were killed at 48 h, since in that time the maximum pleural eosinophilia was observed. Five IL-5 knockout, five IL-13 knockout, and five wild-type control animals were killed at 24 h. Six IL-5 knockout, seven IL-13 knockout, and eight wild-type control animals were killed at 48 h. The mice were killed by carbon dioxide asphyxiation. Immediately after death, the peritoneal cavity was opened and pleural lavage (PL) was performed through the diaphragm with 1 mL of saline solution containing 10 IU of heparin. PL samples contaminated with blood were excluded from analysis. PL nucleated cell counts were measured with an automatic cell counter (Coulter Electronics; Luton, UK). Two independent observers blinded to the treatment group performed PL differential cell counts by manually counting 500 cells in Wright-stained cytospins. The average values are reported.
Statistical Methods
Since data were found to be normally distributed, results are reported as mean [+ or -] SEM. To assess the significance of the difference between two groups, we used the unpaired t test. To assess the significance of the difference between more than two different groups, we used the one-way analysis of variance test. The post hoc Bonferroni test was used to assess the significance of the difference between the means in the individual groups. A p < 0.05 was considered significant.
RESULTS
Macroscopical Effects of Intrapleural Injection of Air
Most of the mice treated with the blind technique and all the mice treated with the open technique recovered from anesthesia and survived with no problem until death. These mice had no distress, and their activity was similar to that of the control mice that received only anesthesia. Twelve of the 137 mice injected with the blind technique died within the first 5 min after the injection. All of the mice that died had nasal bleeding, which is suggestive of lung trauma. At autopsy, 10 mice had large hemopneumothorax and 2 mice had tension pneumothorax.
Small pneumothoraces were evident before PL in every mouse of the "30-min" and the "12-h" groups and 9 of the 13 mice of the "24-h" group. Pneumothorax was not evident in mice killed at 48 h or later. No pleural fluid was visible through the diaphragm in any animal.
Effects of Pneumothorax in PL Cells
PL of the untreated mice contained mainly mononuclear cells (mesothelial cells and macrophages), some lymphocytes, and a very low number of neutrophils and eosinophils. The intrapleural injection of air led to an increase in the number of PL total cells (p < 0.001), PL eosinophils (p < 0.001), neutrophils (p < 0.001), lymphocytes (p = 0.001), and mononuclear cells (p < 0.001) [Table 1]. The number of eosinophils started to increase 30 min and peaked 48 h after the induction of pneumothorax (Table 1). The highest mean [+ or -] SEM percentage of PL eosinophils was observed at 48 h (30.9 [+ or -] 3%). The highest individual percentage of PL eosinophils (53%) was also observed in an animal of the "48-h" group. Neutrophils increased more rapidly (peaked at 12 h) and started to decrease earlier than eosinophils. At 48 h, the number of neutrophils was lower than the number of eosinophils. The highest mean [+ or -] SEM percentage of PL neutrophils was observed at 12 h (48.5 [+ or -] 2%). The highest individual percentage of PL neutrophils (65.2%) was also observed in animals of the 12-h group.
Comparison of PL Cells Between Mice Injected With the Blind and the Open Techniques
The number of PL eosinophils of mice injected using the open technique did not differ significantly from the number of PL eosinophils of the matched control mice injected using the blind technique (Table 2). There was no significant difference in total PL cells, neutrophils, lymphocytes, and mononuclear cells between mice treated with the two different techniques.
Comparison of PL Cells Between Wild-Type and Knockout Mice
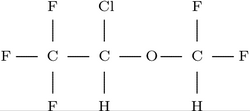
IL-5-knockout mice had fewer PL eosinophils than wild-type or IL-13 knockout mice, both at 24 h (150 [+ or -] 46/[micro]L, 903 [+ or -] 244/[micro]L, and 912 [+ or -] 168/[micro]L, respectively, p = 0.013; Fig 1) and 48 h (181 [+ or -] 45/ [micro]L, 1,587 [+ or -] 212/[micro]L, and 1,379 [+ or -] 364/[micro]L, respectively, p = 0.003; Fig 1). Post hoc analysis showed that the IL-5 knockout mice had significantly fewer PL eosinophils than the wild-type mice both at 24 h (p = 0.029) and 48 h (p = 0.003). Similarly, the IL-5 knockout mice had significantly fewer PL eosinophils than the IL-13 knockout mice at 24 h (p = 0.027) and 48 h (p = 0.015). The number of PL eosinophils did not differ significantly between wild-type and IL-13 knockout mice at 24 h or 48 h (p > 0.05). The number of the PL total cells, mononuclear cells, lymphocytes, and neutrophils did not differ between the three groups (Table 3).
[FIGURE 1 OMITTED]
DISCUSSION
In the present study, we established a murine model of pneumothorax-associated eosinophilia and we examined the role of IL-5 and IL-13 in this reaction. Our main findings were as follows: (1) The induction of a pneumothorax is followed by a pleural inflammatory response that is characterized by a large increase in eosinophils and neutrophils. The number of eosinophils increased gradually and peaked 48 h after the intrapleural injection of air. The number of neutrophils peaked earlier (at 12 h) and remained elevated for a shorter period of time than the eosinophils. (2) IL-5 knockout mice had significantly less PL eosinophilia than wild-type mice, 24 h and 48 h after the introduction of pneumothorax. PL eosinophilia did not differ between IL-13 knockout and wild-type mice. The neutrophilic influx was not affected by the absence of either IL-5 or IL-13.
Pleural injury resulting from the presence of intrapleural air and/or blood is the most common cause of EPE. (1) These EPEs are usually self-limited but may persist for weeks or months. (12,13) The optimal management of the patients with persistent posttraumatic EPE is unknown, and the efficacy of any treatment has not been proven. Similarly, the optimal treatment of the so-called "idiopathic" EPE, which may account for up to 30% of EPEs, (1) is not established. An animal model of eosinophilic pleural inflammation as a consequence of pleural injury provides the opportunity to study the pathogenesis of pleural eosinophilia, which in turn may lead to the development of specific treatments.
We created a murine model of pleural eosinophilia that follows pneumothorax. Using a very simple technique, we were able to create a pneumothorax consistently as evidenced by the presence of air in the pleural space in every mouse killed at 12 h or earlier. The air was subsequently absorbed. The main feature of pneumothorax-associated pleural inflammation was a striking increase of eosinophils and neutrophils. Eosinophils and neutrophils started to accumulate in the pleura/cavity as early as 30 min after the intrapleural injection of air. Neutrophils increased to reach a maximum at 12 h (900 times higher than the control) and remained at high levels for 24 h after the induction of pneumothorax. Eosinophils increased gradually to reach a maximum (700 times higher than the control) at 48 h. A much smaller increase of PL lymphocytes with a maximum at 24 h (threefold the control) and mononuclear cells with a maximum at 48 h (fourfold the control) was also observed. A week after the induction of pneumothorax, the PL cellular composition had returned to the baseline.
The presence of blood in the pleural cavity may also cause pleural eosinophilia. (14) It was thus important to examine whether PL eosinophilia in our model was due to accidental trauma and bleeding that may have occurred during the blind intrapleural injection of air. For this reason, we performed a set of experiments using an open technique that offered direct view of the lung when air was injected intrapleurally. This open technique practically rules out the occurrence of lung trauma and bleeding in the pleural cavity. We showed that the degree of PL eosinophilia did not differ between mice injected with either the blind or the open techniques. This observation adds further support to the concept that air alone is sufficient to attract eosinophils into the pleural cavity.
The model described in the present study closely mimics the pleural inflammatory response that accompanies pneumothorax in humans. Smit and co-workers (6) examined the PL from patients with primary spontaneous pneumothorax who underwent thoracoscopy; they found that during the first 24 h after the onset of the symptoms, neutrophils were the dominant cell population in the pleura/cavity. A few eosinophils were also present. During the following days, the neutrophil percentage decreased while the eosinophil percentage increased. In a recent study, De Smedt and coworkers (15) showed that PL from patients with spontaneous pneumothotax contained an increased number of cells in comparison to PL obtained from healthy subjects. In agreement with our observations, eosinophils and neutrophils were more strikingly increased. The duration of pneumothorax correlated with the degree of PL eosinophilia, which agrees with our observation that the accumulation of eosinophils is a relatively late and sustained aspect of the pleural inflammatory reaction caused by pneumothorax.
The observation that pleural eosinophilia can be associated with pneumothorax is not new. (6,16,17) However, the pathogenesis of the pleural eosinophilia has been poorly understood. We and others (5,6,18) have shown that in humans, pleural fluid IL-5 levels are higher in eosinophilic than in noneosinophilic pleural effusions. This finding was merely suggestive of a role for IL-5 in pleural eosinophilia. The present study is the first to confirm that IL-5 is actually necessary for the development of pneumothorax-associated pleural eosinophilia. In the absence of IL-5, the recruitment of eosinophils into the pleural cavity after the induction of a pneumothorax was almost completely inhibited. Similarly, it has been shown that mice lacking IL-5 fail to develop blood and tissue eosinophilia in response to a parasitic infection (19) or to an allergen challenge. (20) However, it is noteworthy that in our model, PL eosinophilia was not completely abolished in the absence of IL-5. This observation suggests that although IL-5 plays a major role in the development of pneumothorax-associated pleural eosinophilia, alternative mechanisms can also induce the accumulation of the eosinophils in the pleural cavity. The results of the present study combined with the data showing elevated pleural fluid levels of IL-5 in patients with EPE (5,6,18) suggest that IL-5 is a key mediator for the development of pneumothorax-associated EPE as well as other EPEs. Thus, it is possible to speculate that IL-5 blocking strategies may prove useful in the treatment of persistent EPE. However, caution is needed when extrapolating findings from animal models to human disease.
The possible contribution of IL-13, a Th2 cytokine, to the accumulation of eosinophils in the pleural cavity has not been previously examined. In our model, the eosinophil accumulation into pleural cavity was not affected by deletion of IL-13, suggesting that pneumothorax-associated pleural eosinophilia is not mediated by IL-13. The significance of IL-13 for the development of tissue eosinophilia is not consistent across different models. Intratracheal administration of IL-13 induced pulmonary eosinophilia in naive mice. (21) Furthermore, blockade of the IL-13 receptor abrogated parasite-induced pulmonary eosinophilia (22) and attenuated bronchial eosinophilia caused by inhalational challenge in asthmatic mice. (23) However, another group (24) showed that IL-13-induced pulmonary eosinophilia in mice is markedly reduced in the absence of IL-5 and eotaxin, suggesting that IL-13 is not a crucial mediator of eosinophil accumulation in lung tissue. The findings in the latter study are in agreement with our findings that IL-5, but not IL-13, is a major contributor in the development of pneumothorax-associated pleural eosinophilia. It should be also noted that IL-4, which is the prototypic cytokine of Th2-mediated eosinophilic inflammation, was not detectable in postcoronary-artery bypass surgery EPE (5) and posttraumatic EPE. (25) The observations that IL-13, another Th2 cytokine, is not necessary for eosinophil infiltration of the pleura caused by pneumothorax, coupled with the evidence that IL-4 is not important in pleural eosinophilia, suggests that pleural fluid eosinophilia associated with pleural injury is not regulated by a Th2-dependent immunologic mechanism.
When one attempts to extrapolate the results of the present study to human EPEs, a possible criticism of our model is the absence of macroscopically visible pleural effusions. However, a pleural effusion is not commonly observed in various murine models of eosinophilic pleuritis, and PL is required to assess the inflammatory response. (26) Even in humans, the occurrence of pneumothorax-associated eosinophilic infiltration is much more common than the he development of EPE. (16,17) Nevertheless, it is reasonable to assume that pleural fluid production in clinical EPE is due to the inflammatory reaction in the pleura characterized by the increased number of eosinophils.
In conclusion, the present study provides for the first time direct proof that intrapleural air initiates an inflammatory reaction mainly characterized by an influx of eosinophils and neutrophils into the pleural cavity. Pleural eosinophilia was markedly reduced in mice lacking IL-5 but was not affected in mice lacking IL-13. Our results suggest that IL-5 but not IL-13 is required for the development of pneumothorax-associated pleura] eosinophilia in mice and possibly EPE in humans.
Manuscript received February 6, 2004; revision accepted March 28, 2005.
REFERENCES
(1) Kalomenidis I, Light RW. Eosinophilic pleural effusions. Curr Opin Pulm Med 2003; 9:254-260
(2) Rothenberg ME. Mechanisms of disease: eosinophilia. N Engl J Med 1998; 338:1592-1600
(3) Zangrilli JG. Regulation of eosinophil viability by cytokines. Am J Respir Cell Mol Biol 2002; 26:388-390
(4) O'Byrne PM, Wood L. Interleukin-5 and allergic inflammation. Clin Exp Allergy 1999; 29:573-575
(5) Kalomenidis I, Mohamed KH, Lane KB, et al. Pleural fluid levels of vascular cell adhesion molecule-1 are elevated in eosinophilic pleural effusions. Chest 2003; 124:159-166
(6) Smit HJ, van den Heuvel MM, Barbierato SB, et al. Analysis of pleural fluid in idiopathic spontaneous pneumothorax: correlation of eosinophil percentage with the duration of air in the pleural space. Respir Med 1999; 93:262-267
(7) Wills-Karp M, Chiaramonte M. Interleukin-13 in asthma. Curr Opin Pulm Med 2003; 9:21-27
(8) Li L, Xia Y, Nguyen A, Lai YH, et al. Effects of Th2 cytokines on chemokine expression in the lung: IL-13 potently induces eotaxin expression by airway epithelial cells. J Immunol 1999; 162:2477-2487
(9) Sironi M, Sciacca FL, Matteucci C, et al. Regulation of endothelial and mesothelial cell function by interleukin-13: selective induction of vascular cell adhesion molecule-1 and amplification of interleukin-6 production. Blood 1994; 84: 1913-1921
(10) Yokoyama A, Kohno N, Ito M, et al. Eotaxin levels in pleural effusions: comparison with monocyte chemoattractant protein-1 and IL-8, Intern Med 2000; 39:547-552
(11) Herrick CA, Xu L, McKenzie AN, et al. IL-13 is necessary, not simply sufficient, for epicutaneously induced Th2 responses to soluble protein antigen. J Immunol 2003; 170: 2488-2495
(12) Ishiura U, Fujimura M. Intrapleural corticosteroid injection therapy for post-traumatic eosinophilic pleural effusion. Respir Med 1996; 90:501-503
(13) Maltais F, Laberge F, Cormier Y. Blood hypereosinophilia in the course of posttraumatic pleural effusion. Chest 1990; 98:348-351
(14) Chapman JS, Reynolds R. Eosinophilic response to intraperitoneal blood. J Lab Clin Med 1958; 51:516-520
(15) De Smedt A, Vanderlinden E, Demanet C, et al. Characterization of pleural inflammation occurring after primary spontaneous pneumothorax. Eur Respir J 2004; 23:896-900
(16) Askin FB, McCann BG, Kuhn C. Reactive eosinophilic pleuritis: a lesion to be distinguished from pulmonary eosinophilic granuloma. Arch Pathol Lab Med 1977; 101:187-191
(17) Luna E, Tomashefski JF Jr, Brown D, et al. Reactive eosinophilic pulmonary vascular infiltration in patients with spontaneous pneumothorax. Am J Surg Pathol 1994; 18:195-199
(18) Taniguchi H, Mukae H, Matsumoto N, et al. Elevated IL-5 levels in pleural fluid of patients with Paragonimiasis westermani. Clin Exp Immunol 2000; 123:94-98
(19) Kopf M, Brombacher F, Hodgkin PD, et al. IL-5-deficient mice have a developmental defect in CD5+ B-1 cells and lack eosinophilia but have normal antibody and cytotoxic T cell responses. Immunity 1996; 4:15-24
(20) Foster PS, Hogan SP, Ramsay AJ, et al. Interleukin-5 deficiency abolishes eosinophilia, airways hyperactivity and lung damage in a mouse asthma model. J EXP Med 1996; 183:195-201
(21) Kibe A, Inoue H, Fukuyama S, et al. Differential regulation by glucocorticoid of interleukin-13-induced eosinophilia, hyperresponsiveness, and goblet cell hyperplasia in mouse airways. Am J Respir Crit Care Med 2003; 167:50-56
(22) Chiaramonte MG, Schopf LR, Neben TY, et al. IL-13 is a key regulatory cytokine for Th2 cell-mediated pulmonary granuloma formation and IgE responses induced by Schistosoma mansoni eggs. J Immunol 1999; 162:920-930
(23) Taube C, Duez C, Cui ZH, et al. The role of IL-13 in established allergic airway disease. J Immunol 2002; 169: 6482-6489
(24) Pope SM, Brandt EB, Mishra A, et al. IL-13 induces eosinophil recruitment into lung by an IL-5 and eotaxin-dependent mechanism. J Allergy Clin Immunol 2001; 108: 594-601
(25) Schandene L, Namias B, Crusiaux A, et al. IL-5 in post-traumatic eosinophilic pleural effusion. Clin Exp Immunol 1993; 93:115-119
(26) Lee YCG. Experimental models in pleural disease. In: Light RW, Lee YCG, eds. Textbook of pleural diseases. London, UK: Arnold. 2003; 149-166
This work was presented in part at CHEST 2003, Orlando, FL, October 2003.
Supported by the Saint Thomas Foundation, Nashville, Tennessee and "Thorax" Foundation, Athens, Greece.
* From "Marianthi Simou" Laboratory (Drs. Kalomenidis and Papiris), Department of Critical Care and Pulmonary Services, Athens Medical School, "Evangelismos" Hospital, Athens, Greece; Department of Respiratory and Critical Care Medicine (Dr. Guo), First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China; Pulmonary Medicine Department (Dr. Light), Saint Thomas Hospital, Department of Allergy, Pulmonary and Critical Care Medicine (Drs. Lane and Perebles), Vanderbilt University, Nashville, TN; and Section of Pulmonary and Critical Care Medicine (Dr. Elias), Department of Internal Medicine, Yale School of Medicine, New Haven, CT.
Correspondence to: Ioannis Kalomenidis, MD, Department of Critical Care and Pulmonary Services, Athens Medical School, "Evangelismos" Hospital, 45-47 Ipsilandou Str., 10675 Athens, Greece; e-mail: jkalomenidis@hotmail.com
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group