Hypothesis: Human albumin may be effective in the treatment of posttraumatic brain edema due to its hyperoncotic features. Therefore, the aim of the experimental study presented in this paper has two points: the first is to evaluate the efficacy of intraventricular hyperoncotic human albumin on post-traumatic brain edema and the second is to try to show the appropriate posttraumatic time window for albumin administration.
Method: Traumatic brain injury and subsequent edema was formed by a model of impact acceleration injury in rats. Human albumin was administered via intraventricular route by using a stereotactic head holder. All animals in each group were decapitated 24 hours after the procedure and the effect of albumin was evaluated by measurement of tissue specific gravity.
Results: Tissue specific gravity decreased in edematous tissue (trauma indicator), increased after albumin administration at the 12th (p
Conclusion: We conclude that human albumin is effective in cytotoxic, but not in vasogenic edema and exerts its best anti-edematous effect at the 12th hour of severe head trauma and this study may help future studies that will try to show the effects of albumin with different time modalities after severe head injury. [Neurol Res 2005; 27: 67-72]
Keywords: Albumin; brain edema; head trauma
INTRODUCTION
Formation of the brain edema after the head trauma is one of the most crucial and challenging problems encountered in neurosurgical practice. Due to its high morbidity and mortality rates, many efforts have been made by the physicians for the best treatment modalities for the several years1-8. Mannitol is the most popular hyper-osmotic agent used in post-traumatic brain edema. It has been shown that mannitol, by creating an osmotic gradient between the brain tissue and plasma, leads the edema fluid to flow into the vascular bed. In addition, by producing hemodilution and red cell deformity, mannitol increases blood flow to the tissues and reduces cerebrospinal fluid release from the choroids plexus5,9. One of the most effective methods for decreasing the increased intracranial pressure (ICP) is the external ventricular drainage by the insertion of a catheter directly into the lateral ventricles. Barbiturates and hyperventilation may be used for a limited period of time10,11 and use of steroids as a membrane stabilizer is still under investigation. In spite of all the treatment modalities mentioned above, treatment of post-traumatic brain edema remains as a challenging problem. In recent years, there have been tendencies to administer hyperoncotic agents in clinical trials for the treatment of post-traumatic brain edema.
To the best of our awareness, no previous studies have evaluated the efficacy of intraventricular hyperoncotic human Alb on both vasogenic or cytotoxic brain edemas secondary to severe head injury (SHI), and have showed proper post-traumatic time for AIb administration. The experimental study reported here is a preliminary work that aimed to evaluate the effects of intraventricular administration of AIb in vasogenic and cytotoxic brain edemas, and tried to demonstrate the appropriate post-traumatic time for AIb administration.
MATERIALS AND METHODS
The animal protocols of this experimental study were approved by Istanbul University Animal Care and Use Committee. For the study, 64 male adult Sprague-Dawley rats, each weighing 300-400 g served as a subject and divided arbitrarily into eight groups with the equal number in each:
* control (C);
* trauma (T);
* rats administered AIb at the 1st hour post-anesthesia (A^sub 1^);
* rats administered AIb at 12th hour post-anesthesia (A^sub 12^);
* rats administered AIb at both the 1st and 12th hour post-anesthesia (A^sub 1^+A^sub 12^);
* rats administered Alb at the 1st hour post-trauma (TA^sub 1^);
* rats administered Alb at the 12th hour post-trauma (TA^sub 12^);
* rats administered AIb at both the 1st and 12th hour post-trauma (TA^sub 1^+TA^sub 12^).
All the animals were free to access water and food before and after the experiments. Intubation procedure was applied to all groups except the control. The effect of intraventricular Alb administration on post-traumatic brain edema was evaluated by the tissue specific gravity measurements.
Anesthesia and trauma
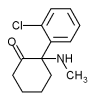
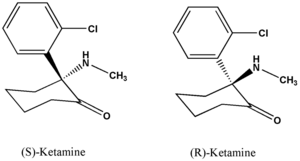
Ketamine (50 mg/kg; Ketalar-Parke Davis/Eczacibasi) was used as an anesthetic agent via intraperitoneal route. After satisfactory sedation has been achieved, respiration/pulse rates and rectal temperatures were recorded at the beginning of the experiment (zero hour). Blood samples were taken from the femoral artery to determine pH, pO^sub 2^, pCO^sub 2^, Na+, P^sup +^, Cl-, glucose and hematocrit levels, and these measurements were also repeated after 1 hour and all the results were recorded. All the animals were still anaesthetized and/or were unconscious when the 1-hour blood gas/electrolyte analysis was performed.
The groups that were subjected to trauma were intubated and put into prone position. A midline vertical skin and periosteal incisions were made to expose the bregma and lambdoid sutures. A steel disc 10 mm in diameter and 3 mm in thickness was placed between the coronal and lambdoid sutures. Then the rats were placed in a prone position on foam rubber 12 × 12 × 43 cm and the severe head trauma was performed according to the principles described by Marmarou et al.12 Immediately after the trauma, the rats were ventilated by a ventilator (Harward Rodent ventilator Model 683, USA) until the vital signs returned to normal. The animals needed one-and-a-half hour to wake up after anesthesia.
Intraventricular albumin administration
A stereotactic frame (Stoelting Co-Stellar Cat No. 51400-USA) was used for intraventricular AIb administration. The rats were placed so that the incisor bar was 5 mm above the inter-aural line. A 1-mm hole was made with a dental drill positioned 0.92 mm behind the bregma and 1.5 mm lateral to the midline. Then, 2 µl of hyperosmolar AIb solution (human albumin 20%, 200 'Dessau' Italy) was injected into the left lateral ventricle by a 24 G Hamilton syringe according to the coordinates described by Pellegrino and Cushman13. Fractions of 0.2 µl were given at 25-second intervals. In order to prevent the reflux of the solution, the syringe was kept in place for a period of no less than 120 seconds before removal. Alb was administered at the 1st, 12th, and both the 1st and 12th hours' post-anesthesia in groups A^sub 1^, A^sub 12^ and A^sub 1^+A^sub 12^, respectively. The same protocol was applied following the trauma in the groups TA^sub 1^, TA^sub 12^ and TA^sub 1^+^sub 12^, respectively. All of the subjects whether they were traumatized or not were anesthetized, and decapitated at the 24th hour after the procedure.
Methods for evaluation (tissue specific gravity)
A gravity column prepared by a mixture of bromobenzene and kerosene was used for determination of the specific gravity of the brain samples. Tissue samples with a volume of 1 mm3 were taken from the highest points of both parietal cortex and dropped into the gravity column, and the values on the scale were noted at the end of 3 minutes. The values were placed into the specific gravity curve to calculate the averages8.
Statistical analysis
Tissue specific gravity values were evaluated by ANOVA and Tukey's method of post-ANOVA tests and all p-values less than 0.05 were accepted as statistically significant.
RESULTS
The mean values±standard deviations of physiological and biochemical parameters obtained at the beginning (zero hour) and 1st hour of the procedure in each group are shown in Tables 1 and 2, respectively. As shown in the tables there are no significant statistical differences between the groups regarding the parameters (p>0.05). The results of tissue specific gravity measurements of each group are shown in Figure 1. This study showed that trauma decreased the tissue specific gravity, and the comparison of the values of the 'C and T' groups revealed a statistically significant difference (p
Tissue specific gravity measurements demonstrate a similar value of statistical significance between 'TA^sub 1^' and 'T' groups (p>0.05). A more remarkable result has been obtained in the comparison of tissue specific gravity values of both TA^sub 12^ and TA^sub 1+12^' and 'T' groups (p
Tissue specific measurements demonstrate a similar value of statistical significance between the groups without trauma (A^sub 1^, A^sub 12^, A^sub 1+12^) and the 'T' group, but were dissimilar when compared with the 'C' group. This result indicates that when AIb is administered in the absence of trauma, it causes the formation of edema.
DISCUSSION
A variety of experimental and/or clinical studies addressing the treatment of post-traumatic brain edema after traumatic brain injury have been performed over the years, and the encouraging results have gained importance to the neurosurgeons as the best treatment of post-traumatic edema9.14-17 Widely held therapeutic modalities stated in the literature have an acceptable risk of complications and limitations of use17-21.
Contribution of the brain swelling to post-traumatic edema is a major problem and accordingly increased ICP causes death at the same time as disastrous complications. It has been revealed that post-traumatic brain edema may be divided into two major categories according to its mechanisms of formation: vasogenic and cytotoxic edema7,18,20,22,23.
However, no clear-cut post-traumatic time between vasogenic and cytotoxic edema after trauma has been yet stated, and it is important to understand the sequence of pathophysiological events leading to brain swelling for the best treatment of severe traumatic brain edema. To help resolve these issues, a variety of studies addressing the type and contribution of edema to the brain swelling after SHl has been performed. By using impact-acceleration brain injury model in rats, Barzo ef al.4 showed that there is biphasic pathophysiological response to SHI. It was found that animals had a significant increase in apparent diffusion coefficient (ADCs) within the first 60 minutes post-injury, followed by a decrease in ADC that had begun 40-60 minutes post-injury and reached a minimum on days 7-14. These finding were also supported by a previous study in which the BBB permeability was tested by using contrast-enhanced MR imaging, which showed the BBB opens immediately after the trauma and approaches closure approximately 30-60 minutes post-injury3. Besides, evidence from other previous studies using different models of head injury supported the notion that the BBB leakage reaches a peak level within 30 minutes following trauma24-27. This short duration of edema is followed by a late edema that begins a few hours postinjury, and has a maximum effect between 3 and 8 days after trauma24,28-32. It now becomes clear from the current literature that SHI is associated with biphasic pathophysiological response, namely the first and short duration of vasogenic, and the second, the prolonged cytotoxic edema. The results of such studies have led the clinicians to scrutinize the current treatment modalities and timing of administration of the antiedematous agents during the post-traumatic period.
Relying on the observations of those studies stated above, we administered human AIb by intraventricular route at the 1st and 12th hours of the trauma for evaluating the effect on vasogenic and cytotoxic edema, respectively. Our results provided that human Alb administered in early period after SHl (within 1st hour) has no effect, namely on vasogenic edema, however, is effective in late period (at 12th hour) of the trauma, that is, in cytotoxic edema.
Experimental studies
Recently, the valuable effect of AIb in the posttraumatic brain edema, particularly in vasogenic stage, has been shown by applications either intravenously or directly into the neural parenchyma8,9,17,33-38. Highdose human AIb has been shown to be neuroprotective in experimental models of both transient global ischemia55 and fluid-percussion traumatic brain injury34. In rat fluid percussion injury model, Belayev ef al.33 showed that intravenous administration of Alb shortly after acute traumatic brain injury causes reduction in histopathological damage and improves neurological deficit due mainly to its hemodilating effect. Furthermore, in recent experimental studies of focal cerebral ischemia models, it has been shown that AIb therapy, if administered promptly after stroke onset, is highly effective in terms of reducing infarction volume and extends of the brain swelling 9,29,39,40. Diffusionweighted magnetic resonance imaging studies in rats showed Alb also normalizes the ADCs of water, even in zones of residual histological injury40,41 A preliminary experimental work performed by focal freeze injury in rats revealed the early administration of hyperosmolar human Alb into the ventricles has decreased the vasogenic brain edema17 Majority of experimental studies concerning the therapeutic effect of human Alb in brain injury have used different injury models including the widely used fluid-percussion injury, focal freeze injury. Results of these models, due to the focal nature of the lesions produced have been criticized because of their inability to produce diffuse axonal injury seen in man4,12 The experimental diffuse brain injury identical to that occurring in man has been produced by impact-acceleration injury model proposed by Marmarou et al12 Therefore, this is the main reason why we used this model in the study presented here.
Clinical applications
Alb therapy has, to date, been practiced for a variety of clinical conditions. For stroke, it caused reduction in mortality rate of more than 10%42. AIb is being commonly applied to the patients after surgical clipping of intracranial aneurysm, in an effort to prevent delayed ischemia and brain edema due to vasospasm43. In another study, Alb was administered in moderate to high doses over a 2-week period after trauma in patients with brain contusions; it reduced contusional edema effectively44. Similarly, patients with putaminal hemorrhage treated with Alb disclosed reductions of cerebral edema45. Cirrhosis and spontaneous bacterial peritonitis are two other clinical entities in which AIb showed reduction in renal impairment and lowered the mortality rate46. Taken together, those observations mentioned above support the notion that human AIb has neuroprotective effect and potential clinical feasibility of use.
Data analysis
This is the first study that evaluates the therapeutic effect of hyperoncotic human AIb on both vasogenic and cytotoxic brain edemas, and defines the therapeutic window following SHI. Moreover, we have demonstrated for the first time that intraventricular hyperoncotic AIb therapy after SHl is effective in cytotoxic edema. Since the experimental impact acceleration traumatic brain injury models discovered that the brain edema reaches its maximum stage at the 24th hour of trauma and human AIb shows its maximum effect at the 12th hours after administration5'29'47, we thought that it would be appropriate to administer AIb at the 1st and 12th hours, and the tissue specific gravities must be evaluated at the 24th hour of the trauma.
The similar specific gravity measurements of the samples taken from the right and left hemispheres indicated that the trauma was diffuse. A comparison of tissue specific gravity measurements of the 'C' and T' groups displayed that the trauma increases water content, while decreasing the tissue specific gravity. This statistically significant difference pointed out the development of the brain edema.
Tissue specific gravity measurements of 'C' and 'TA^sub 12^' groups established nearly similar values. Adding together, it appears that 'TA^sub 12^' is effective than 'TA^sub 1+12^' when compared to group 'C'. These results support the hypothesis that the edema fluid moves from the injury site towards the ventricles and subarachnoid space as a bulk flow in agreement with pressure gradients23,47. Taken in concert, these findings provide compelling evidence that AIb has no therapeutic effect when administered at the 1 st hour of the trauma and the majority of anti-edema effect of AIb was obtained when administered at the 12th hour.
Specific gravity measurements of 'A1', 'A^sub 12^' and 'T' groups confirmed similar marginal value of statistical significance. The measurements of 'A^sub 1^' and 'A^sub 2^' showed statistically significant difference than 'C', but not those of T'. Such results have forced us to conclude that Alb administrations in the absence of trauma have caused the development of edema. The possible explanation of why AIb causes edema in the absence of trauma may be owing to the lack of some mechanisms and the CSF-brain barrier in the mature brain, which allows Alb to gain access to the brain parenchyma from the ventricles2,48,49.
CONCLUSION
In summary, the present study has revealed that human AIb therapy has obvious anti-edema effect and is effective in cytotoxic brain edema. AIb, even in single dose, exerts its maximum effect when administered at the 12th hour of the trauma. We therefore suggest that this agent offers a great promise in the therapy of posttraumatic brain edema. However, studies that are more experimental will be required before a clinical application can be considered.
REFERENCES
1 Albright AL, Latchaw RE, Robinson AG. lntracranial and systemic effects of osmotic and oncotic therapy in experimental cerebral edema. J Neurosurg 1984; 60: 481-489
2 Balslev Y, Saunders NR, Mollgard K. The surface CSF-brain barrier in the developing rat brain. j Neurocytol 1997; 26: 133-148
3 Barzo P, Marmarou A, Fatouros P, Corwin F, Dunbar. Magnetic resonance imaging-monitored acute blood-brain barrier changes in experimental traumatic brain injury. J Neurosurg 1996; 85: 1113-1121
4 Barzo P, Marmarou A, Fatouros P, Hayasaki K, Corvin F. Contribution of vasogenic and cellular edema to traumatic brain swelling measured by diffusion-weighted imaging. J Neurosurg 1997; 87: 900-907
5 Bogaert YE, Rosenthal RE, Fiskum C. Postischemic inhibition of cerebral cortex pyruvate dehydrogenase. Free Radie Biol Med 1998; 16: 811-820
6 Bullock R, Maxwell WL, Graham Dl, Teasdale GM, Adams JH. Glial swelling following human cerebral contusion: an ultrastructural study. ] Neurol Neurosurg Psychiatry 1991; 54: 427-434
7 Miller JD, Becker DB, Ward JD, Sullivan HG, Adams WE, Rosner MJ. Significance of intracranial hypertension in severe head injury. J Neurosurg 1 977; 47: 503-51 6
8 Tomita H, lto U, Tone O, Masaoka H, Tominaga B. High colloid oncotic therapy for contusional brain edema. Acta Neurochir Suppl (Wien) 1994; 60: 547-549
9 Belayev L, Liu Y, Zhao W, Busta R, Ginsberg MD. Human albumin therapy of acute ischemie stroke. Marked neuroprotective efficacy of moderate doses and with a broad therapeutic window. Stroke 2001; 32: 553-563
10 Popp AJ, Feustel PJ, Kimelberg HK. Pathophysiology of traumatic brain injury. In: Wilkins RH, Rengachary SS, eds. Neurosurgery, vol MB. New York: McGraw Hill, 1996; 2623-2637
11 Rea G, Rockwold G. Barbiturate therapy in uncontrolled intracranial hypertension. Neurosurgery 1983; 12: 401-404
12 Marmarou A, Foda MA, Van Den Brink W, Campdell J, Kita H, Demetriadou K. A new model of diffuse brain injury in rats. Part I. Pathophysiology and biomechanics. J Neurosurg 1994; 80: 291-300
13 Pellegrino LJ, Pellegrino AS, Cushman AJ. A Stereo Tactic Atlas of the Rat Brain. New York: Plenum Press, 1979
14 Berger S, Schurer L, Hartl R, Messmer K, Baethmann A. Reduction of post-traumatic intracranial hypertension by hypertonic/hyperoncotic saline/dextran and Hypertonie mannitol. Neumsurgery 1995; 37: 98-108
15 Feldman Z, Zachari S, Reichenthal E, Artru AA, Shapira Y. Brain edema and neurological status with rapid infusion of Lactated Ringer's or 5% dextrose solution following head trauma. Neurosurg 1995; 83: 1060-1066
16 Hansen DT, Warner DS, Traynelis VC, Todd MM. Plasma osmolality and brain water content in a rat glioma model. Neumsurgery 1 994; 34: 505-511
17 Onal C, Unal F, Turanian Ml, Uzürn G, Hasanoglu A, Kaynar MY. The effect of intraventricular albumin in experimental brain edema. Acta Neumchir (Wien) 1997; 139: 661-669
18 Hariri RJ. Cerebral edema. Neurosurg CHn N Am 1994; 5: 687-706
19 Hartwell RC, Sutton LN. Mannitol, intracranial pressure, and vasogenic edema. Neumsurgery 1993; 32: 444-450
20 Kimelberg HK. Current concepts of brain edema. Review of laboratory investigations. J Neurosurg 1995; 83: 1051-1059
21 Pollay M. Blood-brain: cerebral edema. In: Wilkins RH, Rengachary SS, eds. Neumsurgery, vol I. New York: McGraw Hill, 1985; 322-331
22 Halliwell B, Gutteridge JM. The antioxidants of human extracellular fluids. Arch Biochem Biophys 1990; 280: 1-8
23 Reulen HJ, Graham R, Spatz M, Klatzo I. Role of pressure gradients and bulk flow in dynamics of vasogenic brain edema. J Neurosurg 1977; 46: 24-35
24 Bullock R, Statham P, Patterson J. The time course of vasogenic oedema after focal human head injury-evidence from SPECT mapping of blood brain barrier defects. Acta Neumchir Suppl 1990; 51: 286-288
25 Nawashiro H, Shima K, Chigasaki H. Blood-brain barrier, cerebral blood flow, and cerebral plasma volume immediately after head injury in the rat. Acta Neumchir Suppl 1994; 60: 440-442
26 Povlishock JT, Becker DP, Miller JD, Jenkins LW, Dietrich WD. The morphopathological substrates of concussion? Acta Ncuropathol 1979; 47: 1-11
27 Povlishock JT, Becker DP, Sullivan HG. Vascular permeability alterations to horseradish peroxidase in experimental brain injury. Brain Res 1978; 153: 223-239
28 Katayama Y, Becker DP, Tamura T, Ikezaki K. Early cellular swelling in experimental traumatic brain injury: a phenomenon mediated by excitatory amino acids. Acta Neumchir Suppl 1990; 51: 271-273
29 Kcttenmann H, Schachncr M. Pharmacological properties of gamma aminobutyric acid-glutamate-, and aspartate-induced depolarization in cultured astrocytes. J Neumsci 1985; 5: 3295-3301
30 Kita H, Marmarou A. The cause of acute brain swelling after the closed head injury in rats. Acta Neumchir Suppl 1994; 60: 452-455
31 Tanno H, Nockels RP, Pitts LH, Noble LJ. Immunolocalization of heat shock protein after fluid percussion injury and relationship to breakdown of the blood-brain barrier. J Cereb Blood Flow Metab 1993; 13: 116-124
32 Todd NV, Graham Dl. Blood-brain barrier damage in traumatic brain contusions. Acta Neumchir Suppl 1990; 51: 296-299
33 Belayev L, Alonso OF, Huh PW, Zhao W, Busto R, Ginsberg MD. Posttreatment with high-dose albumin reduces histopathological damage and improves neurological deficit following fluid percussion brain injury in rats. J Neurotrauma 1997; 16: 445-453
34 Belayev L, Saul I, Huh PW, ef ai. Neuroprotective effect of highdose albumin therapy against global ischemie brain injury in rats. Brain Res 1999; 845: 107-111
35 Cserr HF, Cooper DN, Suri PK, Patlak CS. Efflux of radiolabelled polyethylene glycols and albumin from rat brain. Am J Physiol 1981; 240: F319-F328
36 Huh PW, Belayev L, Zhao W, Busto R, Saul I, Ginsberg MD. The effect of high-dose albumin therapy on local cerebral perfusion after transient focal cerebral ischemia in rats. Brain Res 1998; 804: 105-113
37 Little JR, Slugg RM, LatchawJP, Lesser RP. Treatment of acute focal cerebral ischemia with concentrated albumin. Neurosurgery 1981; 9: 552-558
38 Matsui T, Sinyama H, Asano T. Beneficial effect of prolonged administration of albumin on ischemie cerebral edema and infarction after occlusion of middle cerebral artery in rats. Neurosurgery 1993; 33: 293-300
39 Belayev L, Busto R, Zhao W, Clemens JA, Ginsberg MD. Effect of delayed albumin hemodilution on infarction volume and brain edema after transient middle cerebral artery occlusion in rats. J Neurosurg 1997; 87: 595-601
40 Belayev L, Zhao W, Pattany PM, ef al. Diffusion-weighted magnetic resonance imaging confirms marked neuroprotective efficacy of albumin therapy in focal cerebral ischemia. Stroke 1998; 29: 2587-2599
41 Albensi BC, Knoblach SM, Chew BGM, O'Reilly MP, Faden AI, Pekar JJ. Diffusion and high resolution MRl of traumatic brain injury in rats: time course and correlation with histology. Exp Neurol 2000; 162: 61-72
42 Goslinga H, Eijzenbach V, Heuvelmans JH, ef ai. Custom-tailored hemodilution with albumin and crystalloids in acute ischemie stroke. Stroke 1992; 23: 181-188
43 Mori K, Arai H, Nakajima K, Tajima A, Maeda M. Hemorrheological and hemodynamic analysis of hypervolemic hemodilution therapy for cerebral vasospasm after aneurismal subarachnoid hemorrhage. Strode 1995; 26: 1620-1626
44 Tominaga T, Ohnishi ST. Ion movements and edema formation in CNS injury. In: Ohnishi ST, Ohnishi T, eds. Central Nervous System Trauma and Research Techniques. Boca Raton, NY: CRC, 1995; 85-94
45 Tone O, lto U, Tomita H, Masaoka H, Tominaga B. High colloid oncotic therapy for brain edema with cerebral hemorrhage. Acta Neurochir Suppl (Wien) 1994; 60: 568-570
46 Sort P, Navasa M, Arroyo V, ef a/. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med 1999; 341: 403-409
47 Groeger U, Marmarou A. The importance of protein content in the oedema fluid for the resolution of brain oedema. Acta Neurochir 1989; 101: 134-140
48 Mollgard K, Balslev Y, Lauritzen B, Saunders NR. Cell junctions and membrane specializations in the ventricular zone (germinal matrix) of the developing sheep brain: A CSF-brain barrier. J Neurocytol 1987; 26: 433-444
49 Saunders NR, Knott GW, Dziegielewska KM. Barrier mechanisms in the brain, II. Immature brain. CHn Exp Pharmacol Physiol 1999; 26(2): 85-91
Merih Is*, Mustafa Uzan[dagger], Faruk Unal3, Talat Kiris[double dagger], Taner Tanriverdi[dagger], Murat Mengi§ and Nurten Kilic¶
* Department of Neurosurgery, Medical Faculty, Duzce Izzet Baysal University, Duzce, Turkey
Departments of [dagger] Neurosurgery and § Physiology, ¶ Experimental Animal Research Laboratory, and Istanbul University, Cerrahpasa Medical Faculty, Istanbul, Turkey
[double dagger] Department of Neurosurgery, Istanbul Medical Faculty, Istanbul University, Istanbul, Turkey
Correspondence and reprint requests to: Mustafa Uzan, PO Box 5, Cerrahpasa, 34.301, Istanbul, Turkey, [uzan@istanbul.edu.tr] Accepted for publication May 2004.
Copyright Maney Publishing Jan 2005
Provided by ProQuest Information and Learning Company. All rights Reserved