Background: Fluoroquinolones are commonly used in the treatment of tuberculosis (TB) for drug-sensitive patients who are intolerant to first-line antituberculous agents or who are infected with drug-resistant organisms. Despite increasing use of these agents, there is little information on their tolerance outside of clinical trial settings.
Objectives: To compare overall rate of major adverse events associated with levofloxacin-containing regimen to standard therapy.
Methods: Cases (levofloxacin-containing regimen) were matched by age and sex to their control subjects (standard first-line TB drugs). Eligible patients were identified from the provincial TB database from 2001 to 2004. Drug safety was assessed by evaluation of the nature of the adverse event, the likelihood of association with the study medications, and severity. Only major side effects, that is, those who had a severe or moderate adverse event that was categorized to be definitely, probably, or possibly related to the TB medications, were considered for the analysis.
Results: During the 3-year study period, 102 patients received levofloxacin, and 358 patients received first-line agents for treatment of active TB. There were no significant differences between the two groups except for indication (82% of patients in the levofloxacin group had an antecedent adverse event to first-line TB drugs, whereas 18% received levofloxacin because of resistance) and concurrent use of first-line drugs (majority of patients in the levofloxacin arm were not receiving concurrent isonlazid or rifampin). The rate of any major adverse event was almost half among those using levofloxacin as among those on standard therapies (rate ratio, 0.60; 95% confidence interval [CI], 0.44 to 0.82). After adjustment for the differences in exposure of concomitant medications, the rate of any major adverse event was similar between the levofloxacin and control arms (adjusted rate ratio, 0.83; 95% CI, 0.66 to 1.03). Furthermore, there was no difference between the levofloxaeln and control arms with respect to CNS (adjusted rate ratio, 0.94; 95% CI, 0.61 to 1.43), GI tract (adjusted rate ratio, 0.81; 95% CI, 0.58 to 1.13), skin (adjusted rate ratio, 0.65; 95% CI, 0.38 to 1.10), or musculoskeletal (MSK) [adjusted rate ratio, 0.87; 95% CI, 0.48 to 1.60] related adverse events when adjusted for concomitant drugs. The results of the secondary analysis for the rate of major adverse events within the first 100 days were similar to the primary analysis. The time to the first major adverse event was similar between the levofloxacin group and the control group (adjusted hazards ratio, 1.01; 95% CI, 0.76 to 1.34).
Conclusions: Concomitant use of a levofloxacin-containing regimen resulted in a similar rate of adverse events compared with conventional first-line regimens when used for treatment of active TB, despite a history of adverse events.
Key words: adverse events; fluoroquinolones; levofloxacin; tuberculosis
Abbreviations: CI = confidence interval; CNS = central nervous system; CVS = cardiovascular; GI = gastrointestinal; MSK = musculoskeletal; TB = tuberculosis
**********
Tuberculosis (TB) accounts for 8.4 million cases worldwide and is one of the leading infectious causes of death today. (1,2) Although in North America, the overall rates of TB have declined more than 10-fold since the 1950s (from 53 per 100,000 to 5.3 per 100,000), there remain significant groups at high risk of TB disease, most notably, foreign-born individuals, who represent greater than 50% of the cases. (3) Other groups who are at high risk for developing TB disease include Aboriginal persons, high-risk inner city groups (including injection drug users and the homeless), and HIV-infected persons. (4) The treatment of drug-sensitive TB requires the use of conventional first-line agents for [greater than or equal to] 6 months. (5) Intolerance to these medications or drug-resistant disease requires the use of alternative regimens frequently containing quinolones. (6-8)
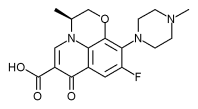
The second-generation quinolone antibiotics (ofloxacin and ciprofloxacin) have moderate in vitro activity against Mycobacterium tuberculosis, (9,10) but the activity (both in vitro and in vivo) of the newer-generation fluoroquinolones, such as levofloxacin (11,12) and moxifloxacin, is twofold to threefold greater. (13,14) Prospective clinical trims of fluoroquinolones as first-line agents for the treatment of TB are limited, and the majority of clinical data (6-8) are on their use as second-line agents, either for those patients infected with drug-resistant M tuberculosis or for those with drug-sensitive disease who are intolerant to the first-line agents. Since the introduction of levofloxacin in North America, it has become a commonly used fluoroquinolone because of its superior in vivo activity against M tuberculosis, as well as its more-convenient dosing schedule (levofloxacin is administered once daily compared with the twice-daily schedule for ciprofloxacin/ofloxacin). (15) Results from the randomized clinical trials (16) evaluating moxifloxacin for the treatment of M tuberculosis are in progress, and, as such, the use of this newer fluoroquinolone is not as prevalent as levofloxacin at the present time.
In August 2001, the TB Control Service at the British Columbia Centre for Disease Control switched from ciprofloxacin to levofloxacin for the treatment of patients with drug-resistant TB infection and for patients who had TB and were intolerant to first-line medications. In order to determine the safety of the new fluoroquinolone-containing regimen, we examined the incidence of adverse events in the levofloxacin-containing regimen vs standard regimens.
MATERIALS AND METHODS
Study Design and Database
We used a ease-control design whereby all of the cases (patients on levofloxacin) were matched by age and sex to control subjects (patients on standard first-line anti-TB agents) in a 1:4 ratio. All of the individuals identified in British Columbia with active TB disease are eligible to receive treatment through a publicly funded provincial program. The treatment of these patients is assessed and followed by the Tuberculosis Control Division within the BC Centre for Disease Control, and all of the records are kept in a central computerized database. In addition, all of the mycobacteriology is completed at the provincial laboratory, based at the Centre for Disease Control, ensuring identification of all of the eases within the province. Although the information captured within the database began in 1990, the use of fluoroquinolones for the treatment of TB was not initiated in British Columbia until 2001.
Subjects
All of the cases of active TB were confirmed by the isolation of M tuberculosis from culture. We evaluated medication records of patients who had received [greater than or equal to] 7 days of levofloxacin (with other antituberculous agents) or standard first-line treatment (ie, isoniazid, rifampin, pyrazinamide, and ethambutol) from 2001 to 2004 for the treatment of active TB. The data collected included age, sex, weight, country of origin, comorbid conditions, other antituberculous medications, dosage, duration of treatment, hospitalizations, previous intolerances to antituberculous medications, adverse events, and reasons for discontinuation of therapy.
Outcome Definitions
In the assessment of the study outcomes, in order to be recorded as an adverse event in the TB control database, both the attending physician and the nurse practitioner at the Tuberculosis Treatment Clinics had to concur (at the time of patient assessment) that the medication was responsible for the observed reaction. These adverse events were additionally evaluated by the investigative team for severity and the likelihood of association with the study medications according to previously published criteria described below. (17,18)
The nature of the adverse events were categorized as those related to the central nervous system, respiratory, cardiovascular (CVS), gastrointestinal, skin, and musculoskeletal (MSK). Central nervous system events included seizures, fever, vertigo/tinnitus, paresthesia, visual disturbances, headache, and confusion. CVS events included arrhythmias, hypotension, increased heart rate, and chest pain. GI system events included nausea and vomiting, anorexia/weight loss, dyspepsia, abdominal pain and hepatitis. Hepatitis was defined as liver transaminases more than three times the upper limit of normal in the presence of GI symptoms or transaminases more than five times the upper limit of normal without symptoms. Dermatologic system events were characterized as rash, pruritis, and swelling. MSK complaints included fatigue, weakness, joint pain, and tendonitis.
The severity of the adverse reaction was categorized as mild, moderate, or severe. Severity was considered as follows: (1) mild if the signs and symptoms did not require additional medication and the study drugs were continued; (2) moderate if the signs and symptoms did not require additional medication but were controlled on discontinuation of the study medication; or (3) severe if the signs and symptoms were potentially life-threatening, permanently disabling, resulted in extended hospital stay and/or required significant treatment (eg, systemic drugs), and required discontinuation of the study medication.
The likelihood of association of the adverse event to the study medication was assessed as definite, probable, possible, or unlikely by using the following five criteria: (1) known adverse drug reaction; (2) temporal relationship; (3) adverse drug reaction disappeared with dose reduction or discontinuation of study drug; (4) symptoms could not be explained by any other known condition or predisposition of patient; and (5) symptoms reappeared on rechallenge, or laboratory tests showed higher-than-normal drug levels or metabolic disturbances, which explained the symptoms. An adverse drug reaction was characterized as definite if all five of the criteria were satisfied; probable if the first four criteria were satisfied; possible if the first three criteria were satisfied; or unlikely if the relevant information could not be obtained, if the temporal sequence was atypical, or if other conditions or dispositions were considered far more likely to have caused the symptoms.
For purposes of this analysis, we included only those patients who were considered to have had a major adverse event. This was defined as patients who had a severe or moderate adverse event that was categorized to be definitely, probably, or possibly related to the TB medications according to the criteria.
Statistical Analysis
The quality of the matching of the age variable was assessed using t test. Cross-tabulations and [chi square] tests of homogeneity were computed for gender. Other descriptive analyses were calculated using t tests and [chi square] tests as appropriate. All p values < 0.05 were considered to be significant, whereas p values < 0.1 were considered as a trend to significance.
The primary analysis was to determine the overall rate of any major event occurrence in the two study arms using a Poisson regression model with the logarithm (the time taking the study drug) as an offset variable. (19) As such, a rate-ratio, with 95% confidence intervals (CIs), between the levofloxacin group and the control group was generated. The potential confounders were evaluated for each person-day of the follow-up, including ethnicity, baseline liver function, previous medication intolerance, and concurrent medications. An adjusted rate ratio was generated by a two-sided elimination method. Second, these Poisson regression analyses were repeated for each of the individual symptom systems (eg, CNS, GI, and skin).
Since a report regarding adverse events of first-line TB agents found that most of the events occurred in the first 3 months, we conducted another analysis looking at the rate of a major adverse event in the first 100 days. (17,20) Other secondary analyses (21,22) included time-to-event curves for each group that were calculated by the Kaplan-Meier method and compared by means of the log-rank test. Cox proportional hazards models were used to compare the time to the first event for the occurrence of any major event and the individual symptom systems. (23) Hazard ratios and their 95% CIs were computed for these models.
RESULTS
From June 2001 to August 2004, a total of 102 patients received levofloxacin for the treatment of active TB in combination with other standard anti-TB medications. Three hundred fifty-eight control subjects were matched to the above cases. As shown in Table 1, the mean age of the patient was 53 years (range, 11 to 98 years). Fifty-nine percent of the participants were women, 57% reported their race as South-East Asian, and 64% were being treated for pulmonary TB. The results of HIV testing were in the records of 213 patients (46%), of whom 5% were positive. Similarly, the results of hepatitis testing were in the records of only 36 patients (8%), of whom 3% were positive for hepatitis B, 3% for hepatitis C, and 1% for both hepatitis B and C. There were no significant differences in the observed demographic or clinical characteristics according to the treatment group. However, there were differences between the treatment groups with respect to the indication for use and concurrent drugs. The majority of patients in the levofloxacin arm were intolerant to one of the first-line TB medications, whereas the other 18% received levofloxacin because of drug-resistant TB. The majority of patients in the levofloxacin arm were not receiving concurrent administration of isoniazid or rifampin. In addition, patients in the levofloxacin-based strategy received significantly less pyrazinamide and ethambutol. The treatment cure rates were 100% for both treatment groups, and there were no TB-related deaths.
The incidence of major adverse events was similar in both arms, with 29% of those in the levofloxacin group having at least one event compared with 28% in the control group. The number of adverse events in the levofloxacin and control arms were similar, with 16.5% of patients experiencing one major event (18% levofloxacin group vs 15% control group), 6.5% with two major events (5% levofloxacin group vs 8% control group), and 6% with three or more major events in the study (7% levofloxacin group vs 5% control group). The organ systems involved in the major adverse events were GI (17% levofloxacin group vs 15% control group), CNS (12% levofloxacin group vs 9% control group), skin (5% levofloxacin group vs 8% control group), and MSK (7% levofloxacin group vs 6% control group). The common adverse events were nausea and vomiting (n = 10 levofloxacin group vs n = 38 control group), hepatotoxicity (n = 9 levofloxacin group vs n = 24 control group), rash (n = 3 levofloxacin group vs n = 21 control group), pruritus (n = 3 levofloxacin group vs n = 15 control group), and joint pain (n = 6 levofloxacin group vs n = 12 control group). There were no respiratory, CVS, or hematologic adverse events seen for the levofloxacin or control groups.
The rate of any major adverse event in the age-matched and gender-matched sample was almost half among those using levofloxacin as among those on standard therapies (rate ratio, 0.60; 95% CI, 0.44 to 0.82) [Table 2]. However, after an additional adjustment for the differences in exposure of concomitant medications (ethambutol, pyrazinamide, rifampin, and isoniazid), the rate ratio was no longer significantly different (Table 2). Similarly, for adverse events of the skin, the age-matched and gender-matched rate ratio showed that levofloxacin had a significantly lower event rate (rate ratio, 0.43; 95% CI, 0.20 to 0.92) when compared with the standard therapies. But after additional adjustment for exposure of concomitant medications, the rate ratio was no long significantly different (Table 2). Finally for the other organ systems (CNS, GI, and MSK), although all of the point estimates of the rate ratio were < 1 (signifying that levofloxacin had a lower event rate), none of these were significant in either the unadjusted (ie, age-matched and gender-matched only) or adjusted (ie, age, gender, and concomitant drugs) models.
In the secondary analysis, when we only evaluated events within the first 100 days, the rate ratios changed slightly. The rate of any major adverse event for the first 100 days for levofloxacin was no longer statistically significant but continued to be lower for the levofloxacin group compared with the control subjects (rate ratio, 0.73; 95% CI, 0.53 to 1.02). Additional adjustment for the differences in exposure of concomitant medications gave a similar rate ratio to the primary analysis (rate ratio, 0.86; 95% CI, 0.68 to 1.08). The rate ratios for adverse events for the first 100 days were < 1 for CNS (rate ratio, 0.64; 95% CI, 0.30 to 1.38), GI (rate ratio, 0.73; 95% CI, 0.53 to 1.02), skin (rate ratio, 0.57; 95% CI, 0.27 to 1.22), and MSK (rate ratio, 0.79; 95% CI, 0.32 to 1.97).
The time to the first major adverse event was similar between the levofloxacin group and the control group (adjusted hazards ratio, 1.01; 95% CI, 0.76 to 1.34). Similarly, the results of the other Cox regression models showed that the time to a major adverse event by an organ system was similar between the two groups (Table 3). The time to any major event for the first 100 days, for the overall case (adjusted hazards ratio, 0.99; 95% CI, 0.74 to 1.33), as well as by an organ system, was no different between the levofloxacin group and the control arm. This finding is illustrated in a Kaplan-Meier survival curve (Fig 1).
[FIGURE 1 OMITTED]
DISCUSSION
In this population-based study, we evaluated the incidence of major adverse events in anti-TB regimens containing levofloxacin and compared it with matched control subjects receiving standard anti-TB regimens. There was a significantly lower adverse event rate in the levofloxacin-containing TB treatment regimens compared with the standard regimens. This is interesting, because the majority of patients receiving levofloxacin had a history of at least one adverse reaction to first-line anti-TB drugs. In the adjusted analysis (where exposure to other TB medications were controlled), levofloxacin appeared to still have a consistently lower rate of events (rate ratio < 1), although not significantly, for any major adverse event (either overall or by individual organ system).
There is a suggestion in the literature that most adverse events for anti-TB agents occur in the first 100 days, and, therefore, using person-days of treatment for the analysis may underestimate the toxicity. Therefore, we conducted a secondary analysis for the rate of any major adverse event in the levofloxacin and control arms in the first 100 days of therapy. Ninety-five percent of the events occurred in the first 100 days; however, the rate of events (either overall or by individual organ system) did not differ compared with the primary analysis using person-days. Although the overall event rate ratio was no longer statistically significant (it crossed the point of unity with the upper confidence limit being 1.02), the point estimate was still < 1 (rate ratio, 0.70), indicating a possible lower adverse event rate in the levofloxacin group compared with the control subjects.
For the primary analysis, the relevant question being addressed is whether regimens containing levofloxacin have less toxicity than those that do not. Because the influence of the major confounding factors were either controlled by the design (age and sex) or were equally distributed between the two groups, it is unlikely that this lower rate ratio was influenced by other factors. Intuitively, this observation makes sense, because those who were treated with levofloxacin appeared to have been treated with fewer medications and, thus, could be expected to have fewer adverse events. However, even when this differential exposure to anti-TB medication was controlled for in the analysis, the point estimate for the adjusted rate ratio for levofloxacin was still < 1 with 95% confidence intervals that barely crossed the point of unity (rate ratio, 0.83; 95% CI, 0.68 to 1.08). As such, the results of this study, although not definitive in suggesting that fluoroquinolone-containing treatment regimens may result in fewer major adverse events in the treatment of active TB, do definitively show that the rate of adverse events is certainly not higher then other anti-TB medications and may, in fact, be lower.
Another possible limitation of the study may have been that the group receiving levofloxacin had a lower rate of adverse events because they were no longer exposed to the agents that were problematic in the first exposure, but, when we examined this in the multivariate model, we did not find an association, and this parameter was not retained in our final Poisson regression models.
Fluoroquinolones are currently being recommended as second-line agents for the treatment of multidrug-resistant TB and for those patients with intolerance to first-line agents by the World Health Organization. (6) In addition, consensus guidelines from the American Thoracic Society, US Center for Disease Control and Prevention, and Infectious Diseases Society of America have suggested incorporating fluoroquinolones for prophylaxis of those exposed to multidrug-resistant TB. (5) These two recommendations have been based on prospective clinical data, which have used ofloxacin, (24-27) ciprofloxaein, (28-31) and levofloxacin (27,32,33) in combination with other anti-TB agents for the treatment of drug-resistant or drug-sensitive TB. Despite the use of fluoroquinolones for a prolonged period in routine clinical practice, there remains little literature on their tolerance outside of a clinical-trial setting. (34,35) Limited tolerance to fluoroquinolones has been described when used for preventative therapy in combination with pyrazinamide, but these are individual case reports or case series. (36-40) We recognize the importance of a case series in identifying adverse events; however, the lack of a control group makes it difficult to definitively identify fluoroquinolones as the cause for the excess adverse events. Our study represents the first population-based, case-control study with a large sample size to objectively assess the adverse events associated with the use of fluoroquinolones for treatment of active TB in routine clinical practice.
The limited tolerance to the combination of ofloxacin and pyrazinamide was first described in 1994 when 14 of 16 health-care workers (87.5%) receiving prophylactic therapy (ie, treatment of latent TB) discontinued treatment in < 6 months because of adverse events. (36,37) A high incidence of adverse effects with ofloxacin and pyrazinamide was reported again 1997, (38) when 13 of 22 patients (59%) prematurely discontinued prophylactic therapy with these agents. The adverse effects included GI reactions, arthralgias, and increases in liver function tests, with one patient experiencing peak aspartate aminotransferase levels of 1,835 U/L and alanine aminotransferase levels of 2,990 U/L. Since then, two reports describing the intolerance of levofloxacin (the L-isomer of ofloxacin) and pyrazinamide have been published. (38,39) Papastavros et al (39) conducted a case series of 17 individuals with suspected multidrug-resistant, latent TB infection who were treated with pyrazinamide and levofloxacin. They found that the regimen of pyrazinamide and levofloxacin was poorly tolerated, with 14 of 17 individuals (82%) experiencing at least one adverse event involving the MSK, GI, dermatologic, or central nervous systems. Lou et al (40) evaluated the tolerability of levofloxacin and pyrazinamide in solid organ transplant patients given a prophylactic treatment. The investigators of this study also found that the regimen of pyrazinamide and levofloxacin was poorly tolerated, with 27 of 48 transplant recipients (56%) discontinuing their treatment within the first 4 months because of adverse events.
Nonrandomized studies such as ours are susceptible to bias because of confounding by indication. (41) The patients in the levofloxacin group were already intolerant to anti-TB medications (this was not adjusted for in our analysis, because a prior adverse event was one of the criteria to be placed on levofloxacin) and, thus, may have been predisposed to the development of adverse events. However, as shown by the consistently protective effect (rate ratio, < 1) of levofloxacin, if this bias exists, it would be conservative and would favor the levofloxacin group. Another limitation of the study is the small sample size, which provided limited power to detect significant associations between the cases and the control subjects. Third, the occurrence of major side effects with anti-TB drugs is associated with age, gender, ethnicity (birthplace in Asia), and HIV. (17,18) Although our analysis was matched for age and gender in the design, and there was a very similar distribution in ethnicity between groups, we were unable to adjust for HIV status, because it was not available for all of the patients. However, this was unlikely to be a source of major confounding in our population because of the relatively low prevalence of HIV infection among TB patients in British Columbia. (42) The results of our study may not be generalizable to other populations, because Asians and Aboriginals represented > 75% of the sample. Possible bias may have included a clinician's tendency to change the therapy for relatively minor adverse events more commonly when the patient was on their first-line regimen (control subjects) compared with the second regimen (cases).
The treatment of multidrug-resistant TB involves the use of multiple second-line and toxic agents for a prolonged period of time. Compliance is stressed when counseling patients on their medication, and patients must be able to tolerate their therapeutic regimens in order to achieve a cure. In this setting, the use of an anti-TB agent with fewer side effects is desirable.
CONCLUSIONS
The concomitant use of a levofloxacin-containing regimen resulted in a similar rate of adverse events compared with the control arm when it was used for the treatment of active TB, although individuals receiving this regimen have a history of adverse events. Additional studies are required to evaluate a potential protective effect of levofloxacin and newer quinolones, such as moxifloxacin, against major adverse reactions.
ACKNOWLEDGMENT: We thank Victoria Cox and Marisa Wan for collecting the data during their student rotations. We thank the contributions of Rick White, a statistician, and Dr. Ramak Shadmani, a physician epidemiologist, for their help on study design and preliminary data analysis.
REFERENCES
(1) Dye C, Scheele S, Dolin P, et al. Global burden of tuberculosis: estimated incidence, prevalence, and mortality by country. JAMA 1999; 282:677-686
(2) World Health Organization. WHO report 2003: global tuberculosis control. Report WHO/CDS/TB/2003-316. Available at: http://www.who.int/gtb/publications/globrep/index.html. Accessed July 19, 2005
(3) CDC. Reported tuberculosis in the United States, 2002. Atlanta, GA: US Department of Health and Human Services CDC, 2003
(4) Advisory Council on the Elimination of Tuberculosis (ACET). Tuberculosis elimination revisited: obstacles, opportunities, and a renewed commitment. MMWR Morb Mortal Wkly Rep 1999; 48:1-13
(5) American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America. Treatment of tuberculosis. Am J Respir Grit Care Med 2003; 167:603-662
(6) Crofton J, Choculet P, Maher D. WHO Report 1997: guidelines for the management of drug-resistant tuberculosis. Geneva, Switzerland: World Health Organization; WHO/TB/ 1996-210
(7) Gleissberg V. The threat of multidrug resistance: is tuberculosis ever untreatable or uncontrollable? Lancet 1999; 353: 998-999
(8) Snider DE, Castro KG. The global threat of drug-resistant tuberculosis. N Engl J Med 1998; 338:1689-1690
(9) Garcia-Rodriguez JA, Gomez Garcia AC. In-vitro activities of quinolones against mycobacteria. J Antimicrob Chemother 1993; 32:797-808
(10) Jacobs MR. Activity of quinolones against mycobacteria. Drugs 1999; 58(suppl):19-22
(11) Mor N, Vanderkolk J, Heifets L. Inhibitory and bactericidal activities of levofloxacin against Mycobacterium tuberculosis in vitro and in human macrophages. Antimicrob Agents Chemother 1994; 38:1161-1164
(12) Klemens SP, Sharpe CA, Rogge MC, et al. Activity of levofloxacin in a murine model of tuberculosis. Antimicrob Agents Chemother 1994; 38:1476-1479
(13) Tortoli E, Dionisio D, Fabbri C. Evaluation of moxifloxacin activity in vitro against Mycobacterium tuberculosis, including resistant and multidrug-resistant strains. J Chemother 2004; 16:334-336
(14) Nuermberger EL, Yoshimatsu T, Tyagi S, et al. Moxifloxacin-containing regimens of reduced duration produce a stable cure in murine tuberculosis. Am J Respir Grit Care Med 2004; 169:421-426
(15) Peloquin CA, Berning SE, Huitt GA, et al. Levofloxacin for drug-resistant Mycobacterium tuberculosis. Ann Pharmacother 1998; 32:268-269
(16) Pletz MW, De Roux A, Roth A, et al. Early bactericidal activity of moxifloxacin in treatment of pulmonary tuberculosis: a prospective, randomized study. Antimicrob Agents Chemother 2004; 48:780-782
(17) Yee D, Valiquette C, Pelletier M, et al. Incidence of serious side effects from first-line antituberculosis drugs among patients treated for active tuberculosis. Am J Respir Grit Care Med 2003; 167:1472-1477
(18) Schberg T, Rebhan K, Lode H. Risk factors for side effects of isoniazid, rifampin and pyrazinamide in patients hospitalized for pulmonary tuberculosis. Eur Respir J 1996; 9:2026-2030
(19) Myers RH, Montgomery DC, Vinig GG. Generalized linear model: with applications in engineering and the sciences. New York, NY: John Wiley & Sons, 2002
(20) Chaisson RE. Tuberculosis chemotherapy: still a double-edged sword. Am J Respir Grit Care Med 2003; 167:1461-1462
(21) Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Star Assoc 1958; 53:457-481
(22) Mantel N. Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chemother Rep 1966; 50:163-170
(23) Cox DR. Regression models and life tables. J R Stat Soc Ser B 1972; 34:187-220
(24) Hong Kong Chest Service/BMJ Research Council. A controlled study of rifabutin and an uncontrolled study of ofloxacin in the retreatment of patients with pulmonary tuberculosis resistant to isoniazid, streptomycin and rifampicin. Tuber Lung Dis 1992; 73:59-67
(25) Kohno S, Koga H, Kaku M, et al. Prospective comparative study of ofloxacin or ethambutol for the treatment of pulmonary tuberculosis. Chest 1992; 102:1815-1818
(26) Sirgel FA, Donald PR, Odhiambo J, et al. A multicentre study of the early bactericidal activity of anti-tuberculosis drugs. J Antimicrob Chemother 2000; 45:859-870
(27) Yew WW, Chan CK, Leung CC, et al. Comparative roles of levofloxacin and ofloxacin in the treatment of multidrug-resistant tuberculosis: preliminary results of a retrospective study from Hong Kong. Chest 2003; 124:1476-1481
(28) Mohanty KC, Dhamgaye TM. Controlled trial of ciprofloxatin in short-term chemotherapy for pulmonary tuberculosis. Chest 1993; 104:1194-1198
(29) Kennedy N, Fox R, Kisyombe GM, et al. Early bactericidal and sterilizing activities of ciprofloxacin in pulmonary tuberculosis. Am Rev Respir Dis 1993; 148:1547-1551
(30) Yew WW, Chau CH, Wong PC, et al. Ciprofloxacin in the management of pulmonary tuberculosis in the face of hepatic dysfunction. Drugs Exp Clin Res 1995; 21:79-83
(31) Sirgel FA, Botha FJ, Parkin DP, et al. The early bactericidal activity of ciprofloxacin in patients with pulmonary tuberculosis. Am J Respir Grit Care Med 1997; 156:901-905
(32) El-Sadr WM, Perlman DC, Marts JP, et al. Evaluation of an intensive intermittent-induction regimen and duration of short-course treatment for human immunodeficiency virus-related pulmonary tuberculosis: Terry Beirn Community Programs for Clinical Research on AIDS (CPCRA) and the AIDS Clinical Trials Group (ACTG). Clin Infect Dis 1998; 26:1148-1158
(33) Telzak EE, Chirgwin KD, Nelson ET, et al. Predictors for multidrug-resistant tuberculosis among HIV-infected patients and response to specific drug regimens: Terry Beirn Community Programs for Clinical Research on AIDS (CPCRA) and the AIDS Clinical Trials Group (ACTG), National Institutes for Health. Int J Tubere Lung Dis 1999; 3:337-343
(34) Berning SE. The role of fluoroquinolones in tuberculosis today. Drugs 2001; 61:9-18
(35) Ginsburg AS, Grosset JH, Bishai WR. Fluoroquinolones, tuberculosis and resistance. Lancet Infect Dis 2003; 3:432-442
(36) Horn DL, Hewlett D, Alfalla C, et al. Limited tolerance of ofloxacin and pyrazinamide prophylaxis against tuberculosis [letter]. N Engl J Med 1994; 330:1241
(37) Horn DL, Hewlett D, Alfalla C, et al. Limited tolerance of ofloxacin and pyrazinamide prophylaxis in health-care workers following exposure to rifampin-isoniazid-streptomycin-ethambutol-resistant tuberculosis. Infect Dis Clin Pratt 1995; 4:219-225
(38) Ridzon R, Meador J, Maxwell R, et al. Asymptomatic hepatitis in persons who received alternative preventive therapy with pyrazinamide and ofloxacin. Clin Infect Dis 1997; 24:1264-1265
(39) Papastavros T, Dolovich LR, Holbrook A, et al. Adverse events associated with pyrazinamide and levofloxacin in the treatment of multidrug-resistant tuberculosis. Can Med Assoc J 2002; 167:131-136
(40) Lou H-X, Shallo MA, McKaveney TP. Limited tolerability of levofloxacin and pyrazinamide for multidrug resistant tuberculosis prophylaxis in solid organ transplant population. Pharmacotherapy 2002; 22:701-704
(41) McMahon AD. Approaches to combat with confounding by indication in observational studies of intended drug effects. Pharmacoepidemiol Drug Saf 2003; 12:551-558
(42) Hernandez-Garduno E, Cook V, Kunimoto D, et al. Transmission of tuberculosis from smear negative patients: a molecular epidemiology study. Thorax 2004; 59:286-290
* From the University of British Columbia (Drs. F. Marra, C.A. Marra, Shi, Elwood, and FitzGerald), Vancouver BC, Canada; and BC Centre for Disease Control (Ms. Moadebi and Mr. Stark) Vancouver, BC, Canada.
None of the authors have direct financial interest in the subject matter of the manuscript. In particular, none of the authors have received funding from Jansen-Ortho, the manufacturer of Levofloxacin.
Manuscript received November 29, 2004; revision accepted February 4, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Fawziah Marra, PharmD, BC Centre for Disease Control, Vaccine and Pharmacy Services, 655 West 12th Ave, Vancouver, BC, V5Z 4R4 Canada; e-mail: fawziah.marra@ bccdc.ca
isoniazid.
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group