Background: Although fluoroquinolones possess excellent in vitro activity against Legionella, few large-scale clinical trials have examined their efficacy in the treatment of Legionnaires disease. Even fewer studies have applied rigorous criteria for diagnosis of community-acquired Legionnaires disease, including culture of respiratory secretions on selective media.
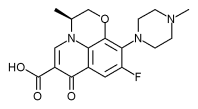
Methods: Data from six clinical trials encompassing 1,997 total patients have been analyzed to determine the efficacy of levofloxacin (500 mg qd or 750 mg qd) in treating patients with community-acquired pneumonia (CAP) due to Legionella.
Results: Of the 1,997 total patients with CAP from the clinical trials, 75 patients had infection with a Legionnella species. Demographics showed a large portion of these patients were < 55 years of age and nonsmokers. More than 90% of mild-to-moderate and severe cases of Legionella infection resolved clinically at the posttherapy visit, 2 to 14 days after treatment termination. No deaths were reported for any patient with Legionnaires disease treated with levofloxacin during the studies.
Conclusions: Levofloxacin was efficacious at both 500 mg for 7 to 14 days and 750 mg for 5 days. Legionnaires disease is not associated only with smokers, the elderly, and the immunosuppressed, but also has the potential to affect a broader demographic range of the general population than previously thought. (CHEST 2004; 125:2135-2139)
Key words: clinical efficacy; community-acquired pneumonia; Legionella; levofloxacin
Abbreviations: BCYE = buffered charcoal yeast extract: CAP = community-acquired pneumonia; ELISA = enzyme-linked immunosorbent assay: MIC = minimum inhibitory concentration; PSI = pneumonia severity index
**********
Legionella are facultative, intracellular bacteria that penetrate and proliferate within the phagosomes of alveolar macrophages and blood monocytes. (1-3) Thus, antimicrobials that cannot penetrate the host's cellular membrane, such as penicillins and cephalosporins, are relatively ineffective against these bacteria. (4) Legionella is a major cause of lethal pneumonia, and mortality rates range from 5 to 25% among immunocompetent hosts, and even higher among the immunosuppressed. (5)
In the past, erythromycin was typically used for the treatment of Legionnaires disease. However, newer antimicrobials have been shown to be safer and more effective. (6) The Infectious Diseases Society of America and the American Thoracic Society' currently recommend doxycycline, azithromycin, and various fluoroquinolones for treating Legionella respiratory infections. (7,8)
Levofloxacin, one of the recommended fluoroquinolones, has excellent in vitro activity against Legionella, with a minimum inhibitory concentration (MIC) equal to 0.03 [micro]g/mL. (9) In vitro studies (3,10,11) using intracellular systems have shown that levofloxacin is effective in intracellular killing of various Legionella strains. In addition, levofloxacin concentrates in the intrapulmonary compartments at levels well above the MIC. (12) Steady-state concentrations of levofloxacin in the epithelial lining fluid and 'alveolar macrophages are significantly higher than the plasma concentrations. (12) The ratio of the area under the concentration-time curve or peak concentration to MIC is assumed to be a key pharmacodynamic indication for clinical and microbiologic success of the fluoroquinolones. (13,14) In addition, unlike the macrolides, which are bacteriostatic for Legionella, the quinolones are bactericidal. (15)
Legionnaires disease cannot be readily diagnosed because of its nonspecific clinical and radiologic manifestations, and the need for specialized laboratory tests. (16) Culture and urinary antigen are considered the most specific tests for diagnosis. In the prospective analysis of levofloxacin presented herein, efficacy and toxicity data are presented for what we believe to be the largest population of eases of sporadic community-acquired Legionnaires disease ever studied.
MATERIALS AND METHODS
Clinical Trials Involved
This analysis integrated data from five prospective phase 111 clinical trials (studies 1, 2, 3, 5, and 6) and one phase IV clinical trial (study 4). Study 1 (data on file; R.W. Johnson Pharmaceutical Research Institute; Raritan, NJ) and study 317 were open-label, noncomparative studies that evaluated the efficacy and safety profiles of levofloxacin in the treatment of CAP. Study 2 (18) was an open-label, randomized, active-controlled study that compared levofloxacin with parenteral ceftriaxone and/or oral cefuroxime axetil in the treatment of CAP. Study 4 (19) was an open-label, randomized, active controlled study that compared levofloxacin with ceftriaxone plus erythromycin, followed by amoxicillin-clavulanate plus clarithromycin. Additionally, patients in study 4 had diagnoses of "serious" CAP; they fulfilled criteria that predicted a higher probability" of death, roughly comparable to the pneumonia severity index (PSI) class IV population (score of 91 to 130). (20) Study 5 was a multicenter, randomized, double-blind study that compared the efficacy of 5 day, high-dose (750 mg) levofloxacin therapy with a 10-day course of levofloxacin 500 mg for CAP. (21) Study 6 was a noncomparative, open-label study that evaluated tire efficacy of the 5-day, high-dose levofloxacin regimen for CAP (data on file; Ortho-McNeil Pharmaceutical, Inc.; Raritan, NJ).
Subjects
The investigational review board of each center approved the studies, and all patients provided written informed consent. All enrolled patients required a primary diagnosis of CAP confirmed by radiographic evidence. For studies 1, 2, and 3, the clinical signs and symptoms of CAP also included at least two of the following: elevated temperature (oral [greater than or equal to] 38[degrees]C, rectal [greater than or equal to] 39[degrees]C), new or increased cough, production of purulent sputum, rales or pleuritic chest pain, and shortness of breath. Studies 5 and 6 required at least one of the following: fever (oral [greater than or equal to] 38[degrees]C) or hypothermia (oral [less than or equal to] 35[degrees]C), leukocytosis (WBC count > 10,000/ [micro]L), or bands > 10%. Excluded from these studies were patients with the following: (1) infections due to organisms known to be resistant to a study (hug prior to the patient's entry into the study, (2) a diagnosis of cystic fibrosis or fungal infection, (3) empyema, (4) HIV infection and CD4 counts < 200 cells/[micro]L, (5) neutropenia (< 500 cells/[micro]L), (6) hospital-acquired infections, (7) requirement of an additional nonstudy systemic antimicrobial agent, (8) a history of seizures or a major psychiatric disorder, (9) a history of allergy to a study drug or drugs, (10) pregnancy or breast feeding, (11) severe renal impairment (creatinine clearance < 20 mL/min [creatinine clearance < 50 mL/min for study 5]), or (12) any investigational agent within 30 days of entry into the study.
Patients in studies 1, 2, and 3 were classified as having severe, pneumonia on the basis of one or more of the following: bacteremia, hypotension (diastolic BP < 60 mm Hg) in the absence of volume depletion, altered mental status, baseline respiratory rate exceeding 30 breaths/min, or a requirement for intubation or mechanical ventilation. Patients in study 4 were considered to have a high risk of mortality and had to have at least three American Thoracic Society criteria for hospital admission, (8) and either mechanical ventilation or two of the following: elevated temperature (oral [greater than or equal to] 39[degrees]C) or hypothermia (oral [less than or equal to] 35[degrees]C), respiratory rate > 30 breaths/min, systolic hypotension (systolic BP < 90 mm Hg), pulse rate of at least 131) beats/min, or altered mental status. The inclusion criteria of study 4 limited enrollment to those patients with severe CAP. In studies 5 and 6, the patient's PSI score (20) determined the severity of the disease. Mild-to-moderate cases belonged to PSI class I or II (score, [less than or equal to] 70) and were treated as inpatients or outpatients, while severe cases belonged to PSI class III or IV (PSI score > 70 but [less than or equal to] 130) and were hospitalized for at least 24 h.
Study Design
Patients in studies 1, 2, and 3 received levofloxacin, 500 mg/d for 7 to 14 days, while patients in study 4 received levofloxacin, 500 mg/d for 10 to 14 days. (Two patients in study 2 with Legionnaires disease underwent extended therapies of 15 days and 18 days, respectively.) In study 5, patients received levofloxatin, 500 mg/d, for 10 days or 750 mg for 5 days. Patients in study 6 received levofloxacin, 750 mg for 5 days. Patients in all trials were started un either IV or oral therapy, and those receiving IV therapy could be switched to oral medication at the investigator's discretion. Clinical ,and microbiologic responses were determined at a posttherapy visit occurring 2 to 14 days after cessation of drug therapy, and at a poststudy visit occurring 3 to 5 weeks after the completion of drug therapy. At posttherapy, a cured or improved patient had resolution or partial resolution of clinical signs and symptoms associated with active infection, along with improvement or stabilization on chest radiograph. Failure indicated an inadequate response to therapy with additional antibiotic treatment required for the original infection. Failure was also designated for patients who had a clinical failure but in whom the admission pathogen appeared to have been eradicated (negative test-of-cure culture finding).
Legionella Diagnostic Testing
The Special Pathogens Laboratory at the VA Pittsburgh Healthcare System, Pittsburgh, PA, performed Legionella culture, urinary antigen, and serologic testing. Cases were diagnosed as Legionnaires disease based on any of the following: (1) fourfold increase in the level of IgM or IgG determined by enzyme-linked immunosorbent assay, (ELISA), (2) seroconversion by the Carter Wallace IgG/IgM ELISA (Carter-Wallace-Wampole; Cranbury, NJ), (3) positive urinary antigen test result using EIA for Legionnela pneuzmophila serogroup 1 (Binax; S. Portland, ME), or (3) isolation of Legionella from pretreatment sputum cultures. Culture was performed using three media: buffered charcoal yeast extract (BCYE) agar; BCYE with polymixin B, anisomycin, and vancomycin (PAV); and BCYE with polymixin B, anisomycin, and cefamandole (PAC). Specimens were pretreated with an acid buffer (HCl-KCl, pH 2.2) for 4 min prior to plating.
Statistical Evaluation Groups
The intent to-treat population consisted of all patients in file trials who were treated with levofloxacin and who fulfilled the previously mentioned criteria for CAP caused by a Legionella species. The clinically evaluable population was a combination of all Legionella-infected patients in the clinically evaluable populations of the six individual clinical trials.
RESULTS
Patient Demographic and Baseline Characteristics
>From a total of 1,997 patients with a diagnosis of CAP, 75 patients (3.8%) had Legionella infection based on at least one of the following criteria: seroconversion (either fourfold increase in IgM or IgG levels determined by ELISA [55 patients] or by Wampole EIA [14 patients]), positive urinary antigen (5 patients), or positive sputum culture (6 patients). The numbers total > 75 because some patients had multiple positive test results. In the clinically evaluable population, 71 of 1,551 patients (4.6%) were determined to have Legionella infection. Patients were stratified according to the severity of the disease, with 47 patients classified with mild-to-moderate CAP and 24 patients with severe CAP. Patients were categorized according to whether they had traditional risk factors for contracting Legionella-induced CAP. Forty-six percent (33 of 71 patients) of the clinically evaluable population had a chronic respiratory disease, including bronchitis, emphysema, sinusitis, and COPD, and 41% (29 of 7] patients) had a history of smoking. Thirty-four percent (24 of 71 patients) had none of these risk factors, and over half of these (14 of 24 patients) were also < 55 years of age.
Seroconversion to Mycoplasma pneumoniae and Chlamydia pneumoniae was observed in 25% (19 of 75 patients) and 17% (13 of 75 patients), respectively. Fifteen percent (11 of 75 patients) and 9% (7 of 75 patients) had Streptococcus pneumoniae and Haemophilus influenzae isolated from sputum cultures, respectively.
Clinical Evaluations
Seventy-one patients with community-acquired Legionnaires disease were clinically evaluable, and clinical success (cured plus improved) was observed during the posttherapy visit (Table 1) in 92.9% (66 of 71 patients) overall; 74.6% were cured and 18.3% were improved. Clinical failure occurred in five patients (7.0%) based on the criteria that additional antibiotics were prescribed by the physician None of the five clinical failures resulted in patient death. Among the 13 patients receiving 750 mg of levofloxacin for 5 days, 12 patients (92.3%) achieved clinical success at posttherapy; 5 of the patients had severe pneumonia.
During the posttherapy visit, 93.6% of mild-to-moderate cases were assessed as clinical successes, compared with 91.6% of the severe cases. Also, no patient was found to have a documented microbiological relapse during the poststudy visit (3 to 5 weeks after therapy ended).
Safety Evaluations
Adverse effects in 7% (5 of 75 patients) were judged by the investigator to be probably or definitely drug related. The most common complaints included anxiety, insomnia, headache, nausea, and diarrhea. Most of the reported adverse events were judged to be mild in character by the investigators, and no patients discontinued therapy because of drug-related adverse events.
DISCUSSION
Levofloxacin was found to be highly effective against Legionella infectious, leading to clinical success in > 90% of patients. It should be noted that, while not all patients with Legionnaires disease in these six studies fulfilled the criteria for cure, not a single patient died during the course of hospitalization and/or treatment. Levofloxacin treatment was as successful in patients with severe CAP as in those with mild-to-moderate disease. During the posttherapy visit, clinical success was seen in 93.6% of patients with mild-to-moderate pneumonia, compared with 91.6% with severe pneumonia, with no documented microbiologic relapse in either patient group.
For 13 patients with Legionella, a high-dose (750 mg), short-course (5 day) levofloxacin treatment was administered. This regimen was based on the rationale that higher concentration peaks lead to increased killing of the pathogen, decreased resistance development, and higher patient compliance with the shorter course. The 750-mg dose increases peak plasma concentration twofold over the 500-mg dose at steady state, while maintaining a high drug concentration in the alveolar macrophages (105.1 [micro]g/mL 4 h after dosing). (12) The clinical cure rate was 92.3% (12 of 13 patients) at posttherapy; 5 of the patients had severe pneumonia. Although definitive conclusions cannot be drawn from the limited number of patients in this study, a high-dose, short-course therapy warrants scrutiny as a treatment option for Legionella-induced CAP.
In a meta-analysis of 13 studies of CAP in which an oral antibiotic could be administered, the respiratory quinolones showed a modest therapeutic advantage compared with other alternative antibiotics (such as macrolides, [beta]-lactams, and doxycycline) (22); 100% (10 of 10 patients) of fluoroquinolone-treated patients with Legionella infection were cured as compared to 33% (4 of 12 patients) treated with a [beta]-lactam agent. In another retrospective observational study (15) of 33 patients with Legionnaires disease, patients treated with a fluoroquinolone had lower complications, more rapid defervescence, and lower mortality than patients treated with erythromycin; the differences, however, were not statistically significant.
Legionella infections account for up to 16% of cases of CAP, and in numerous observational studies Legionella is among the top four microbial causes of hospitalization due to CAP. (6,23) The classic risk factors for Legionnaires disease include cigarette smoking, chronic lung disease, and immunosuppression; the disease most frequently occurs in the elderly. (6) Based on a large-scale study of CAP in Ohio, the Centers for Disease Control and Prevention (CDC) estimated that only 3% of sporadic cases of Legionnaires disease are correctly diagnosed (24) It is probable that detection bias occurs such that those patients with the classic risk factors are more likely to undergo Legionella laboratory testing.
However, the demographics of the patients with Legionella in this large study deviated from the typical patient profiles, especially with > 70% of the subjects being < 65 years of age. Although approximately half of the patients had a history of respiratory illness and more than a fourth had a history of smoking, we found that approximately 34% (24 of 71 patients) did not have either of these risk factors. In addition, 14 of these 24 patients were 'also < 55 years of age, providing evidence that Legionnaires disease is not limited to elderly patients with chronic respiratory illnesses or a history of smoking. None of the patients were known to be receiving immunosuppressive therapy, which is another key risk factor for Legionnaires disease. Interestingly, in a retrospective review of Legionnaires disease in Allegheny County, PA, Squier et al (25) also found that 28% of reported eases had none of the classic risk flatters for Legionnaires disease. These findings suggest that testing for Legionnaires disease is warranted in patients with CAP with broader demographics than previously appreciated. These data also suggest the need for an agent with intracellular activity when treating CAP regardless of the presence or absence of the typical Legionella risk factors. This is the largest antibiotic study of patients with Legionella-induced CAP ever published. Levolloxacin proved to be highly efficacious at both the 500-mg and 750-mg doses, and mortality was negligible. With greater routine use of Legionella culture on selective media, it is likely that undiagnosed eases may be uncovered. Moreover, other Legionella seregroups and species not diagnosable by serology and urinary antigen may be identified as the actual etiology of CAP.
REFERENCES
(1) Roig J, Domingo C, Morera J. Legionnaires disease. Chest 1994; 105:1817-1825
(2) Nguyen MLT, Yu VL. Legionella infection. Clin Chest Med 1991; 12:257-268
(3) Baltch AL, Smith RP, Franke MA, et al. Antibacterial effects of levofloxacin, erythromycin, and rifampin in a human monocyte system against Legionella pneumophila. Antimicrob Agents Chemother 1998; 42:3153-3156
(4) Edelstein PH. Antimicrobial chemotherapy for Legionnaires disease: a review. Clin Infect Dis 1995; 21(suppl 3):S265-S276
(5) Marston BJ, Lipman HB, Breiman RF. Surveillance for Legionnaires disease: risk factors for morbidity and mortality, Arch Intern Med 1994; 154:2417-2422
(6) Stout JE, Yu VL. Legionellosis. N Engl J Med 1997; 337:682-687
(7) Bartlett JG, Dowell SF, Mandell LA, et al. Practice guidelines for the management of community-acquired pneumonia in adults. Clin Infect Dis 2000; 31:347-382
(8) Niederman MS, Mandell LA, Anzueto A, et al. Guidelines for the management of adults with community-acquired pneumonia: diagnosis, assessment of seventy, antimicrobial therapy, and prevention. Am J Respir Crit Care Med 2001; 163:1730-1754
(9) Critchley IA, Jones ME, Heinze PD, et al. In vitro activity of levofloxacin against contemporary clinical isolates of Legionella pneumophila, Mycoplasma pneumoniae and Chlamydia pneumoniae from North America and Europe. Clin Microbiol Infection 2002; 8:214-221
(10) Stout JE, Arnold B, Yu VL. Comparative activity of ciprofloxacin, ofloxacin, levofloxacin, and erythromycin against Legionella species by broth microdilution and intracellular susceptibility testing in HL 60 cells. Diagn Microbiol Infect Dis 1998; 30:37-43
(11) Smith RP, Baltch AL, Franke M, et al. Effect of levofloxacin, erythromycin or rifampicin pretreatment of growth of Legionella pneumophila in human monocytes. J Antimicrob Chemother 1997; 40:673-678
(12) Gotfried MH, Danziger LH, Rodvold KA. Steady-state plasma and intrapulmonary concentrations of levofloxacin and ciprofloxacin in healthy adult subjects. Chest 2001; 119:1114-1122
(13) Wright DH, Brown GH, Peterson ML, et al. Application of fluoroquinolone pharmacodynamics. J Antimicrob Chemother 2000; 46:669-683
(14) Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis 1998; 26:1-12
(15) Pedro-Botet M, Vilaseca Z, Sopena N, et al. Erythromycin versus fluoroquinolones in the treatment of Legionnaires disease. Presented at the 41st Interscience Conference for Antimicrobial Agents and Chemotherapy, Chicago, IL, September 22 to 25, 2001; abstract L-878
(16) Mulazimoglu L, Yu VL. Can Legionnaires disease be diagnosed by clinical criteria? A critical review. Chest 2001; 120:1049-1053
(17) Fogarty CM, Sullivan JG, Chattman MS, et al. Once a day levofloxacin in the treatment of mild to moderate and severe community-acquired pneumonia in adults. Infect Dis Clin Pract 1998; 7:400-407
(18) File TM Jr, Segreti J, Dunbar L, et al. A multicenter, randomized study comparing the efficacy and safety of intravenous and/or oral levofloxacin versus ceftriaxone and/or cefuroxime axetil in treatment of adults with community-acquired pneumonia. Antimicrob Agents Chemother 1997; 41:1965-1972
(19) Fogarty C, Siami G, Kohler R, et al. Multicenter, open-label, randomized study to compare the safety and efficacy of levofloxacin vs ceftriaxone sodium and erythromycin followed by clarithromycin and amoxicillin/clavulanate in the treatment of serious community-acquired pneumonia in adults. Clin Infect Dis 2004; 38(Suppl): S16-S23
(20) Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify, low-risk patients with community-acquired pneumonia. N Engl J Med 1997; 336:243-250
(21) Dunbar LM, Wunderink RG, Habib MP, et al. High-dose, short-course levofloxacin for community-acquired pneumonia: a new treatment paradigm. Clin Infect Dis 2003; 37:752-760
(22) Salkind AR, Cuddy PG, Foxwortb JW. Fluoroquinolone treatment of community-acquired pneumonia: a meta-analysis. Area Pharmacother 2002; 36:1938-1943
(23) Muder RR, Yu VL, Fang G-D. Community-acquired Legionnaires disease. Semin Respir Infect 1989; 4:32-39
(24) Marston BJ, Ploufte JF, Breiman RF, et al. Preliminary findings of a community/based pneumonia incidence study. In: Barberee JM, Breiman RF, Dufour AP, eds. Legionella: current status and emerging perspectives. Washington, DC: American Society for Microbiology, 1993; 36-37
(25) Squier C, Lin YE, Stout JE. "Waterborne pathogens: Legionella and other opportunistic pathogens. Presented at the American Society of Healthcare Engineers of the American Hospital Association, July 16 to 18, 2001; Tampa, FL; abstract 055995
* From the VAMC and University of Pittsburgh (Drs. Yu and Stout), Pittsburgh, PA; Department of Veterans Affairs Medical Center, University of Kentucky Medical Center (Dr. Green berg), Lexington, KY; and Ortho-McNeil Pharmaceutical, Inc. (Drs. Zadeikis, Olson, Tennenberg, and Mr. Khashab), Raritan, NJ. Drs. Yu and Stout have received research funding from Ortho-McNeil Pharmaceutical, Inc., but not for this study.
Drs. Tennenberg, Olson, Zadeikis, Kahn, and Mr. Khashab are employed by Ortho-McNeil Pharmaceutical Inc.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Manuscript received July 10, 2003; revision accepted December 30, 2003.
Correspondence to: Neringa Zadeikis, MD, MBA, Ortho-McNeil Pharmaceutical, Inc., 1000 Route 202, Room 3121, Raritan, NJ 08869-0602; e-mail: nzadeiki@ompus.jnj.com
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group