Abstract
In this double-blind, placebo-controlled, crossover, parallel study, we treated 20 adults who had seasonal allergic rhinitis with once-daily fixed-combination loratadine/pseudoephedrine sulfate to observe its effect on relieving symptoms, primarily nasal congestion. Acoustic rhinometry detected a trend toward improvement in nasal patency, although the difference between pre- and post-treatment measures was not statistically significant. Endoscopic inferior turbinate photography documented that treatment led to statistically significant reductions in the amount of nasal edema and nasal secretions. The results of a quality-of life questionnaire suggested that treatment alleviated nasal and ocular symptoms of rhinoconjunctivitis. An analysis of subjective visual analog scale scores showed a trend toward improvement in most but not all nasal symptoms. We conclude that once-a-day fixed-combination loratadine/pseudoephedrine is effective in relieving nasal congestion in patients with seasonal allergic rhinitis.
Introduction
Symptoms of seasonal allergic rhinitis include nasal congestion, rhinorrhea, nasal and throat itching, postnasal drip, and sneezing. Of these five symptoms, nasal congestion is the most frequent and often the most severe. [1,2] The physical signs associated with seasonal allergic rhinitis are erythema of the nasal mucosa, edema of the turbinates, and excessive nasal secretions.
The cornerstones of treatment are antihistamines and decongestants. The signs and symptoms of allergic rhinitis are mediated primarily by histamine. Symptoms occur as a result of the direct and indirect actions of histamine on [H.sub.1] and, to a lesser extent, [H.sub.2] receptors. [3] Antihistamines, by blocking [H.sub.1] receptors, are effective in suppressing rhinorrhea and sneezing, but they are less effective in relieving nasal congestion. The reason is that antihistamines cannot blunt the prolonged action of other vasoactive mediators (kinins and leukotrienes), nor can they reverse capillary vasodilation, which is mediated by [H.sub.2] receptors. [3] Decongestants are alpha-adrenoceptor agonists that constrict the upper respiratory mucosal vessels, thus reducing mucosal edema and lessening the subjective sensation of nasal congestion.
Loratadine is a nonsedating antihistamine that has been found to be safe and effective in relieving rhinorrhea, nasal itching, and sneezing in patients with seasonal allergic rhinitis. [4] Pseudoephedrine sulfate is an orally active decongestant that reduces nasal edema and alleviates congestion. The once-daily fixed-combination form of these two drugs (Claritin-D 24 Hour; Schering Corp.) contains 10 mg of immediate-release loratadine and 240 mg of extended-release pseudoephedrine and has been approved for the relief of symptoms of seasonal allergic rhinitis. In a study by Bronsky et al, this fixed-combination agent was shown to he safe and effective in relieving overall nasal symptoms, as well as the specific symptom of nasal congestion. [5]
The goal of this study was to further evaluate the efficacy of loratadine/pseudoephedrine in relieving nasal congestion in patients with seasonal allergic rhinitis, and to assess by several different measures of effectiveness its effect on other common parameters associated with allergic rhinitis. These measures included an objective quantitative instrument (acoustic rhinometry), an objective qualitative instrument (endoscopic inferior turbinate photography), and two patient-oriented quantitative instruments (rhinoconjunctivitis quality-of-life questionnaire scores and visual analog allergic symptom scores).
Materials and methods
Study design. We undertook this double-blind, placebo-controlled, crossover, parallel trial at the University of Chicago to study the effect of loratadine/pseudoephedrine on nasal congestion caused by natural exposure to seasonal allergens in patients who had seasonal allergic rhinitis. Before any patients were recruited, the study was approved by the Human Research Institutional Review Board at the University of Chicago Medical Center. To be eligible for this study, patients had to have been free from intranasal and parenteral steroids for 2 weeks, astemizole for at least 3 months, other antihistamines for at least 3 days, and decongestants and ipratropium for at least 1 week prior to starting the study.
Seasonal allergic rhinitis to ragweed was diagnosed by a positive skin prick test or by an allergen-specific enzyme immunoassay (Pharmacia Diagnostics; Piscataway, N.J.) result of class 2 or greater. [6] Patients had to have been free of other health problems, could not be taking alpha blockers, and they must not have had any contraindication to using pseudoephedrine. All patients were informed of the procedures, treatments, and potential risks they might encounter during the study, and all signed informed consent statements before their first visit. Patients were also instructed on how to complete the quality-of-life questionnaire and how to perform the visual analog test prior to starting the study.
During their initial visit to the allergy clinic, patients provided their medical history and underwent an otolaryngologic examination, with specific emphasis on the nasal examination. They also underwent allergy testing for specific weeds. Nasal congestion was measured objectively by two means: quantitatively by acoustic rhinometry and qualitatively by a blinded visual analysis of endoscopic color photography of the inferior turbinates. Symptoms of nasal congestion were quantified by rhinoconjunctivitis quality-of-life questionnaire scores and visual analog allergic symptom scores. The seven women in the study were tested for pregnancy, and all results were negative. These women all agreed to practice birth control for the duration of the study, and they all had a negative urine pregnancy test immediately after the completion of the study.
All patients had to agree to spend at least 1 hour outdoors each day in an area of Chicago where natural exposure to ragweed pollen was expected to occur. Depending on which group they had been randomized to, patients were instructed to take either the active drug or placebo once a day between 7 and 8 a.m.
Patients returned to the allergy clinic 7 days after their initial visit. Acoustic rhinometry and endoscopic photography were repeated, and quality-of-life and visual analog scores were again recorded. Patients were also questioned about any leftover medications. Following a washout period of at least 7 days, patients returned for a third visit, and the same procedures and tests were repeated. Patients were then crossed over to the alternate regimen for 7 days. After I week on the alternate regimen, they returned for the fourth and final visit, and the procedures and tests were again repeated; patients were also questioned again regarding any leftover medications, and the women underwent a second pregnancy test.
Treatment schedules were in part dependent on pollen counts in the Chicago area, which were recorded at the nearest American Academy of Allergy, Asthma, and Immunology testing station. When pollen counts were low, treatment for some patients was postponed and the washout period for others was extended. The aim was to have all patients on their regimen when counts were higher than 50.
Acoustic rhinometry. Acoustic rhinometry was performed with a second-generation rhinometer (Hood Laboratories; Pembroke, Mass.) according to the protocol established by Hilberg. [7] Each patient's nasal patency was evaluated by measuring the cross-sectional area (CSA) of the nose at the nasal valve (CSA1), at the anterior portion of the inferior turbinate (CSA2), and at the anterior portion of the middle turbinate (CSA3). We also measured the total nasal volume. Measurements were taken of both sides of the nose and considered together to minimize any possible influence of the nasal cycle. The greater the cross-sectional area and nasal volume, the less the nasal obstruction.
Endoscopic photography. To obtain endoscopic photographs of the inferior turbinates, we asked patients to sit in a hydraulic examining chair that was equipped with a stable head support to prevent excess head movement during the examination. The height of the chair was adjusted to bring the floor of the nasal fossa to the level of the Hopkins 4 mm 0[degrees] endoscope, which was connected to a video camera with a C-ring. The endoscope was placed at the anterior margin of the inferior turbinate, and the distance from the tip of the endoscope to the C-ring was measured. Two still photographs of each side of the nose (again, to minimize the influence of the nasal cycle) were obtained from the videotaped recording of the anterior nasal endoscopic examination. The photographs of the inferior turbinates were evaluated in ablinded fashion by two investigators for redness, edema, and secretions. Each of these parameters was rated on a scale of 0 (none) to 5 (severe). The total score at each visit was obtained by add ing the grades of both observers for both photographs for both sides of the nose. The maximum score for each of the three parameters was 40.
Quality-of-life questionnaire. Our rhinoconjunctivitis quality-of-life questionnaire was based on that designed by Juniper and Guyatt. [8] The questionnaire covers seven domains: nasal symptoms, eye symptoms, other symptoms, performance of daily activities, practical problems, quality of sleep, and emotional status. Patients rated themselves on a scale of 1 (hardly troubled) to 6 (extremely troubled).
Visual analog symptom scale. There were nine domains of nose and eye symptoms measured on the visual analog scale. The five nasal domains were stuffy nose (which was the focus of this study), runny nose, nasal or throat itching, postnasal drip, and sneezing. The four eye domains were itchy eyes, watery eyes, sore or red eyes, and swollen eyes. Patients rated the degree of their symptoms on a scale of 0 (none) to 100 (very severe).
Results
Demographics. Twenty-two patients enrolled in the study between Aug. 1 and Oct. 16, 1997. The study was closed on Nov. 4, 1997. Two patients were subsequently excluded from this analysis because they did not complete the study. The 20 remaining patients were made up of seven women and 13 men, aged 19 to 51 years (mean: 30). Three were smokers (one-half to one pack per day) and 14 were moderate alcohol drinkers. All patients tested positive for allergies to ragweed, and all were symptomatic at the time of the study.
Acoustic rhinometry. Acoustic rhinometry measurements were obtained from 18 patients (table 1). Results:
CSA1. Treatment with loratadine/pseudoephedrine resulted in a mean improvement in CSA1 measurements of 0.073 ([pm]0.089) [cm.sup.2], while placebo resulted in a mean worsening of 0.006 ([pm]0.246) [cm.sup.2].
CSA2. Likewise, active treatment increased the mean CSA2 value by 0.11 ([pm]0.424) [cm.sup.2], while placebo resulted in a mean worsening of 0.03 ([pm]0.694) [cm.sup.2].
CSA3. The mean CSA3 value improved during both active and placebo treatment-by 0.076 ([pm]0.629) and 0.017 ([pm]0.927) [cm.sup.2], respectively.
Nasal volume. The mean nasal volume increased by 0.398 ([pm]1.891) [cm.sup.3] during active treatment, and decreased during placebo treatment by 0.155 ([pm]3.109) [cm.sup.3].
Although the differences in these four measurements during active and placebo treatment were not statistically significant, they do indicate a positive trend.
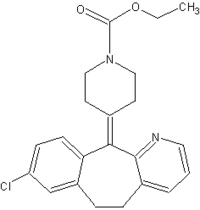
Endoscopic photography. Two photographs of the inferior turbinate of each patient were evaluated for the amount of redness, edema, and secretions (table 2; figure). Results:
Redness. During loratadine/pseudoephedrine treatment, the mean redness score improved by 1.00 ([pm]6.0) point; during placebo treatment, the mean score decreased by 1.10 ([pm]4.07) points.
Edema. The mean edema score improved an average of 4.10 ([pm]6.0) points during active treatment; the difference between the pre-and post-treatment scores was statistically significant (p[less than]0.01). The mean edema score also improved slightly during placebo treatment (0.20 [[pm]4.9]), but the difference between pre- and post-treatment values was not statistically significant.
Secretions. The mean secretion score improved by a statistically significant 2.60 ([pm]5.1) points (p[less than]0.04) during active treatment, and worsened by 2.10 ([pm]6.2) points during placebo treatment.
Quality-of-life questionnaire. All 20 patients answered the quality-of-life surveys at each session (table 3). Findings:
Nasal symptoms. The difference in mean nasal symptom scores before and after loratadine/pseudoephedrine treatment was 0.60 ([pm]1.16) points. This difference was statistically significant (p[less than]0.04) and met Juniper et al's definition of a "minimally important difference" (MID: [geq]0.5). [9] The difference in mean nasal symptom scores before and after placebo was only 0.07 ([pm]1.85) points, which was neither clinically important nor statistically significant.
Eye symptoms. The pre- and post-treatment difference in mean eye symptom scores was 0.57 ([pm]1.32) points during loratadine/pseudoephedrine therapy. This represented a clinically important improvement, and it approached, but did not reach, statistical significance (p[less than]0.08). The difference before and after placebo treatment was 0.14 ([pm]1.31) points, which was not significant either clinically or statistically.
Other symptoms. The mean score for symptoms other than those involving the nose and eyes rose 0.18 ([pm]0.77) points after loratadine/pseudoephedrine treatment, but the difference was not clinically important or statistically significant. The same was true of the difference during placebo treatment (0.13 [[pm]1.27]).
Daily activities. Neither active treatment nor placebo had a clinically or statistically significant effect on the performance of daily activities (0.23 [[pm]0.81] and 0.10 [[pm]1.43], respectively).
Practical problems. The mean score representing practical problems rose 0.47 ([pm]1.23) points after active treatment, a figure that was not statistically significant but was clinically important. The increase after placebo treatment was 0.45 ([pm]1.42) points, which was not statistically significant but did approach clinical importance.
Quality of sleep. The patients' quality of sleep appeared to worsen slightly after loratadine/pseudoephedrine treatment, as the mean score fell 0.12 ([pm]1.40) points. However, this decrease was neither clinically important nor statistically significant. Likewise, the apparent improvement in sleep after placebo (0.28 [[pm]1.67]) was not clinically important or statistically significant.
Emotional status. The increase in the mean emotional status score after loratadine/pseudoephedrine treatment was 0.40 ([pm]0.98), which approached both clinical importance and statistical significance (p[less than]0.09). There was virtually no difference in emotional status scores after placebo (-0.01 [[pm]1.16]).
Visual analog symptom scale. We analyzed five nasal symptoms (table 4) and four eye symptoms (table 5) as rated by each patient on the visual analog symptom scale. Findings:
Nasal domains. The mean stuffy nose score increased by 3.3 ([pm]36.53) points after loratadine/pseudoephedrine treatment and decreased by 4.90 ([pm]30.58) points after placebo. On the other hand, rhinorrhea worsened following active treatment, as the mean score decreased by 6.75 ([pm]21.23) points; during placebo, the mean score increased by 6.25 ([pm]31.85) points, but the difference between the study medication and placebo values was not significant. The mean score for nasal or throat itching improved slightly following active treatment (1.0 [[pm]28.02]) and worsened with placebo (-3.30 [[pm]37.221). Mean postnasal drip scores worsened after both active treatment (-2.75 [[pm]23.29]) and placebo (-1.50 [[pm]36.52]). Mean sneezing scores improved with both loratadine/pseudoephedrine (5.85 [[pm]22.63]) and placebo (6.85 [[pm]22.21]); there was no statistically significant difference between the two.
Eye domains. Improvements in mean eye itching scores were 4.20 ([pm]29.60) points with loratadine/pseudoephedrine and 6.15 ([pm]29.36) with placebo--not a significant difference. Mean scores for both watery eyes and sore or red eyes also improved in both groups (5.20 [[pm]25.37] and 3.85 [[pm]20.65], respectively, for watering, and 2.55 [[pm]30.39] and 2.25 [[pm]27.67] for soreness or redness). Finally, there was a slight improvement in the mean score for swollen eyes after loratadine/pseudoephedrine treatment (0.40 [[pm]20.23]), and a slight worsening with placebo (-0.60 [[pm]16.94]), but the difference was not significant.
Discussion
Our study focused primarily on nasal congestion because it is often extremely bothersome. We used acoustic rhinometry to measure nasal congestion because it has been found to be reliable in giving an objective assessment of nasal patency. [10] Rhinometry shows the cross-sectional area of the entire nasal cavity and essentially provides a topographic map of the nose. Hilberg et al found that cross-sectional measurements on acoustic rhinometry are reliable. [7] Rhinometry has a coefficient of variation of less than 2%, and it provides a good correlation between actual volume and total measured nasal volume. Grymer et al found a highly significant correlation between the minimal nasal cross-sectional area on acoustic rhinometry and the subjective feeling of nasal patency as reported by patients." [11] Quantification of nasal cross-sectional areas on acoustic rhinometry is independent of airflow. Rhinometry is also minimally invasive and is particularly useful for performing repeat measurements in rapid successio n. Therefore, we considered it to be a reasonable objective test to quantitatively measure changes in nasal congestion.
Our results show that loratadine/pseudoephedrine treatment increased nasal cross-sectional area and nasal volume, whereas the effects of placebo were inconsistent, with a slight decrease in the mean CSA1, CSA2, and nasal volume measurements and a very slight mean increase in the CSA3 measurement. Loratadine/pseudoephedrine treatment resulted in a positive trend in each acoustic rhinometry domain. The fact that the degree of improvement did not reach statistical significance is most likely the result of the small number of patients for whom we had complete acoustic rhinometry data.
We also used endoscopic inferior turbinate photography because some researchers have found that it is a valuable tool for studying nasal patency objectively. [12-14] Our results show that loratadine/pseudoephedrine treatment alleviated redness and edema in the inferior turbinates, decreased the amount of nasal secretions, and improved the overall appearance of the nose. Treatment with placebo was associated with an increase in redness and secretions. The decreases in inferior turbinate edema and secretions following loratadine/pseudoephedrine treatment were statistically significant, as was the overall nasal improvement. Our results with endoscopic inferior turbinate photography support the use of loratadine/pseudoephedrine for alleviating nasal congestion in patients with seasonal allergic rhinitis.
The rhinoconjunctivitis quality-of-life questionnaire was developed by Juniper and Guyatt to measure various factors that are important to patients with rhinoconjunctivitis. [8] In studies involving patients with perennial allergic rhinitis and those with seasonal allergic rhinitis, this questionnaire has been reported to be reproducible, responsive, and valid. [1,2,8] The MID is the smallest amount of change in any of these factors that patients perceive to be beneficial and which would mandate, in the absence of troublesome side effects or excessive cost, a change in the patient's management. [15] The MID for the rhinoconjunctivitis quality-of-life questionnaire has been determined by Juniper et alto be a change greater than approximately 0.5. [9] Applying this formula to our results, we found that treatment with loratadine/pseudoephedrine was associated with an improvement in nasal and eye symptoms, both of which were clinically important. The improvement in nasal symptoms was also statistically significa nt, while the improvement in eye symptoms and in the total quality-of-life questionnaire score approached significance.
The results of visual analog testing were inconsistent. Visual analog scale scores indicated that loratadine/pseudoephedrine treatment alleviated nasal stuffiness, nasal and throat itchiness, and sneezing, but worsened rhinorrhea and postnasal drip. All eye symptoms improved with both active treatment and placebo, and there was no significant difference in eye results. A number of investigators have found visual analog scales to be unreliable in subjectively assessing nasal congestion. Indeed, a seven-point Likert scale, such as that used in the rhinoconjunctivitis quality-of-life questionnaire, has been found to be easier to administer and interpret in terms of how much change constitutes an MID. [16]
In conclusion, there was a good correlation between symptom improvement and the findings seen on acoustic rhinometry, endoscopic inferior turbinate photography, and the quality-of-life questionnaire, but not with visual analog scores. We find that once-a-day fixed-combination loratadine/pseudoephedrine is effective in relieving the nasal congestion in patients with seasonal allergic rhinitis.
Acknowledgment
The authors express their appreciation to Tammie Ismail, Mohammed Ahmed, Robert Nelson, and Patrice Al- Saden, RN, for their contributions to the completion of this article.
From the Allergy Clinic, Section of Otolaryngology-Head and Neck Surgery, University of Chicago Medical Center (Dr. McFadden, Mr. Moinuddin, and Dr. Corey), the Department of Otolaryagology, University of Pittsburgh School of Medicine (Dr. Gungor), Metro (Hospital) Manila, the Philippines (Dr. Ng), and the Northwestern University Medical School, Chicago (Dr. Mamikoglu).
This study was supported by a research grant from the Schering Corp.
References
(1.) Juniper EF, Guyatt GH, Andersson B, Ferrie PJ. Comparison of powder and aerosolized budesonide in perennial rhinitis: Validation of rhinitis quality of life questionnaire. Ann Allergy 1993;70:225-30.
(2.) Juniper EF, Guyatt GH, Dolovich J. Assessment of quality of life in adolescents with allergic rhinoconjunctivitis: Development and testing of a questionnaire for clinical trials. J Allergy Clin Immunol 1994;93:413-23.
(3.) Tarnasky PR, Van Arsdel PP Jr. Antihistamine therapy in allergic rhinitis. J Farm Pract 1990;30:71-80.
(4.) Dockhorn RJ, Bergner A, Connell JT, et al. Safety and efficacy of loratadine (Sch-29851): A new non-sedating antihistamine in seasonal allergic rhinitis. Ann Allergy 1987;58:407-l1.
(5.) Bronsky E, Boggs P, Findlay S, et al. Comparative efficacy and safety of a once-daily loratadine-pseudoeplsedrine combination versus its components alone and placebo in the management of seasonal allergic rhinitis. J Allergy Clin Immunol 1995;96:139-47.
(6.) Tandy JR, Mabry RL, Mabry CS. Correlation of modified radioallergosorbent test scores and skin test results. Otolaryngol Head Neck Surg 1996;115:42-5.
(7.) Hilberg O, Jackson AC, Swift DL, Pedersen OF. Acoustic rhinometry: Evaluation of nasal cavity geometry by acoustic reflection. J Appl Physiol 1989;66:295-303.
(8.) Juniper EF, Guyatt GH. Development and testing of a new measure of health status for clinical trials in rhinoconjunctivitis. Clin Exp Allergy 1991;21:77-83.
(9.) Juniper EF, Guyatt GH, Griffith LE, Ferrie PJ. Interpretation of rhinoconjunctivitis quality of life questionnaire data. J Allergy Clin Immunol 1996;98:843-5.
(10.) Lai VW, Corey JP. The objective assessment of nasal patency. Ear Nose Throat J 1993;72:395-6, 399-400.
(11.) Grymer LF, Hilberg O, Pedersen OF, Rasmussen TR. Acoustic rhinometry: Values from adults with subjective normal nasal patency, Rhinology 199l;29:35-47.
(12.) Roithmann R, Cole P, Chapnik J, et al. Acoustic rhinometry, rhinomanometry, and the sensation of nasal patency: A correlative study. J Otolaryngol 1994;23:454-8.
(13.) Watson WT, Roberts JR, Becker AB, et al. Nasal patency in children with allergic rhinitis: Correlation of objective and subjective assessments. Ann Allergy Asthma Immunol 1995;74:237-40.
(14.) Zedalis D, Dolen WK, Glover GC, et al. Evaluation of nasal patency by fiberoptic rhinoscopy. J Allergy Clin Immunol 1989;83:973-8.
(15.) Juniper EF, Goyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific Quality of Life Questionnaire. J Clin Epidemiol 1994;47:81-7.
(16.) Guyatt GH, Townsend M, Bernman LB, Keller JL. A comparison of Likert and visual analogue scales for measuring change in function. J Chron Dis 1987;40:1129-33.
(*.)Values for each measurement are the total for both sides of the nose.
(+.)Ranges for nasal volume are measured in [cm.sup.3].
Key to areas measured: CSA1 = cross-sectional area at the nasal valve; CSA2 = cross-sectional area at the ante nor portion of the inferior turbinate; CSA3 = cross-sectional area at the anterior portion of the middle turbinate.
Key to timing of measurements: BA = before active treatment; AA = afteractive treatment; BA-AA = diference in measurements before and after active treatment; BP = before placebo; AP = after placebo; BP-AP = difference in measurements before and after placebo.
The maximum score for each is 40.
(*.)Two photographs of the inferior turbinate of each patient were evaluated in a blinded fashion by two investigators for redness, edema, and secretions. Each of these symptoms was rated on a scale of 0 (none) to 5 (severe). Values represent the total scores obtained by adding the grades of both observers for both photographs for both sides of the nose.
Key to timing of measurements: BA = before active treatment; AA = after active treatment; BA-AA = difference in measurements before and after active treatment; BP = before placebo; AP = after placebo; BP-AP = difference in measurements before and after placebo.
COPYRIGHT 2000 Medquest Communications, Inc.
COPYRIGHT 2000 Gale Group