Abstract
Parkinson's disease (PD) is the most common movement pathology, severely afflicting dopaminergic neurons within the substantia nigra (SN) along with non-dopaminergic, extra-nigral projection bundles that control circuits for sensory, associative, premotor, and motor pathways. Clinical, experimental, microanatomic, and biochemical evidence suggests PD involves multifactorial, oxidative neurodegeneration, and that levodopa therapy adds to the oxidative burden. The SN is uniquely vulnerable to oxidative damage, having a high content of oxidizable dopamine, neuromelanin, polyunsaturated fatty acids, and iron, and relatively low antioxidant complement with high metabolic rate. Oxidative phosphorylation abnormalities impair energetics in the SN mitochondria, also intensifying oxygen free radical generation. These pro-oxidative factors combine within the SN dopaminergic neurons to create extreme vulnerability to oxidative challenge. Epidemiologic studies and long-term tracking of victims of MPTP (1-methyl-4-phenyl-1,2,3,6,-tetrahydropyridine) poisoning, suggest oxidative stress compounded by exogenous toxins may trigger the neurodegenerative progression of PD. Rational, integrative management of PD requires: (1) dietary revision, especially to lower calories; (2) rebalancing of essential fatty acid intake away from pro-inflammatory and toward anti-inflammatory prostaglandins; (3) aggressive repletion of glutathione and other nutrient antioxidants and cofactors; (4) energy nutrients acetyl L-carnitine, coenzyme Q10, NADH, and the membrane phospholipid phosphatidylserine (PS); (5) chelation as necessary for heavy metals; and (6) liver P450 detoxification support. (Altern Med Rev 2000;5(6):502-545)
Introduction
Parkinson's disease (PD) is the most common disease of motor system degeneration and, after Alzheimer's disease, the second most common neurodegenerative disease.[1] Parkinson's disease takes a heavy toll in mental anguish, lost productivity, and health care expenditures. PD prominently features dopamine transmitter insufficiency, and current management is almost exclusively reliant on dopamine replacement drugs. But, while these drugs are initially effective in most patients, they do not slow the underlying degeneration in the area of the brain most affected, the substantia nigra (SN). Their effectiveness declines over time and their adverse effects become increasingly more troublesome. Broader options for long-term management are urgently needed.
Many different lines of evidence have converged to suggest PD is primarily an oxidative disease, fueled by endogenous susceptibility and driven by the cumulative contributions of endogenous and exogenous (environmental) oxidant stressors. In this review the evidence for the various oxidative contributions to PD is critiqued, from the perspective of developing a more effective and necessarily more integrative strategy for its medical management.
A Disease of Progressive Neurodegeneration
Parkinson's disease was first described in 1817 by the physician James Parkinson.[2] Prior to this, accounts of the symptoms were remarkably scarce, which led many researchers to theorize whether this disease may have been a product of the beginning of the early 19th century and the Industrial Revolution in England.[1] Some speculated that, because certain environmental neurotoxins cause Parkinson's-like ("parkinsonian") symptoms, some contaminant in the new industrial environment may have increased its prevalence. This debate has continued to the present, with the evidence steadily accumulating in favor of oxidative causation linked to environmental toxins.
Parkinson's disease is widespread in Westernized countries. In the United States, for example, as many as one million people have PD with more than 50,000 new cases being diagnosed each year.[1] The disease is highly age-dependent: it can manifest as early as the mid-30s, but becomes more common past the age of 50, with 57 being the average age of diagnosis in the United States. Its prevalence in the over-50s U.S. population is above one percent, and in the over-80 population likely exceeds five percent.[3] PD is becoming more common with the overall aging of populations.
Parkinson's disease often first becomes noticeable as tremor in a limb, and as it progresses three other unmistakable symptoms arise:[1-3] bradykinesia (slowness of movement); rigidity (both "cogwheel"/jerkiness and "leadpipe"/stiffness); and posture instability with impaired gait, associated with the stooped stance characteristic of the disease. Bradykinesia may cause the patient to feel glued to the ground or to the chair in which they sit, and progressively erases body language and facial expressiveness. The disease is not restricted to motor degeneration -- as many as 35 percent of PD cases also develop dementia.[5]
Parkinson's disease is now recognized to be a widespread degenerative illness that affects not just the central nervous system, but also the peripheral and enteric systems.[4] Formerly the disease was typecast as motor system degeneration, yet sensory fields, association areas, and premotor fields become damaged throughout the brain (Figure 1). The limbic, autonomic, and neurosecretory control fields (hypothalamus) all show micro-anatomic damage. At the cellular level, neuron death in PD is more systemic than previously assumed: non-invasive imaging recently demonstrated that the nerve supply to the heart degenerates in PD subjects.[6] Biochemically, abnormalities of liver detoxification and mitochondrial oxidative phosphorylation also occur.[7,8]
[Figure 1 ILLUSTRATION OMITTED]
The pathological process that underlies PD typically is slow-paced but relentlessly progressive, the clinical symptoms tending to manifest relatively late in the pathological progression. Classically, the hallmark of PD has been degeneration of dopamine-producing neurons in the relatively small SN, most intensely localized in the zona compacta. The definitive Parkinson's disease diagnosis is still posthumous, the key features being neuron death in the SN accompanied by the presence of Lewy bodies and Lewy neurites.[9]
Normally, dopamine produced in the SN is moved to the caudate nucleus and the putamen, where it is involved in stimulating and coordinating the body's motor movements. In PD, neurons producing dopamine in the SN die, reducing the overall supply of dopamine and compromising the brain's capacity to effectuate movement. Curiously, dopamine-producing neurons outside of the SN tend not to be affected, though many other neuronal types -- glutamatergic, cholinergic, tryptaminergic, GABAergic, noradrenergic, adrenergic -- show "grievous cytoskeletal damage," according to Braak and Braak.[4]
The characteristic pattern of nerve cell destruction in SN neurons appears to be linked to abnormalities that develop in the cytoskeleton. The pathognostic Lewy bodies and Lewy neurites are composed mainly of abnormal cytoskeletal neurofilament proteins.[3,4] Neurons afflicted with Lewy formations remain viable for a relatively long period, but are functionally compromised and die prematurely. As a rule, projection neurons with long axons are more vulnerable than local circuit and projection neurons with short axons, which tend to be spared.[4]
Current Management of Parkinson's Disease
Parkinsonism is a term broadly applied to the subject presenting with movement impaired by rigidity, tremor, or extreme slowness (bradykinesia).[1] Parkinsonism can have various causes (Table 1): occupational exposure to manganese;[1] trauma to the brain;[9] viral inflammation of the brain, as with Encephalitis lethargica which struck five million victims during the years 1916-1926;[11] and exposures to toxins still unknown, such as that which has afflicted citizens of Guam.[12] The diagnosis of Parkinson's disease is reserved for cases confirmed by selective cell death in the SN.
Table 1: Classes of Prescription Drugs that can Precipitate Parkinsonian Symptoms. From Worst Pills, Best Pills.[10]
Antihypertensive, diuretic: Diupres, Enduronyl, Hydropres, Regroton, Demi-Regroton, Salutensin, Ser-Ap-Es
Antihypertensive, non-diuretic: Aldomet
Antidepressant: Asendin, Aventyl/Pamelor, Desyrel, Elavil, Limbitrol, Ludiomil, Luvox, Norpramin, Paxil, Prozac, Sinequan, Tofranil, Triavil, Wellbutrin, Zoloft
Antipsychotic: Compazine, Haldol, Mellaril, Navane, Prolixin, Risperdal, Stelazine, Thorazine, Triavil, Zyprexa
Other: Reglan, Zyban
Currently, PD is managed mainly through dopamine replacement therapy -- pharmaceutical agents aimed at replacing dopamine in the brain or mimicking its actions at dopamine receptors.[9] Most commonly used is the dopamine precursor levodopa in combination with carbidopa (Sinemet[R] and Sinemet CR). The vast majority of patients experience benefits initially, but rarely do the benefits persist. Typically, after 2-5 years on levodopa drugs the patient's responses become erratic. Nausea is a constant threat, and dyskinesias develop that feature excessive and uncontrollable movements. Other adverse effects develop: mental confusion, "freezing" and inability to move, dystonia, low blood pressure episodes, sleep disturbances, and hallucinations.[1,9]
Adverse side effects usually pose a major ongoing challenge to the PD patient.[10] For example, the combined effects of the disease and the drugs used to treat it produce sleep problems in an estimated 70 percent of patients and daytime hallucinations in about 30 percent. Levodopa is usually effective for motor symptoms at the beginning, but over time tends to cause motor fluctuations, dyskinesias, and other adverse side effects. These can become so disabling that surgical treatment becomes the only apparent option for restoring any quality of life.[13]
Other drugs used for PD symptom management include amantadine (Symmetrel[R]), selegiline (Eldepryl[R], deprenyl), dopamine agonists (bromocriptine, pergolide, pramipexole, ropinirole), and several anticholinergic drugs. All these have major adverse effects and generally are less effective than Sinemet[R] in suppressing symptoms. Tolcapone, an inhibitor of COMT (catechol-O-methyltransferase, the enzyme which normally inactivates dopamine), became available in 1998. It caused several deaths from liver failure.[1] Another COMT inhibitor -- entacapone -- was released in 1999 which was not liver-toxic but still caused dyskinesias, nausea, diarrhea, abdominal pain, and urine discoloration.[1]
As PD progresses, in addition to the adverse effects accruing from levodopa therapy the ever-worsening loss of dopamine neurons causes progressively crippling damage to motor control circuits throughout the brain.[4] The control may shift, so the pathways that normally inhibit movement come to dominate those that activate movement. The increasing desperation of the patient can become the rationale for risky surgical intervention; for example, whether to remove inhibitory zones or to implant electrodes aimed at restoring a healthy balance of circuits. [13-15]
Surgical destruction of brain tissue was tried prior to the advent of levodopa therapy, but produced inconsistent results. More recently, microelectrodes are being used to detect signals from individual brain cells, using these signals as "signposts" to arrive at more precise locations in the brain.[13] Pallidal and subthalamic nuclear surgery can improve motor symptoms and levodopa-induced dyskinesias, but only unilateral pallidotomy is acceptable since the bilateral procedure carries unacceptably high risk. The unilateral procedure, however, probably the most common surgery for advanced PD, unfortunately does not allow for postoperative reduction in levodopa doses. Postsurgical mortality is 1-1.8 percent, risk of permanent neurological deficit is about five percent, and benefits tend to dissipate within 1-4 years.
Deep-brain electrical stimulation (DBS) by way of surgically implanted electrodes has the advantages over ablation of being regulatable and reversible. DBS also has been bilaterally performed in many patients with marked benefit and little permanent morbidity.[14,15] DBS post-operative morbidity and mortality is less than for ablation, and the stimulation side effects are relatively mild.[15] On the negative side, infection may ensue, mechanical failure occurs in 3-4 percent of cases, batteries must be replaced at regular intervals, and the device is expensive. On the positive side, successful bilateral stimulation can allow medication dosing to be reduced, providing the patients a better quality of life. Although results from randomized studies are not yet available, surgeons who have done both ablation and DBS agree that DBS is better for the patient.
Obviously, the need to broaden the options for therapy in Parkinson's disease is urgent. This urgency compels renewed focus on the etiology and pathogenesis of the disease. Deeper scientific understanding of PD would lead to better preclinical detection and prophylaxis, validation of biomarkers, confirmation of genetic and environmental risk factors, and more prolonged symptom control with fewer adverse effects.
A Broad Spectrum of Potential Etiologic Factors
As with almost all disease states, a broad spectrum of both genetic and environmental factors have been suggested as contributing to the initiation and progression of PD. Aging is also implicated, with advanced age being the single most important risk factor for the disease.
Role of Aging
Parkinson's disease is clearly age-dependent. Several of the neurodegenerative syndromes documented in the elderly -- gait slowing, for example -- resemble those seen in PD and may be prodromal for the disease.[3] While the inexorable downhill slide of Parkinson's disease is unmistakably a disease process, aging undoubtedly contributes to PD progression, perhaps because of its accumulative oxidative damage and steady decrease of antioxidant capacity.
Heritability and Genetic Susceptibilities
There appears to be an inherited component to PD, and a number of family pedigrees with multiple cases of PD have been extensively studied.[16,17] To date, seven loci on four chromosomes are reliably linked to PD and/or to neurodegeneration of the parkinsonian type, not always with the presence of the Lewy structures. The protein products from two of these loci are linked to nerve cell damage in other neurodegenerative conditions. Alpha-synuclein, localized to chromosome 4, is a major component of the Lewy bodies, not just in PD but also in dementia with Lewy bodies and in the Lewy body variant of Alzheimer's disease.[16] Non-familial PD subjects carrying a specific alpha-synuclein allele and ApoE4, a high-risk allele for Alzheimer's, have a 13-fold increased risk of developing PD. Parkin, localized to chromosome 6, causes early-onset parkinsonism without the Lewy bodies that define PD.[16] Most PD cases, however, do not have other affected family members and have no apparent familial contribution.
One particularly good test system with which to quantify disease heritability is a twin study, in which disease frequency is compared between cohorts of identical twins and fraternal twins. If genetic factors are important, concordance in monozygous (MZ) twins, who are 100-percent genetically identical, will be greater than in dizygous twins, who are only 50-percent genetically identical. Tanner and a team of associates did such a twin study.[18]
Drawing from the U.S. World War II Veteran Twins Registry, Tanner's group compiled a pool of 19,842 white male twins. After exhaustive screenings and a series of in-depth diagnostic examinations, they confirmed 193 twins with PD among 172 twin pairs. They confirmed mono- vs. di-zygosity using polymerase chain reaction analysis of DNA. For the entire sample as a whole, with average age of onset of 64.5 years, there was no significantly greater concordance of the disease between identical twins than between fraternal twins, indicating no genetic linkage to PD. In contrast, for those who developed the disease earlier than age 50, further data analysis disclosed there was greater genetic concordance in the MZ twins. For this group, which represents 10-15 percent of the total PD cases, genetic linkage was not ruled out.[18]
With the key studies now done, the preponderance of the evidence indicates the general PD population has no more than a mild genetic contribution. Still, overall absence of defined heritability does not necessarily rule out subpopulations with higher heritability, or subtle genetically-conditioned vulnerabilities. Rohan de Silva et al[16] and Reiss et al[17] discuss how various specific gene mutations and deletions might potentially contribute to PD. The genes involved could act with varying degrees of penetrance, or polygenically contribute to disease vulnerability with no single gene being wholly responsible. Though better designed and more definitive than those that preceded it, the outcome of the Tanner study still leaves open possibilities in these areas. For early-onset PD, the cumulative evidence is consistent with a strong heritability component (at least in white males, the only group studied to date).[7,16,17]
Some individuals with PD have impaired liver detoxification. The P450 IID6 enzyme, which was characterized based on its capacity to metabolize debrisoquine, was found to be dysfunctional more frequently in PD subjects than in non-PD controls.[7] Of the PD subjects, those with very early onset ([is less than] age 40) were most likely to have this problem. The gene for P450 IID6 was localized to chromosome 22, and efforts are underway to develop it into a biomarker for early-onset PD, but this may not prove practical. Conducting such assays in vivo is expensive and laborious, and in the studies some of the medications being taken for PD may have complicated the outcomes.
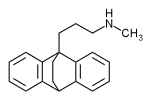
Interestingly, P450 IID6 is present in the nigrostriatal system and the notorious parkinsonian toxin, 1-methyl, 4-phenyl, 1,2,3,6-tetrahydropyridine (MPTP) is a substrate for this complex.[7] MPTP came to the forefront of PD research in 1982, when drug addicts in northern California began to develop severe parkinsonism after intravenous injection of a synthetic heroin that was contaminated with MPTP as a byproduct of its synthesis. [19]
Environmental Contributors, Especially Toxins
The MPTP poisonings led to a serendipitous finding: that the symptoms resulting from exposure to MPTP very closely matched the many features of PD.[19-21] This shifted the focus toward environmental factors as potential PD initiators or contributors. As the search progresses, a single toxic cause remains elusive but a role for environmental factors seems almost certain.
Whatever the exact degree of contribution from environmental toxins, currently the cumulative evidence suggests PD is a multifactorial oxidative disease. The main causal, oxidative contributors indicted to date are: (1) measurable amplification of the endogenous oxidative load by constitutive impairments of mitochondrial energy transformations; (2) innate vulnerability of the brain's substantia nigra region to oxidative challenge; and (3) initiation or promotion by toxic exposure(s) that further deplete antioxidants. These factors combine to initiate a downhill course for the neurons of the SN and elsewhere in the brain, the end result of which appears to be a slow-acting yet long-term progressing, inflammatory process. This eventually results in the micro-anatomic degeneration and clinical symptomatologies of Parkinson's disease.
Mitochondrial Energetics Generate Endogenous Oxidative Burden
All the body's cells, like oxygen-utilizing cells anywhere, generate life energy and simultaneously generate oxygen free radicals (oxyradicals). The resultant oxidative burden is an obligatory, unavoidable byproduct of oxygen-based (aerobic) respiration. Very early in the progression of life, the adoption of oxygen to drive energetics produced a higher energy yield from food molecules, but with a "downside." This downside was the production of oxyradicals, so highly reactive they have the potential to destroy the living system.[22] Antioxidant defenses developed, which curb the toxic threat from oxyradicals and help keep them integrated with the myriad pathways of healthy metabolism.[23] The major cellular "hot spots," where the bulk of oxyradicals are produced and antioxidant defenses are normally most challenged, are the semi-independent organelles called mitochondria.
Present in all human cells, the mitochondria are the cells' energy powerhouses since they generate the vast bulk of the ATP that drives life processes.[23] The mitochondria have their own DNA and manage the oxidative phosphorylation process ("oxphos"). In this process carbon-carbon double bonds are split to create pairs of energized electrons, whose electronic energy is then converted into the chemical bond energy of ATP. As the mitochondria utilize 90 percent or more of the cells' available oxygen to make ATP, they also generate 90 percent or more of the oxyradicals that make up the endogenous oxidative burden.[24]
The mitochondrial electron transfer complexes use highly electrophilic molecular oxygen to create an electronic potential gradient which "pulls" electrons through a series of five cytochrome-protein complexes. The complexes sequentially extract the electrons' energy, converting it to ATP (Figure 2); at the end the electrons are combined with hydrogen and oxygen to make water. However, during the transfers single electrons escape enzymatic control; these combine with oxygen to create oxygen free radicals, at a rate of around two percent of all oxygen consumed. To protect against destruction by this flux of oxyradicals, the mitochondria have sophisticated antioxidant defenses; but inevitably a few oxyradicals slip through to attack biomolecules. In PD this electron leakage is abnormally accentuated.[25]
[Figure 2 ILLUSTRATION OMITTED]
Flawed Energetics Characterizes Parkinson's Disease
Parkinson's disease subjects have been found to have abnormalities of oxidative phosphorylation that impair their mitochondrial energy generation and almost surely increase their endogenous oxidative burden. Research into mitochondrial energetics in PD was sparked by the observation that the notorious MPTP targets the mitochondria and inhibits their energetic function.[25] It is now clear that PD patients have mitochondrial energetic impairment which closely resembles that attributable to MPTP but is apparently constitutive in origin.[26-29]
The oxidative phosphorylation complexes are aggregates of enzymes, functionally linked and distributed in groups throughout the inner membranes of the mitochondria (Figure 2). The complexes I, II, III, IV, and V occur in spatial sequences that optimize electron transfer efficiency while minimizing the possibilities for single-electron "leakage" to oxygen that would generate oxyradicals.[25] The system is finely balanced: damage to any one complex both reduces ATP yield and worsens the inevitable leakage of oxyradicals from the system.
Schapira and coworkers[8] were the first to report that mitochondrial complex I activity was selectively reduced in the SN of patients with PD, and subsequently this was confirmed by others.[26-29] Haas et al[26] found this abnormality was not confined to the brain: using platelets purified from early-stage patients not on medication for PD, they documented abnormalities of complex I and possibly also complexes II and III in their mitochondria. The complex I impairment ranged from 16-54 percent, and was worse in more advanced cases of the disease. Complex I abnormalities were also described from non-nigral brain areas, muscle, and fibroblasts of PD subjects, but whether these really exist is still being debated.[25,27]
In metabolically extreme situations, as from exposure to hypoxia, hyperoxia, or metabolic poisons, the mitochondrial complexes can be shut down and the cell soon dies.[25] Complex I is especially sensitive to MPTP,[21] and, as mentioned above, is the same complex found to be hypofunctional in PD patients.[8,26,27] Complex I (NADH:ubiquinone oxidoreductase) serves as the principal entry point for electrons into the enzymatic transport chain. Like most other mitochondrial proteins, complex I is genetically coded for by the ring-shaped DNA of the mitochondrion. To help determine whether complex I is genetically abnormal, Swerdlow and colleagues[27] devised an experiment using "cybrids."
Swerdlow's group first produced a cultured line of human neuroblastoma cells that contained no mitochondrial DNA. Then they repopulated these cells with mitochondria prepared from the platelets of PD patients or healthy control subjects. This created matched populations of cybrids in which the cytoplasm was commonly shared, but the mitochondrial DNA came either from PD mitochondria or from non-PD (control) mitochondria. Using this elegant means for comparison, they could confirm that the PD mitochondria were at least 20-percent less efficient in complex I activity, produced higher levels of oxygen free radicals, and rendered their host cells more susceptible to MPTP-induced cell death. They suggested the complex I defect was based in the mitochondrial DNA of the PD patient. Such gene damage could come from parental inheritance or from oxidative attack upon the mitochondria. Whatever the primary source of the mitochondrial genic damage, enhanced complex I vulnerability (and perhaps damage to other complexes[28]) helps explain why some individuals develop PD following toxin exposure, while others do not.
Following on MPTP's emergence in 1982, intensive study of its action mechanisms rendered it an experimental model for exogenous oxidant toxins and yielded valuable insights on PD.[19-21,25,28,29] Technically, MPTP is a "protoxin." It is not toxic by itself but once it enters the brain becomes biotransformed to the toxic product [MPP.sup.+] (1-methyl-4-phenyl-pyridinium) by the enzyme monoamine oxidase B (MAO-B).[19,20] [MPP.sup.+] is a highly reactive free radical oxidant that is selectively taken up by the dopamine neurons of the substantia nigra, then once inside the neurons is selectively taken up by their mitochondria.[21] Within the mitochondrion [MPP.sup.+] readily inhibits complex I of the oxphos apparatus;[25] also inhibited may be the enzyme alpha-ketoglutarate dehydrogenase, which is located near complex I and also involved in energetics.[28,29]
[MPP.sup.+] infiltration of the cells' mitochondria, consequent to MPTP exposure, creates an alarming cellular scenario: extreme impairment of mitochondrial energy production for the cell, accompanied by amplification of oxygen radical production. Most likely a vicious cycle develops, wherein lowered energy production by the mitochondria heightens oxyradical formation, which causes oxidative damage, further lowering energy production until the cell dies. In an afflicted human progressing toward clinical expression of Parkinson's disease, this process takes years; MPTP produces parkinsonian symptoms within just days.
Substantia Nigra Vulnerable to Oxidative Stress
Oxidative stress exists when the oxidative burden on a living system is so great that effective antioxidant defenses cannot be maintained.[22,23] Intensified oxidative burden -- arising from increased endogenous production of oxyradicals and/or from excessive exposure to exogenous oxidative agents -- threatens to shift the finely balanced oxidation-reduction state away from reduction and towards oxidation. If sufficiently sustained, oxidative stress can impose lasting oxidative imbalance on the living system, hastening its demise.[30]
The brain carries a high endogenous oxidative burden. First, by having myelin sheaths the neurons are particularly enriched in polyunsaturated lipids. Due to their high density of carbon-carbon double bonds, these lipids are prime targets for oxidative attack.[22] Second, the brain consumes a disproportionately high share of the body's oxygen intake, creating a correspondingly high flux of endogenous oxyradical formation. Third, the activities of the antioxidant enzymes catalase and peroxidase are abnormally low in the brain. The superoxide dismutase enzymes are active, acquiring superoxide oxyradical as it leaks out of the mitochondrial complexes and converting it to hydrogen peroxide ([H.sub.2][O.sub.2]). But in the virtual absence of catalase and peroxidase, which normally would detoxify these peroxide products, the burden for detoxifying [H.sub.2][O.sub.2] is shunted onto the glutathione peroxidase enzyme. This enzyme uses glutathione (GSH) as its essential cofactor, and when it is adaptively induced the brain's GSH reserves are likely rendered more prone to depletion from oxidative attack.[30] Multiple studies confirm that the brain's substantia nigra region is abnormally depleted of GSH in PD patients.[31-34]
The substantia nigra's unique biochemistry renders it even more vulnerable to oxidative stress than the brain as a whole. Its unique biochemical features are:
(1) A high content of dopamine, consequent to the high density of dopaminergic neurons in the SN. Dopamine has a strong tendency to spontaneously break down into oxidant metabolites by "auto-oxidation;" most reactive among these auto-metabolites are 6-hydroxydopamine quinone and dopamine aminochrome.[35] Dopamine's oxidative breakdown also can be accelerated by free (ionized) iron or by other redox-active elements such as copper, zinc, or manganese.[37]
(2) An extremely high content of iron, higher even than in the liver,[34,36,37] and most concentrated in the SN's zona compacta which becomes most damaged in PD.[36] It has been suggested that when iron reaches such high concentrations in cells it can escape buffer control by ferritin and the other iron-binding proteins.[37] It could then (via the Fenton reaction) catalytically convert hydrogen peroxide to generate the highly reactive hydroxyl radical, which can damage DNA and all other classes of biomolecules.[22,35,36] Substantia nigra iron levels measure even higher in patients with advanced disease.[36]
The protein alpha-synuclein, normally a presynaptic constituent, in its aggregated form is a prominent component of the Lewy aggregates that develop in the SN of Parkinson's patients.[4] Experimentally, ionized iron, in addition to copper and zinc, will catalyze its transformation into aggregates.[38] Copper is sometimes elevated in the cerebrospinal fluid of advanced PD patients, but its in vivo relationship (if any) with alpha-synuclein aggregation is not yet apparent.
(3) High activities of the two monoamine oxidase enzymes (MAO-A and B), which normally function to degrade dopamine to products that include hydrogen peroxide. MAO-B activity increases with aging.[39]
(4) High content of melanin (dopamine-melanin).[37,39] This complex macromolecular material can be formed from the auto-oxidation of dopamine. Its normal function appears to be the scavenging of free radicals. But when infiltrated with high levels of ionized iron, it can drive the Fenton reaction and exacerbate the conversion of endogenous hydrogen peroxide to the potent hydroxyl radical.[37] The population of melanin-enriched, dopaminergic neurons found in the SN's zona compacta are the worst affected in PD. Melanin within the SN could act as a support matrix upon which ionized iron would catalyze oxyradical generation from available hydrogen peroxide or from neuromelanin itself.[39]
(5) Low GSH content relative to other brain areas.[32-34,37] In animal and cell-level experiments, depletion of nigrostriatal GSH enhanced sensitivity to oxidants and to complex I impairment. GSH depletion seemingly occurs early in the disease pathogenesis, so it may be a central factor in the process.[37,40]
Techniques are available to detect and quantify oxidative stress in vivo. Table 2 shows that many of the universally accepted oxidative stress indicators are significantly abnormal in the SN of the Parkinson's patient.
Table 2: Indications of Oxidative Stress in the Substantia Nigra of Parkinson's Disease Patients.
* Mitochondrial abnormalities, linked to heightened oxyradical production[25]
* Substantial (40%) to marked (90%-plus) depletion of GSH (glutathione, glutathione reduced)[32,33,37]
* Degree of GSH depletion correlates with severity of neuron loss and with disease severity[33,34]
* Elevated lipid peroxides, hydroperoxides, and malondialdehyde, and decreased polyunsaturated fatty acids[40,42]
* Increased SOD (superoxide dismutase) activity, generating elevated hydrogen peroxide in absence of elevated peroxidases to detoxify it[43]
* Increased oxidative damage to DNA and proteins[40,41,44]
The substantia nigra, and particularly its zona compacta, carries so many pro-oxidant biochemical risk factors it could well be an oxidative "accident waiting to happen." One such accident could be Parkinson's disease, provoked by oxidant insult from outside the SN.[40]
Glutathione Depletion Pivotal in Parkinson's Disease
Environmental agents implicated in the etiology of PD include pesticides, oxidant transition and heavy metals (iron, copper, zinc, manganese, mercury, lead, aluminum), and certain food-borne toxic agents, all of which can readily be categorized as oxidative stressor agents. What all these diverse agents have in common is their capacity to challenge the fragile antioxidant status of the SN and deplete its GSH content. The evidence strongly suggests glutathione depletion is the pivotal event in Parkinson's etiology.
Glutathione is a potent molecular antioxidant, a conjugation cofactor for the liver P450 system, and an essential cofactor for the glutathione peroxidase family of antioxidant enzymes.[23,33,37] GSH also plays higher-level roles in metabolism: anti-inflammatory, antitoxin, and metabolic regulator.[31] Its levels are homeostatically maintained inside the living cell, where the self-adjusting mechanisms for maintaining GSH are numerous. GSH levels may well be a life gauge: that is, for as long as its levels are maintained the living cell is healthy and functional, and once it is severely depleted the cell is destined to die.[31,45]
Evidence is growing that GSH depletion contributes to neurodegenerative diseases. In numerous animal models of GSH depletion, the blockage at birth of the animal's capacity for GSH synthesis distorts brain development. In young or adult animals, GSH blockage results in neuronal pathology. Specific clinical evidence in Parkinson's disease also points to GSH depletion as the common thread. Bains and Shaw[45] gathered together the various threads and assembled them into the model summarized in Figure 3.
[Figure 3 ILLUSTRATION OMITTED]
The features of this model most relevant to PD are GSH degradation in the SN, and its overlap with the presence of oxidative stressors. A source of oxidative stress need not be just a toxin -- it can be insufficiency of dietary antioxidants or mineral enzyme cofactors, impairment of antioxidant enzyme synthesis, or the overall decline of antioxidant defense capacity with advancing age. Furthermore, the negative synergy between GSH depletion and oxidative stress certainly need not result only in PD. This GSH-depletion model predicts the clustering of neurodegenerative disease symptoms sometimes clinically observed in the same individual, including Alzheimer's disease, amyotrophic lateral sclerosis (ALS), and PD.
The Bains and Shaw model of pathologic GSH depletion also predicts that populations most at risk for developing diseases such as PD, Alzheimer's, and ALS are those at the low end of the overall range for GSH.[45] They propose that "low-glutathione" individuals exist in the population, "primed" for initiation of PD or other neurodegenerative progression. Glutathione depletion could arise in various ways, including genetic propensity, poor diet, pharmaceutical treatment (as with acetaminophen use), or as a function of age. An Italian clinical team reported that intravenous administration of GSH to newly-diagnosed PD patients resulted in marked improvement in motor ability in nine patients.[46] These findings were substantiated by Perlmutter in the United States.[2]
Potential Exogenous Triggers for Parkinson's
In its most healthy state the substantia nigra is more vulnerable to oxidative attack than probably any other brain region. Its unique co-enrichments with dopamine, monoamine oxidases, iron, and melanin all contribute to this excessive degree of vulnerability. The SN also carries the mitochondrial complex I defect, which lowers energy production and intensifies endogenous oxygen free radical production. Then there is the aging factor: as the decades pass, antioxidant defenses tend to become less competent. Conceivably the SN decompensates only from endogenous oxidative stress, but the evidence argues for an additional exogenous event or insult. What, then, is the trigger that finally sets in motion the SN's degenerative breakdown?
This question cannot be satisfactorily answered, but clues do exist. One clue comes from a mixed ALS-parkinsonism dementia complex specific to the island of Guam.[12,47] An exogenous toxic influence is known to be involved, but no single agent has been confirmed beyond doubt. Prime candidates are the DNA poison cycasin from the false sago palm (Cycas circinalis),[47] or two excitotoxins that also come from this palm. In addition, there is the high aluminum content of the soil, and zinc contamination of food prepared from this palm.[12] Some experts speculate that combinations of these factors could be acting in synergy.
Another food-borne category of potential neurotoxins is the [Beta]-carbolines (harman, norharman, TaClo)[48] and the tetrahydroisoquinolines (TIQ), which are structurally similar to [MPP.sup.+].[40] Some of these have been isolated from the brain, cerebrospinal fluid, and plasma of PD patients. They also are consumed in foods such as cheese, cocoa, bananas, milk, eggs, and beef, and they cross the blood-brain barrier.[29] The [Beta]-carboline TaClo can be endogenously formed from tryptamine, following exposure to chloral or trichloroethylene, and the TIQs can be formed in the brain from catecholamine condensation with aldehydes.[40] Although they are described as "weak neurotoxins," the long-term effects of chronic exposure have not been well explored.
Heavy metals and transition metals that accumulate at or near the SN are potential triggers for PD. Occupational exposure to iron, aluminum, or manganese for more than 30 years greatly increases the risk of acquiring PD (odds ratio 13.64, p [is less than] 0.05);[49,50] manganese overexposures often manifest as parkinsonism. Iron, though essential for life, is highly redox-active and chronically high levels could escape protein buffering and promote oxyradical generation.[35]
Acting to some degree like iron, which is highly oxidative, mercury, lead, zinc, and copper all have oxidant activity. All are capable of intensifying oxyradical generation in vivo and depleting tissue antioxidant stores. Mercury crosses the blood-brain barrier, and a case-control study conducted in Singapore has linked body burden of this element to the diagnosis of PD.[51]
Pesticides have now become highly suspect as potential Parkinson's disease triggets.[52,53] A connection was long suspected between PD and rural living, including the drinking of contaminated well water or exposures to pesticides or herbicides, as well as industrial exposures to chemicals and heavy metals.[54] Cases have been reported of workers with exposure to multiple pesticides and early-onset PD.[50] Earlier, epidemiological studies suggested an etiological relationship between PD and pesticide exposure; dieldrin which is a mitochondrial poison was specifically implicated.[53] A more recently completed study added further likelihood to the possibility that pesticides trigger PD.[55]
Dr. Lorene Nelson, a neuroepidemiologist at Stanford University School of Medicine in Palo Alto, California, and colleagues did a study of 496 persons diagnosed with PD and compared them with 541 matched controls.[55] Using structured interviews, they determined that home exposure to insecticides and herbicides was associated with increased risk of PD. Fungicide exposure did not emerge as statistically significant. Upon further analysis, in-home insecticide exposure for nongardeners was found to pose higher risk (twice normal) than outside gardening with herbicides (1.7x) or insecticides (1.5x).
Parkinson's Initiation May Not Require Extended Exposure
Parkinson's disease is deceptively complex, but as a result of the MPTP experience real progress has been made toward understanding the mechanisms operative in the disease. A few high-dose exposures to MPTP by the intravenous route can trigger parkinsonian symptoms that very closely resemble PD.[19,20] MPTP's startling toxicity is an exaggerated though faithful model for PD wherein, due to molecular abnormalities, the mitochondria become targeted by an exogenous oxidant toxin. This compromises energy supply, magnifies oxidative load thus depleting antioxidant resources, and destroys the vulnerable substantia nigra.
Following their initial report on MPTP toxicity,[19] Langston and collaborators followed the fates of a small number of more severely affected MPTP victims.[20] After seven years, they used positron emission tomography (PET) imaging with labeled fluorodopa to assess striatal dopamine function in 10 subjects originally exposed to MPTP for very short periods.[56] The PET findings closely matched the clinical records and indicated nigrostriatal function in these subjects was declining more rapidly than in normal aging.
As the years went by, Langston's group continued long-term patient tracking, and obtained samples from the brains of three individuals not long after death.[20] They found convincing evidence that, following an initial brief period of MPTP exposure years previous, some of the victims had progressed to bona fide Parkinson's disease. All three had originally injected MPTP for no more than a week in 1982, and they died 3, 12, and 16 years after the initial exposure. At death all had active neuronal degeneration and a type of reactive histopathology in the SN that strikingly resembled the pattern established for PD, though they had not used MPTP since their initial exposure.
These findings from Langston can be taken to suggest that a transient toxic exposure -- even a relatively short, one-week period of exposure to MPTP -- initiated a slowly progressive brain pathology that continued to worsen for as long as 16 years until the death of the patient. They reported their findings were indicative of "active, ongoing nerve cell loss," suggesting that, "a time-limited insult to the nigrostriatal system can set in motion a self-perpetuating process of neurodegeneration."[20] They suggested three possible mechanisms to explain these dramatic findings: (1) oxidative stress; (2) treatment of the subjects' initial parkinsonian symptoms with levodopa, which could enhance dopamine production in overworked and hypofunctional SN neurons and further promote dopamine oxidation; and (3) a self-perpetuating inflammatory process. None of these mechanisms excludes the others; on the contrary, the available findings suggest all three are simultaneously active in the Parkinson's brain. Parkinson's disease appears to be a multifactorial disease, initiated and probably driven by oxidative factors.
This multifactorial, oxidative stress model for Parkinson's disease is consistent with the considerable body of clinical data on PD. It carries a sobering implication: the thousands of oxidant chemicals that contaminate the air, water, soil, and food could act singly or in combination to trigger disease progression. Foods depleted of antioxidants, oxidant pharmaceuticals, or lifestyle factors that raise oxidative load (smoking, drinking, chronic virus load) could all contribute. If the toxic exposure is at relatively low concentration but sustained over time, the process can be set into motion but take years or decades to clinically manifest. The aging process also may come into play: a younger individual may be comparatively resistant to toxic triggers unless genetically susceptible, whereas an older person might be rendered comparatively defenseless against oxidant attack.
The pattern of cell breakdown and inflammation evident in the PD brain is unique to PD. It exhibits some of the predictable features of nerve tissue reaction to damage, including microglial activation[57,58] and increases in cytokines such as transforming growth factor-beta (TGF-[Beta]-1) and tumor necrosis factor-alpha (TNF-[Alpha]).[59] Atypical features include a conspicuous absence of astrocytic activation[60] and no evidence of apoptotic cell death.[58] Just how this unique mix of processes combine to create the inexorable progression of brain degeneration still remains to be deciphered. Until more definitive evidence emerges, the strategy for attempted prophylaxis of PD, and for its long-term medical management, must be fully integrative and take into account all possible contributory factors.
L-Dopa Likely Contributes to Disease Progression
The standard medical therapy for PD continues to be levodopa, usually with carbidopa added to prolong its retention (Sinemet, Sinemet CR). Levodopa is the most immediate biochemical precursor to dopamine, the neurotransmitter depleted due to breakdown of the substantia nigra. This therapy does not ameliorate the underlying progressive loss of dopamine-producing neurons and over the long term may contribute to PD progression.
Parkinson's patients treated with levodopa sometimes develop elevated plasma homocysteine (HCy).[61] Hyperhomocysteinemia is a major risk factor for vascular disease.[62] SAMe (s-adenosyl methionine, a methyl-activated metabolite of methionine) is a key metabolic contributor to the recycling of HCy.[60] Levodopa was found to deplete SAMe from the central nervous system of human subjects, and perhaps poses a threat to the homeostatic regulation of homocysteine.[63]
Muller and colleagues[64] measured plasma HCy in Parkinson's patients treated with levodopa, and compared them with Parkinson's subjects not previously treated, and healthy controls. HCy levels were almost twice as high in the levodopa-treated PD patients as compared with the non-treated group and the healthy group (p [is less than] 0.001 and p [is less than] 0.002, respectively); plasma HCy of the non-treated Parkinson's patients did not significantly differ from the healthy participants. Dangerously elevated plasma HCy may provide a key to the increased mortality attributed to vascular disease in patients with PD.[65] These findings also suggest PD patients taking levodopa might benefit from concomitant supplementation with folate and vitamin B12, both of which help recycle HCy.
Nutrient Deficiencies in Parkinson's Disease
The brain uses the same nutrients that other organs use; therefore, all nutrient classes can be useful to Parkinson's patients. Many nutrients have been found deficient in PD, and others are likely to be deficient at some point during disease progression.[66]
Certain individual amino acids are precursors to brain neurotransmitters and significantly ameliorate symptoms when given as dietary supplements. Tyrosine, phenylalanine, and tryptophan can all be blocked from absorption by levodopa, thereby becoming deficient. L-tyrosine is a direct precursor to levodopa, which is then converted to dopamine. Deficiency may develop due to reduced intake from meat, dairy and eggs, or to diminished enzymatic conversion from phenylalanine. PD patients also may have impaired capacity to utilize L-tyrosine,[67] even though it may be normally absorbed.[68] In 1989, Lemoine and collaborators reported L-tyrosine gave better clinical results and had many fewer side effects than levodopa when tested in a small group of patients.[66] L-tyrosine should not be taken at the same time of day as levodopa, since it competes for absorption.
D-phenylalanine is another amino acid that should not be taken with levodopa.[66] The D-form (DPA specifically; not the L-form) was reported to improve rigidity, walking, speech difficulties, and psychic depression, but not tremor.[69] L-tryptophan also competes with levodopa for absorption.[66] Parkinson's disease patients treated with levodopa can manifest low serum tryptophan,[70] and L-tryptophan therapy often helps them break through their depression.[71] In a placebo-controlled study, L-tryptophan produced improvements in functional ability beyond those afforded by levodopa, and also significantly improved mood and drive.[72] Given with niacin and pyridoxine, L-tryptophan was useful in ameliorating the motor complications from long-term levodopa therapy.[66]
L-methionine is an essential amino acid, and its supplementation may benefit PD. In one study, 15 patients who had maximal improvement from standard medications were increased gradually from 1 g/day to 5 g/day.[73] Ten of the 15 improved on all measures except tremor and drooling.
A number of B vitamins may be deficient in PD patients. In one reported case, deficiency of folic acid due to an inborn error of folate metabolism generated parkinsonian symptoms which included progressive hypokinesia, tremor, rigidity, and "pill-rolling," with deficiency of dopamine though SN degeneration was not found at autopsy.[74] Niacin can become deficient in patients treated with levodopa, especially if it is given with carbidopa or other decarboxylase inhibitors.[75] Supplementation with niacin may prolong elevated brain levodopa levels.[76]
In the case of vitamin B6, treatment with levodopa alone often raises the levels of this vitamin, so co-supplementation is contraindicated.[77] By contrast, treatment with the commonly prescribed levodopa-carbidopa combination may provoke a marginal B6 deficiency, and supplementation with B6 can benefit at least some of these patients.[78,79] Vitamin B6 can be injected intraspinally with thiamine, for partial symptomatic relief.[66]
Vitamin C (ascorbic acid) is sometimes found decreased in Parkinson's brains.[34] One double-blind trial in PD found supplementation produced a modest improvement in functional performance.[66] In 1975, Sacks and Simpson reported 4 g/day ascorbic acid lessened nausea and other levodopa side effects in the case of a 62-year-old man.[80] When alternated between ascorbic acid and placebo (citric acid) under double-blind conditions, his patterns of improvement correlated with the periods of receiving ascorbic acid.
Vitamin E supplementation may be important for PD patients. A 1988 survey of the dietary habits of PD patients prior to the age of 40 revealed that intakes of nuts, oils, and plums relatively high in vitamin E were associated with lowered risk of PD.[66] Previous clinical studies using high doses of encapsulated vitamin E suggested this vitamin has an important role in slowing disease progression.[81,82]
Disagreement exists as to whether copper is elevated or deficient in PD. It was reported elevated in the cerebrospinal fluid of Parkinson's patients, the degree of elevation being significantly correlated with both disease severity and rate of progression.[83] The researcher suggested copper chelation be used therapeutically in these cases. However, others reported copper in the SN region was abnormally low.[84,85]
Glutathione becomes more depleted from the SN as the disease progresses (Figure 4).[34] N-acetyl cysteine[86] and alpha-lipoic acid contribute to GSH repletion and are also potent antioxidants. Building on the highly positive findings from Italy -- that intravenous GSH benefited all nine patients with early PD[46] -- the pioneering Perlmutter Center offers intravenous GSH as the most direct means for GSH repletion.[2]
[Figure 4 ILLUSTRATION OMITTED]
Integrative Management of Parkinson's Disease
With the evidence steadily accumulating that Parkinson's disease is a multifactorial oxidative disease, there is an urgent need for integrative management. The allopathic model that currently dominates Parkinson's management is obsolete. The major adverse side effects of the various drugs currently in use for the disease, combined with the limitations of the dopamine replacement strategy, dictate the need for alternatives.
The classic Parkinson's progression -- depletion of dopamine-producing neurons from the substantia nigra, the accumulation of Lewy bodies -- no longer represents the pathobiology of this disease. A systemic pattern for PD is evident from the findings of multiple control circuit damage throughout the brain; damage along the various nondopaminergic pathways; peripheral nerve degeneration; changes in the heart; mitochondrial insufficiency in brain and probably in muscle and platelets; and defective P450 detoxification. This broadened understanding of the disease dictates that its medical management strategy also be broadened.
Dietary Revision
Decreasing protein intake is useful in PD. For patients being maintained on levodopa, high protein intake typical of Western lifestyle may interfere with levodopa availability and contribute to episodic loss of symptomatic control by the drug (the "off-on" phenomenon). Mena and Cotzias[87] assessed several levels of protein intakes, and found low intake (0.5 g/kg/day) improved symptomatic control throughout the day, while high intake (10 g/kg/day) exaggerated the off-on pattern. Seven patients were maintained for up to a year on low protein intake; six of them maintained stability with five achieving reductions of levodopa doses. These early results were confirmed in subsequent clinical studies.[88-90]
In a double-blind study that compared low protein intake (50 g/day for men and 40 g/day for women) to high protein intake (80 g/day for men and 70 g/day for women), total performance scores were significantly improved, along with tremor, hand agility, and mobility in the low protein groups.[88] In another study, modifying meal patterns to eat the majority of protein in the evening also improved symptoms.[89] These effects were unrelated to levodopa absorption or blood levels; perhaps they are due to some central action of high dietary protein[88] or variation in the plasma content of large amino acids.[89]
Reducing caloric and fat intakes is also important. Logroscino and his collaborators from Columbia University[91] surveyed the dietary intakes of 110 PD and 287 non-PD subjects in New York City. They found PD patients consumed significantly more calories (p [is less than] 0.0001), their energy-adjusted fat intake was significantly higher (p [is less than] 0.007), and an increasing intake of animal fats was strongly related to PD (p [is less than] 0.001, odds ratio 5.3, 95% confidence interval 1.8-15.5). Intakes of antioxidants were not significantly different between the groups. These findings are worthy of further investigation; they are consistent with a report from England that cardiovascular disease, also linked to high fat, high calorie diets, is a more predominant cause of death among PD patients than the general population.[65]
Caloric reduction has been under scrutiny for some time as a means to better health and extended longevity. Considerable personal discipline is required to adhere to the regimen, but the scientific findings are very clear: less calories consumed translates into decreased free radical production. This is an important means of lowering endogenous oxidative load, which is linked to aging progression.[92] Reduction of lipid calories is also integral to this strategy, because lipids are the foremost substrates for peroxidative attack coming from endogenous oxidative overload. In addition, high animal fat consumption generally results in a pro-inflammatory shift in the tissues due to the preponderance of long-chain omega-6 content.[93] Parkinson's patients may be well advised to rebalance their dietary fatty acid sources by minimizing saturated fats and increasing long-chain omega-3 intakes while reducing their total caloric intake.
Metal Detoxification
Iron occurs at very high concentrations in the SN, wherein it normally is bound to ferritin. Free unbuffered iron likely worsens the oxidative degenerative process in PD, so periodic monitoring of iron saturation status is strongly indicated. Mercury can access the brain by volatilizing from dental fillings, or by crossing the blood-brain barrier after becoming absorbed from foods.
A landmark Singapore study assessed mercury body burden and linked this to risk of PD.[51] Fifty-four cases of confirmed PD were compared to 95 hospital-based controls. PD was accurately diagnosed, then mercury body burden indirectly assessed via blood and urine levels. The relative risk for PD was 8.5x for blood Hg [is greater than] 5.9 ng/mL (95% confidence interval 2.2-33.2), and 14.8x for urine Hg [is greater than] 6.8 ng/ mL (95% confidence interval 3.5-63.7). Dentists occupationally exposed to mercury in Singapore averaged above this range, and unexposed office workers averaged below it. A "zero load" approach to mercury detoxification should be the norm, wherein all sources of mercury exposure are eliminated. Where mercury contamination is identified, chelation should be used to eliminate it from the body.[94]
Systemic Glutathione Replacement
With the evidence so overwhelming that GSH depletion is a central event in PD,[32,33,37] and that the degree of GSH depletion is worse in advanced disease (Figure 4, lower), effective repletion of GSH must be a therapeutic priority. Combined intravenous and oral GSH replacement is safe and well tolerated, providing ongoing benefit. As oral GSH precursors both N-acetylcysteine[95] and alpha-lipoic acid are appropriate. GSH is also a systemic antioxidant, and its ongoing repletion may help ameliorate Parkinson's-related damage in the heart, liver, muscles, and other organs.[31]
Systemic GSH status is also conserved by bolstering other antioxidant defenses. Especially noteworthy is high-dose vitamin C, which provides antioxidant reducing equivalents known to conserve GSH. Intravenous ascorbate is a long-established and proven protocol.[96] Taken together with vitamin C, vitamin E probably also helps delay PD progression.
In 1979, believing oxidative stress could be a major factor causing neuronal death in PD, Dr. Stanley Fahn, a neurologist at Columbia University, began prescribing relatively high doses of vitamins C (3 g/day) and E (3,200 IU/day) for his PD patients.[81] As controls he used data on patients from another physician, who managed her cases almost identically to his practice but did not administer antioxidants. After tracking 21 patients for a number of years, Fahn's group found early-onset patients (onset [is less than] 54 years) maintained on high doses of vitamins C and E were able to delay levodopa or deprenyl therapy by about 25 months when compared with matched controls. The later-onset patients (54+ years) were able to delay the transition to drugs by about 35 months.
Subsequently, a large, multicenter, double-blind trial was organized. In this DATATOP study (Deprenyl and Tocopherol Antioxidant Therapy of Parkinson's)[82] the Parkinson's Study Group evaluated 2,000 IU of tocopherol and 10 mg of deprenyl per day in 800 subjects with early PD. Primary endpoint for the study was disability sufficient to prompt the decision to begin taking levodopa. The outcome was that deprenyl treatment delayed disability for almost nine months, whereas tocopherol treatment (at 2000 IU/day, lower than Fahn's study) was not found to extend delay. This finding should not be unexpected since nutrient antioxidants often work together in coordinated biochemical defense rather than acting singly.[23,42]
Comprehensive GSH conservation requires additional oral supplementation with the entire range of nutrient antioxidants and antioxidant enzyme mineral co-factors. However, since PD causes considerable nervous system damage prior to becoming symptomatic, antioxidant intervention may slow further progression but is unlikely to completely restore function unless implemented prior to clinical emergence of the disease. Bains and Shaw suggest a prophylactic strategy for PD, including screening at early middle-age to detect individuals with low-glutathione status.[45]
Essential fatty acids may have benefits for PD symptoms. Evening primrose oil, enriched in the anti-inflammatory, omega-6 gamma-linolenic acid, was reported to relieve tremor.[98] The omega-3 fatty acids, especially DHA and EPA in fish oils, tend to reduce pro-inflammatory cytokine production in vivo.[99,100] Due to their high propensity for oxidation they should be administered in conjunction with high intakes of antioxidants. Octacosanol, a long-chain alcohol found in wheat germ oil, was reported to be helpful in PD. In a double-blind crossover trial, 3 of 10 patients significantly improved and none worsened, with no adverse side effects experienced.[101] The means by which this nutrient is benefiting PD is not immediately evident.
Revitalizing the Parkinson's Brain
Given the confirmed presence of mitochondrial energetic abnormalities in the substantia nigra and elsewhere in the afflicted brain,[26,27,29] nutrients that safely boost mitochondrial function deserve further exploration for clinical benefit in PD. Coenzyme Q10 (ubiquinone; CoQ10) is an electron acceptor and antioxidant that is a key component of mitochondrial electron transfer.[24] Two separate groups reported CoQ10 was significantly reduced in mitochondria taken from the brain[97] and platelets[102] of PD patients (Figure 4, upper). Lowered complex I activity was strongly correlated with reduced mitochondrial content of CoQ10.
Shults and collaborators gave three different oral doses of CoQ10 with vitamin E daily to 15 PD patients and, after one month, found complex I activity was increased.[103] At 600 mg/day of CoQ10, complex I activity doubled to well within the range for healthy subjects, but small sample sizes precluded attainment of statistical significance. Since the mitochondrial CoQ10 balance may be shifted from the reduced form to the oxidized form in PD,[102] the oxidative drain placed on CoQ10 may be extreme. Additional supplementation with other mitochondrial support nutrients -- nicotinamide adenine dinucleotide (NADH), acetyl-L-carnitine, and phosphatidylserine (PS) -- could diversify energy input to the mitochondria and further help compensate for the energetic impairment of PD.
NADH is an electron energy carrier also indispensable to mitochondrial oxidative phosphorylation. Birkmayer and collaborators pioneered its application in PD.[104,105] Reasoning that exogenous levodopa down-regulates its own endogenous biosynthesis, they sought to boost endogenous dopamine production via the intrinsic pathways.[104] After finding that NADH did boost dopamine production in cultured nerve cells, they conducted an open-label trial on PD patients.[105] They treated 415 patients intravenously and 470 by the oral route. Using patients as their own controls, they found similar benefits between intravenous and oral NADH. For oral NADH the mean improvement of disability was 19.8 percent, for intravenous 20.6 percent; maximum improvement was 55 and 60 percent, respectively, and 36 percent of patients experienced better than 10-percent benefit. Subsequently, Kuhn and collaborators confirmed the benefit of intravenous NADH.[106]
Acetyl-L-carnitine is another mitochondrial energy carrier, activating transport into the mitochondria of fatty acids to be used for energy. This nutrient has energizing, protective, and trophic effects.[107] In animal experiments it partially protected the SN against [MPP.sup.+] attack, enhanced dopaminergic transmission, and boosted intrinsic growth factor production.[107,108]
Phosphatidylserine is a fundamental component of the mitochondrial membrane systems on which are assembled the electron transfer complexes. It is also a membrane building block for the synaptic and other neuronal membranes, and plays a key role in electro-chemical transmission between the neurons. Whole-brain imaging with PET showed PS can markedly enhance energetics throughout the brain.[107] In an open-label trial conducted on Parkinson's patients in Germany, PS provided greater than 10-percent benefit to 7 of 12 subjects.[109]
For the busy integrative physician to consolidate all these approaches into a cohesive protocol the patient can manage is not an easy task. One example where this has been accomplished, and a paramount resource for integrative management of PD, is the Perlmutter Health Center in Naples, Florida. The center's director, David Perlmutter, MD, developed the protocol summarized in Table 3.
Table 3: The Perlmutter Protocol-- Integrative Parkinson's Disease Management.[2]
* Glutathione (reduced, GSH), intravenous, 600-1,000 mg 3 times per week
* Cellular Energizers: Coenzyme Q10 120 mg, NADH 5 mg (twice daily), PhosphatidylSerine 100 mg daily
* Antioxidants: Vitamin C (ascorbic acid) 800 mg, Vitamin E (d-alpha-tocopherol) 1200 IU, alpha-Lipoic acid 80 mg, N-AcetylCysteine (NAC) 400 mg, Ginkgo biloba extract (standardized 24/6) 60mg, Acetyl-L-Carnitine 400 mg, Vitamin D 400 IU, daily.
* Other nutrients: Vitamin B3 (as niacinamide) 100 mg, Vitamin B6 (as pyridoxine) 100 mg, Vitamin B12 (as cyanocobalamin) 200 mcg, Folic acid 800 mcg, Magnesium (as citrate) 420 mg, Zinc (as an "amino acid chelate") 20 mg, daily.
* In PD patients less than 65 years of age, check liver detoxification capacity and treat with milk thistle extract and other liver support nutrients as necessary.
Upcoming Advances in Integrative Management
The inexorable downhill slide that currently characterizes Parkinson's disease can be ameliorated through early and aggressive intervention based on an integrative protocol as exemplified in Table 3. Over the longer term, medical mastery over this disease awaits advances in presymptomatic detection and risk assessment, and in effective brain restoration. Relevant to these goals, several promising technological breakthroughs are on the horizon.
Functional Whole-Brain Imaging
Tomographic imaging, both by PET and SPECT (single photon emission tomography), offers exciting possibilities for improved preclinical detection and for assessment of severity and progression. At the cellular level in the brain abnormalities are discernible years before the disease becomes clinically manifest, but these can only be visualized microscopically following biopsy. Functional whole-brain imaging is superior because it is non-invasive, is becoming increasingly more available, and can now detect and quantify dopamine activity in the living brain. As shown in Figure 5, PET examination using perfusion with 18F-6-fluorodopa label can effectively probe decreased dopaminergic function in the brain (putamen) prior to the appearance of clinical symptoms.[110],[111]
[Figure 5 ILLUSTRATION OMITTED]
Following its intravenous administration, 18F-6-fluorodopa is taken up by the nigrostriatal dopaminergic projections and decarboxylated to labeled dopamine and dopamine metabolites. This conversion is imaged at high resolution using PET. Parkinson's patients imaged with PET revealed an average 50-percent loss of dopamine uptake by the putamen.[111] These data could be compared to the average 60-80 percent loss of SN zona compacta cells as quantified from postmortem sampling. As putamen dopamine levels become reduced by 90 percent in end-stage PD, PET shows the nigrostriatal projections are making virtually no dopamine.
Patients with newly emergent, one-sided PD show by PET a 30-percent dopamine loss, which matches the 30-percent nigral cell loss threshold (counted at autopsy) for symptom emergence. In one case, the technique detected impaired dopamine metabolism five years prior to symptom emergence.[111] This could be extremely valuable for risk assessment in asymptomatic, at-risk individuals, including relatives with known PD pedigrees.
Using a new 3-dimensional signal integration approach, 18F-dopa PET and other sophisticated whole-brain labeling technology can now detect reduced dopamine uptake in all patients with emergent PD, and demonstrate progressive reductions in the striatal, nigral, and cingulate levels of dopamine storage as the disease progresses.[112] PD can now be discriminated from atypical parkinsonian conditions with 80-percent accuracy, and non-PD conditions that feature reduced dopamine metabolism (striatonigral degeneration, multiple system atrophy) can also be quantified and discriminated from PD.
Clinical rating scales are notoriously imprecise for estimating PD progression. 18F-dopa PET and related imaging provide a more objective approach to staging, especially since disease duration correlates with dopaminergic decline. The preclinical "window" of dopaminergic decline prior to symptom emergence is estimated at 6 [+ or -] 3 years using imaging,[113] whereas estimates from nigral cell counts set this period at an average 4.5 years.[111]
Neuroprotection
The allopathic approach to PD management continues to generate new pharmaceuticals, with the hope of eventually replacing levodopa with a comparably effective and less toxic monotherapy. Potential neuroprotective monotherapies are receiving high priority. Among the drugs already utilized for PD management, selegiline and amantadine appear to have neuroprotective properties.[114] Epidemiologic and clinical evidence suggests estrogens can be protective in PD,[115] and PET-controlled comparisons suggest ropinirole may be protective at early stages.[114] In a baboon model of PD, nitric oxide synthase inhibitors blocked the biochemical and clinical manifestations of MPTP toxicity.[116] In a rat model of PD, infusions of the opiate receptor antagonist naloxone partially protected against SN damage.[117] In cultures of dopaminergic neurons, the cytokines IL-1[Beta] and IL-6 protected against [MPP.sup.+] toxicity.[118] Other possible neuroprotectors for PD are MAO-B inhibitors, NMDA-receptor antagonists, and dopamine receptor agonists.[114] A few experts have suggested a "multi-neuroprotective" strategy be explored, which hopefully is a prelude to an eventual "meeting of the minds" on integrative management of PD.
Neural Transplantation
Attempts to replace dopamine-secreting neurons within the disease-ravaged substantia nigra, using transplanted adrenal medullary or fetal tissue, successfully demonstrated that such tissue can partially survive the transplantation process, become established, and produce dopamine in the new tissue environment.[119] To date, a few patients have benefited from this landmark procedure, and no doubt relative success will improve as the technique is improved. However, transplanted dopamine neurons have not been able to fully replace the needed amounts of dopamine. Future transplant methodology is likely to place greater priority on stem cells and/or cultured cell lines as the tissue source, probably in closer conjunction with growth factors and other cell-activating substances.
Stem Cells, Growth Factors, and Gene Therapy
Recent unequivocal demonstration that stem cells are present in the human brain has created a new dimension of possibilities for regeneration of the central nervous system.[120] This advance is particularly timely for PD, wherein the earlier limited successes with tissue transplantation have prepared the ground for stem cell transplants which should have better implantation potential. Now growth-promoting trophic substances, or growth factors are being employed to improve the possibilities for survival of the transplant. One factor already being utilized for this purpose is glial cell line-derived neurotrophic factor.[121] Vasoactive intestinal peptide helps nerve cells in culture to conserve their GSH stores[122] Still, from the integrative perspective the challenge is to induce the Parkinson's brain to endogenously produce the needed variety and combinations of growth factors (probably in synergy with stem cells) that would accomplish brain revitalization.
In the more distant future, gene therapy using transplantation of genetically engineered cells, or direct insertion of genes into a patient's brain cells, may prove clinically feasible,[123] Skin and muscle cells genetically altered to overproduce tyrosine hydroxylase have been successfully transplanted into MPTP-parkinsonian monkeys, where they survived, integrated well into the brain, and produced dopamine for several months. A great deal of basic research remains, in order to develop effective biological vectors for gene insertion, to ensure inserted genes will continue to function, and to identify other gene products than dopamine-synthesizing enzymes likely to benefit the disease.
Until that time when such heroic, high-tech medicine has become effective, safe, and financially affordable, the available clinical experience suggests that PD management can be markedly improved by following an integrative medical model. This more rational and more resourceful medical approach would embrace non-invasive early detection, rendering dopamine replacement the last resort rather than the first; pursue nerve tissue restoration before surgical intervention; and win for the Parkinson's disease patient years of productive well-being.
References
[1.] Saunders CD. Parkinson's Disease: A New Hope. Boston, MA: Harvard Health Publications; 2000.
[2.] Perlmutter D. BrainRecovery.com: Powerful Therapy for Challenging Brain Disorders. Naples, FL: The Perlmutter Health Center (www.brainrecovery.com); 2000.
[3.] Waite LM, Broe GA, Creasey H, et al. Neurological signs, aging, and the neurodegenerative syndromes. Archs Neurol 1996;53:498-502.
[4.] Braak H, Braak E. Pathoanatomy of Parkinson's disease. J Neurol 2000;247 Suppl. 2:3-10.
[5.] Brown RG, Marsden CD. How common is dementia in Parkinson's disease? Lancet 1984; 2:1262-1265.
[6.] Goldstein DS, Holmes C, Li ST, et al. Cardiac sympathetic denervation in Parkinson disease. Ann Intern Med 2000;133:338-347.
[7.] Tanner CM. Liver enzyme abnormalities in Parkinson's disease. Geriatrics 1991;46:S60-S63.
[8.] Schapira AHV, Mann VM, Cooper JM, et al. Anatomic and disease specificity of NADH CoQ1 reductase (complex I) deficiency in Parkinson's disease. J Neurochem 1990;55:2142-2145.
[9.] Olanow CW, Jenner P, Youdim M. Neurodegeneration and Neuroprotection in Parkinson's Disease. New York, NY: Academic Press; 1996.
[10.] Wolfe SM, Sasich LD, Hope RE, et al. Worst Pills, Best Pills. New York: Pocket Books; 1999.
[11.] Casals J, Elizan TS, Yahr MD. Postencephalitic parkinsonism - a review. J Neural Transm 1998;105:645-676.
[12.] Stone R. Guam: deadly disease dying out. Science 1993;261:424-426.
[13.] Krack P, Poepping M, Weinert D, et al. Thalamic, pallidal, or subthalamic surgery for Parkinson's disease? J Neurol 2000;247 Suppl. 2:122-134.
[14.] Bejjani BP, Dormont D, Pidoux B, et al. Bilateral subthalamic stimulation for Parkinson's disease by using three-dimensional stereotactic magnetic resonance imaging and electrophysiological guidance. J Neurosurg 2000;92:615-625.
[15.] Jahanshahi M, Ardouin A, Brown RG, et al. The impact of deep brain stimulation on executive function in Parkinson's disease. Brain 2000;123:1142-1154.
[16.] Rohan de Silva HA, Khan NL, Wood NW. The genetics of Parkinson's disease. Curt Opin Gen Dev 2000;10:292-298.
[17.] Reiss O, Kuhn W, Krueger R. Genetic influence on the development of Parkinson's disease. J Neurol 2000;247 Suppl 2:69-74.
[18.] Tanner CM, Ottman R, Goldman SM, et al. Parkinson disease in twins. JAMA 1999;281:341-346.
[19.] Langston JW, Ballard P, Tetrud JW, Irwin I. Chronic parkinsonism in humans due to a product of meperidine-analog synthesis. Science 1983;219:979-980.
[20.] Langston JW, Fomo LS, Tetrud J, et al. Evidence of active nerve cell degeneration in the substantia nigra of humans years after 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine exposure. Ann Neurol 1999;46:598-605.
[21.] Sayre LM. Biochemical mechanism of action of the dopaminergic neurotoxin MPTP. Toxicol Lett 1989;48:121-149.
[22.] Kidd PM, Levine SA. The biochemistry of free radicals. In: Levine SA, Kidd PM ed. Antioxidant Adaptation: Its Role in Free Radical Pathology. El Cerrito, CA: PMK; 1985.
[23.] Kidd PM. Natural antioxidants, first-line defense (Chapter 6). In: Kidd PM, Huber W ed. Living With the AIDS Virus: A Strategy for Long-Term Survival. E1 Cerrito, CA: PMK; 1991.
[24.] Kidd PM, Huber W, Summerfield F, et al. Coenzyme Q1O: Essential Energy Carrier and Antioxidant. El Cerrito, CA: PMK Biomedical; 1988.
[25.] Reichmann H, Janetsky B. Mitochondrial dysfunction -- a pathogenetic factor in Parkinson's disease. J Neurol 2000;247 Suppl. 2:63-68.
[26.] Haas RH, Nasirian F, Nakano K, et al. Low platelet mitochondrial complex I and complex II/III activity in early untreated Parkinson's disease. Ann Neurol 1995;37:714-722.
[27.] Swerdlow RH, Parks JK, Miller SW, et al. Origin and functional consequences of the complex I defect in Parkinson's disease. Ann Neurol 1996;40:663-671.
[28.] Mizuno Y, Saitoh H, Sone N. Inhibition of mitochondrial alpha-ketoglutarate dehydrogenase by 1-methyl-4-phenylpyridinium ion. Biochem Biophys Res Comm 1987; 143:971-976.
[29.] Mizuno Y, Ikebe S, Hattori N, et al. Role of mitochondria in the etiology and pathogenesis of Parkinson's disease. Biochim Biophys Acta 1995;1271:265-274.
[30.] Levine SA, Kidd PM. Antioxidant Adaptation: Its Role in Free Radical Pathology. San Leandro, CA: Biocurrents/Allergy Research Group; 1985.
[31.] Kidd PM. Glutathione: systemic protectant against oxidative and free radical damage. Altern Med Rev 1997;2(3):155-176.
[32.] Perry TL, Godin DV, Hansen S. Parkinson's disease: a disorder due to nigral glutathione deficiency? Neurosci Lett 1982;33:305-310.
[33.] Jenner P. Oxidative mechanisms in nigral cell death in Parkinson's disease. Mov Disord 1998;13:S24-S34.
[34.] Riederer P, Sofic E, Rausch W, et al. Transition metals, ferritin, glutathione, and ascorbic acid in parkinsonian brains. J Neurochem 1989;52:515-520.
[35.] Pezzella A, d'Ischia M, Napolitano A, et al. Iron-mediated generation of the neurotoxin 6-hydroxydopamine quinone by reaction of fatty acid hydroperoxides with dopamine: a possible contributory mechanism for neuronal degeneration in Parkinson's disease. J Med Chem 1997;40:2211-2216.
[36.] Jellinger K, Paulus W, Grundke-Iqbal I, et al. Brain iron and ferritin in Parkinson's and Alzheimer's diseases. J Neural Transm Park Dis Dement Sect 1990;2:327-340.
[37.] Youdim MBH, Ben-Schachar D, Riederer P. Is Parkinson's disease a progressive siderosis of substantia nigra resulting in iron and melanin induced neurodegeneration? Acta Neurol Scand 1989;126:47-54.
[38.] Paik SR, Shin HJ, Lee JH. Metal-catalyzed oxidation of alpha-synuclein in the presence of copper(II) and hydrogen peroxide. Arch Biochem Biophys 2000;378:269-277.
[39.] Youdim MBH, Ben-Schachar D, Riederer P. The role of monoamine oxidase, iron-melanin interaction, and intracellular calcium in Parkinson's disease. J Neural Transm 1990;32:S239-S248.
[40.] Foley P, Riederer P. Influence of neurotoxins and oxidative stress on the onset and progression of Parkinson's disease. J Neurol 2000;247 Suppl. 2:82-94.
[41.] Jellinger KA. Cell death mechanisms in Parkinson's disease. J Neural Transm 2000;107:1-29.
[42.] Dexter DT, Carter CJ, Wells FR, et al. Basal lipid peroxidation in substantia nigra is increased in Parkinson's disease. J Neurochem 1989;52:381-389.
[43.] Martilla RJ, Lorentz H, Rinne UK. Oxygen protecting enzymes in Parkinson's disease: increase of superoxide dismutase-like activity. J Neurol Sci 1988;86:321-331.
[44.] Kanda S, Bishop JF, Eglitis MA, et al. Enhanced vulnerability to oxidative stress by alpha-synuclein mutations and C-terminal truncation. Neuroscience 2000;97:279-284.
[45.] Bains JS, Shaw CA. Neurodegenerative disorders in humans: the role of glutathione in oxidative stress-mediated neuronal death. Brain Res Rev 1997;25:335-358.
[46.] Sechi G, Deledda MG, Bua G, et al. Reduced intravenous glutathione in the treatment of early Parkinson's disease. Progr Neuropsychopharmacol Biol Psychiatry 1996;20:1159-1170.
[47.] Zhang ZX, Anderson DW, Mantel N, Roman GC. Motor neuron disease on Guam: geographic and familial occurrence, 1956-85. Acta Neurol Scand 1996;94:51-59.
[48.] Kuhn W, Mueller T, Rommelspacher H. Elevated levels of harman and norharman in cerebrospinal fluid of parkinsonian patients. J Neural Transm 1996;103:1435-1440.
[49.] Zayed J. Environmental factors in the etiology of Parkinson's disease. Can J Neurol Sci 1990;17:286-291.
[50.] Hirsch EC, Brandel JP, Galle P, et al. Iron and aluminum increase in the substantia nigra of patients with Parkinson's disease: an x-ray microanalysis. J Neurochem 1991;56:446-451.
[51.] Ngim CH, Devathasan G. Epidemiological study on the association between body burden mercury level and idiopathic Parkinson's disease. Neuroepidemiol 1989;8:128-141.
[52.] Bocchetta A, Corsini GU. Parkinson's disease and pesticides. Lancet 1986;2:1163.
[53.] Fleming L, Mann JB, Bean J, et al. Parkinson's disease and brain levels of organochlorine pesticides. Ann Neurol 1994;36:100-103.
[54.] Tanner CM, Langston JW. Do environmental toxins cause Parkinson's disease? A critical review. Neurology 1990;40 Suppl.3:17-31.
[55.] Stephenson J. Exposure to home pesticides linked to Parkinson's disease. JAMA 2000;283:3055-3056.
[56.] Vingerhoets FJG, Snow BJ, Tetrud JW, et al. Positron emission tomographic evidence for progression of human MPTP-induced dopaminergic lesions. Ann Neurol 1994;36:765-770.
[57.] McGeer PL, Itagaki S, Boyes BE, McGeer EG. Reactive microglia are positive for HLA-DR in the substantia nigra of Parkinson's and Alzheimer's disease brains. Neurology 1988;38:1285-1291.
[58.] Banati RB, Daniel SE, Blunt SB. Glial pathology but absence of apoptotic nigral neurons in long-standing Parkinson's disease. Mov Disord 1998;13:221-227.
[59.] Vawter MP, Dillon-Carter O, Tourtellote WW, et al. TGFbetal and TGFbeta2 concentrations are elevated in Parkinson's disease in ventricular cerebrospinal fluid. Exp Neurol 1996;142:313-322.
[60.] Mirza B, Hadberg H, Thomsen P, Moos T. The absence of reactive astrocytosis is indicative of a unique inflammatory process in Parkinson's disease. Neuroscience 2000;95:425-432.
[61.] Kuhn W, Roebroek R, Blom H, et al. Elevated plasma levels of homocysteine in Parkinson's disease. Eur Neurol 1998;40:225-227.
[62.] Chambers JC, McGregor A, Jean-Marie J, Kooner JS. Acute hyperhomocysteinaemia and endothelial dysfunction. Lancet 1998;351:36-37.
[63.] Surtees R, Hyland K. L-3,4-dihydroxyphenylalanine (levodopa) lowers central nervous system S-adenosylmethionine concentrations in humans. J Neurol Neurosurg Psychiatr 1990;53:569-572.
[64.] Muller T, Werne B, Fowler B, Kuhn W. Nigral endothelial dysfunction, homocysteine, and Parkinson's disease. Lancet 1999;354:126-127.
[65.] Ben-Shlomo Y, Marmot MG. Survival and cause of death in a cohort of patients with parkinsonism: possible clues to etiology. J Neurol Neurosurg Psychiatr 1995;58:293-299.
[66.] Werbach MR. Nutritional Influences on Illness. Tarzana, CA: Third Line Press; 1993.
[67.] Yamaguchi T, Nagatsu T. Effects of tyrosine administration on serum biopterin in normal controls and patients with Parkinson's disease. Science 1983;219:75-77.
[68.] Growdon JH, Melamed E, Logue M, et al. Effects of oral L-tyrosine administration on CSF tyrosine and homovanillic acid levels in patients with Parkinson's disease. Life Sci 1982;30:827-832.
[69.] Heller B, Fischer E, Martin R. Therapeutic action of D-phenylalanine in Parkinson's disease. Arzneim Forsch 1976;26:577-579.
[70.] Lehmann J. Tryptophan malabsorption in levodopa-treated parkinsonian patients. Acta Med Scand 1973;194:181-189.
[71.] Lehmann J. Levodopa and depression in Parkinsonism. Lancet 1971;1:140.
[72.] Coppen A, Metcalfe M, Carroll JD, Morris JG. Levodopa and L-tryptophan therapy in Parkinsonism. Lancet 1972;1:654-658.
[73.] Smythies JR, Halsey JH. Treatment of Parkinson's disease with L-methionine. Southern Med J 1984;77:1577.
[74.] Clayton PT, Smith I, Harding B, et al. Sub-acute combined degeneration of the cord, dementia and parkinsonism due to an inborn error of folate metabolism. J Neurosurg Psychiatry 1986;49:920-927.
[75.] Bender DA, Earl C J, Lees AJ. Niacin depletion in parkinsonian patients treated with L-dopa, benserazide and carbidopa. Clin Sci 1979;56:89-93.
[76.] Black MJ, Brandt RB. Nicotinic acid or N-methyl nicotinamide prolongs elevated brain dopa and dopamine in L-dopa treatment. Biochem Med Metab Biol 1986;36:244-251.
[77.] Mars H. Effect of chronic levodopa treatment on pyridoxine metabolism. Neurology 1975;25:263-266.
[78.] Baker AB. Treatment of paralysis agitans with vitamin B6 (pyridoxine hydrochloride). JAMA 1941;May 31:2484-2488.
[79.] Zeligs MA. Use of pyridoxine hydrochloride (vitamin B6) in parkinsonism. JAMA 1941;May 10:2148-2149.
[80.] Sacks W, Simpson GM. Ascorbic acid in levodopa therapy. Lancet 1975;1:527.
[81.] Fahn S. A pilot trial of high-dose alpha-tocopherol and ascorbate in early Parkinson's disease. Ann Neurol 1992;32:S128-S132.
[82.] Parkinson's Study Group. Effects of tocopherol and deprenyl on the progression of disability in early Parkinson's disease. New Engl J Med 1993;328:176-183.
[83.] Pall HS, Williams AC, Blake DR, et al. Raised cerebrospinal-fluid copper concentration in Parkinson's disease. Lancet 1987;2:238-241.
[84.] Dexter DT, Wells FR, Lees AJ, et al. Increased nigral iron content and alterations in other metal ions occurring in brain in Parkinson's disease. J Neurochem 1989;52:1830-1836.
[85.] Uitti RJ, Rajput AH, Rozdilsky B, et al. Regional metal concentrations in Parkinson's disease, other chronic neurological diseases, and control brains. Can J Neurol Sci 1989;16:310-314.
[86.] Martinez M, Martinez N, Hernandez Al, Ferrandiz ML. Hypothesis: can N-acetylcysteine be beneficial in Parkinson's disease? Life Sci 1999;64:1253-1257.
[87.] Mena I, Cotzias GC. Protein intake and treatment of Parkinson's disease with levodopa. New Engl J Med 1975;292:181-184.
[88.] Tsui JK, Ross S, Poulin K, et al. The effect of dietary protein on the efficacy of L-dopa: a double-blind study. Neurology 1989;39:549-552.
[89.] Carter JH, Nutt JG, Woodward WR, et al. Amount and distribution of dietary protein affects clinical response to levodopa in Parkinson's disease. Neurology 1989;39:552-556.
[90.] Pare S, Barr SI, Ross SE.. Effect of daytime protein restriction on nutrient intakes of free-living Parkinson's disease patients. Am J Clin Nutr 1992;55:701-707.
[91.] Logroscino G, Marder K, Cote L, et al. Dietary lipids and antioxidants in Parkinson's disease: a population-based, case-control study. Ann Neurol 1996;39:89-94.
[92.] Walford RL, Walford L. The Anti-Aging Plan. New York: Four Walls Eight Windows; 1995.
[93.] Kidd PM. Cell membranes, endothelia, and atherosclerosis - the importance of dietary fatty acid balance. Altern Med Rev 1996;1:148-167.
[94.] Frackelton JP, Christensen RL. Mercury poisoning and its potential impact on hormone regulation and aging: preliminary observation using a new therapeutic approach. J Adv Med 1998:11:9-25
[95.] van Zandwijk N. N-Acetylcysteine (NAC) and glutathione (GSH): antioxidant and chemopreventive properties, with special reference to lung cancer. J Cell Biochem 1995;Suppl 22:24-32.
[96.] Cathcart RF. Vitamin C (Ascorbate): Comprehensive History and Protocols. Los Altos, California, USA: www.orthomed.com; 2000.
[97.] Shults CW, Haas RH, Passov D, Beal MF. Coenzyme Q10 levels correlate with the activities of complexes I and II/III in mitochondria from parkinsonian and nonparkinsonian subjects. Ann Neurol 1997;42:261-264.
[98.] Critchley EMR. Evening primrose oil (Efamol) in parkinsonian and other tremors. In: Clinical Uses of Essential Fatty Acids, Horrobin DF ed. Montreal: Eden Press; 1982.
[99.] Caughey GE. Effect on tumor necrosis factor alpha and interleukin l-beta production of diets enriched in n-3 fatty acids from vegetable oil or fish oil. Am J Clin Nutr 1996;63:116-122.
[100.] Youdim KA, Martin A, Joseph JA. Essential fatty acids and the brain: possible health implications. Intl J Dev Neurosci 2000;18:383-399.
[101.] Snider SR. Octacosanol in Parkinsonism. Ann Neurol 1984;16:723.
[102.] Gotz ME, Gerstner A, Harth R, et al. Altered redox state of platelet coenzyme Q10 in Parkinson's disease. J Neural Transm 2000;107:41-48.
[103.] Shults CW, Beal MF, Fontaine D, et al. Absorption, tolerability, and effects on mitochondrial activity of oral coenzyme Q10 in parkinsonian patients. Neurology 1998;50:793-795.
[104.] Birkmayer GJD, Birkmayer W. Stimulation of endogenous L-dopa biosynthesis - a new principle for the therapy of Parkinson's disease. Acta Neurol Scand Suppl 1989;126:183-187.
[105.] Birkmayer JGD, Vrecko C, Volc D, Birkmayer W. Nicotinamide adenine dinucleotide (NADH) - a new therapeutic approach to Parkinson's disease. Acta Neurol Scand Suppl 1993;146:32-35.
[106.] Kuhn W, Muller T, Winkel R, et al. Parenteral application of NADH in Parkinson's disease: clinical improvement partially due to stimulation of endogenous levodopa biosynthesis. J Neural Transm 1996;103:1187-1193.
[107.] Kidd PM. A review of :nutrients and botanicals in the integrative management of cognitive dysfunction. Altern Med Rev 1999;4:144-161.
[108.] Steffen V, Santiago M, de la Cruz CP, et al. Effect of intraventricular injection of 1-methyl-4-phenylpyridinium: protection by acetyl-L-carnitine. Hum Exp Toxicol 1995;14:865-871.
[109.] Funfgeld EW, Nedwidek P. Neurohomologous phosphatidylserine in Parkinsonian patients with associated disorders of cerebral metabolism. Clin Trials J 1987;24:42-61.
[110.] Laihinen A, Ruottinen H, Rinne JO, et al. Risk for Parkinson's: twin studies for the detection of asymptomatic subjects using (18F)6-fluorodopa PET. J Neurol 2000;247 Suppl. 2:II110-113.
[111.] Brooks DJ. Morphological and functional imaging studies on the diagnosis and progression of Parkinson's disease. J Neurol 2000;247 Suppl. 2:11-18.
[112.] Piccini P, Burn DJ, Ceravalo R, et al. The role of inheritance in sporadic Parkinson's disease: evidence from a longitudinal study of dopaminergic function in twins. Ann Neurol 1999;45:577-582.
[113.] Morrish PK, Rakshi JS, Bailey DL, et al. Measuring the rate of progression and estimating the preclinical period of Parkinson's disease with (18F)dopa-PET J Neurol Neurosurg Psychiatry 1998;64:314-319.
[114.] Riederer P, Sian J, Gerlach M. Is there neuroprotection in Parkinson's syndrome? J Neurol 2000;247 Suppl 4:8-11.
[115.] Green PS, Simpkins JW. Neuroprotective effects of estrogens: potential mechanisms of action. Intl J Dev Neurosci 2000;18:347-358.
[116.] Snyder SH. No NO prevents parkinsonism. Nat Med 1996;2:965-966.
[117.] Lu X, Bing G, Hagg T Naloxone prevents microglia-induced degeneration of dopaminergic substantia nigra neurons in adult rats. Neuroscience 2000;97:285-291.
[118.] Akaneya Y, Takahashi M, Hatanaka H. Interleukin-1 [Beta] enhances survival and interleukin-6 protects against MPP+ neurotoxicity in cultures of fetal rat dopaminergic neurons. Exp Neurol 1995;136:44-52.
[119.] Diederich NJ, Goetz CG. Neuropsychological and behavioral aspects of transplants in Parkinson's disease and Huntington's disease. Brain Cognit 2000;42:294-306.
[120.] Eriksson PS, Perfilieva E, Bjork-Eriksson T, et al. Neurogenesis in the adult human hippocampus. Nat Med 1998;4:1313-1317.
[121.] Nakao N, Yokote H, Nakai K, Itakura T. Promotion of survival and regeneration of nigral dopamine neurons in a rat model of Parkinson's disease after implantation of embryonal carcinoma-derived neurons genetically engineered to produce glial cell line-derived neurotrophic factor. J Neurosurg 2000;92:659-670.
[122.] Often D, Sherki Y, Melamed E, et al. Vasoactive intestinal peptide (VIP) prevents neurotoxicity in neuronal cultures: relevance to neuroprotection in Parkinson's disease. Brain Res 2000;854:257-262.
[123.] NINDS (National Institute of Neurological Diseases and Stroke), USA. Parkinson's Disease: A Research Planning Workshop. Bethesda, MD, USA: Office of Scientific and Health Reports (tel. 301-496-5751), NINDS, National Institutes of Health; 1999.
Parris Kidd, PhD (Cell biology, University of California at Berkeley) -- Contributing Editor, Alternative Medicine Review; Health educator and biomedical consultant to the supplement industry. Correspondence address: 847 Elm St, El Cerrito, CA 94530
COPYRIGHT 2000 Thorne Research Inc.
COPYRIGHT 2001 Gale Group