Ninety patients with atrophic (dry) age-related macular degeneration were randomly assigned to receive, in double-blind fashion, one of three treatments for one year: 1) lutein 10 mg/day (an amount present in approximately 60 g of spinach); 2) lutein plus a supplement containing antioxidants, vitamins, and minerals; or 3) placebo. The supplement provided daily 2,500 IU vitamin A, 15,000 IU natural beta-carotene, 1,500 mg vitamin C, 400 IU vitamin D, 500 IU vitamin E, 50 mg thiamine, 10 mg riboflavin, 70 mg vitamin B3, 50 mg pantothenic acid, 50 mg vitamin B6, 500 mcg vitamin B12, 800 mcg folic acid, 300 mcg biotin, 500 mg calcium, 300 mg magnesium, 75 mcg iodine, 25 mg zinc, 1 mg copper, 2 mg manganese, 200 mcg selenium, 200 mcg chromium, 160 mg bilberry extract (standardized to 25% anthocyanosides), 150 mg alpha-lipoic acid, 200 mg N-acetylcysteine, 100 mg quercetin, 100 mg rutin, 900 mg taurine, and several other nutrients.
The mean macular pigment optical density increased by 0.09 log unit in group 1 (p = 0.1 vs. placebo) and by 0.08 log unit in group 2 (p = 0.02), and decreased by 0.03 log unit in the placebo group. Snellen equivalent visual acuity improved by a mean of 5.4 letters (equivalent to approximately 1 line on the eye chart) in group 1 (p = 0.01 vs. baseline and vs. placebo). In group 2 the mean improvement was 3.5 letters (p = 0.04 vs. baseline; p = 0.08 vs. placebo). Contrast sensitivity improvement significantly in both active-treatment groups; the degree of improvement was greater in the group receiving combination therapy then in those receiving antioxidants alone; no significant improvement was seen in the placebo group. Active treatment was effective at all stages of age-related macular degeneration (stages II, III, & IV).
Comment: These results indicate that supplementation with lutein or lutein together with other nutrients can increase macular pigment optical density and improve visual function in patients with age-related macular degeneration, By some, but not all, measures, combination therapy was more effective than lutein alone.
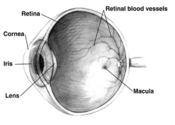
Lutein is a carotenoid found primarily in spinach, corn, other vegetables, and eggs. It is a normal component of the macular pigment, where it filters the retina-damaging blue-light portion of the sun's rays. A thicker macular pigment (increased macular pigment optical density) provides greater protection than a thinner macular pigment, and lutein supplementation has been shown to increase the thickness of the macular pigment. Antioxidants such as selenium, vitamin E, vitamin C, and quercetin may protect retinal tissue against oxidative damage, and nutrients such as zinc, taurine and anthocyanosides appear to have direct effects on ocular tissues (e.g., stabilizing cell membranes or enhancing visual function).
Richer S, et al. Double-masked, placebo-controlled, randomized trial of lutein and antioxidant supplementation in the intervention of atrophic age-related macular degeneration the Veterans LAST study (Lutein Antioxidant Supplementation Trial). Optometry 2004;75(4):1-15.
COPYRIGHT 2005 The Townsend Letter Group
COPYRIGHT 2005 Gale Group