Malaria
Malaria (Italian: "bad air"; formerly called ague or marsh fever in English) is an infectious disease which in humans causes about 350-500 million infections and approximately 1.3 million deaths annually, mainly in the tropics. Sub-Saharan Africa accounts for 85% of these fatalities. more...
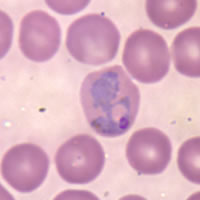
Malaria is caused by the protozoan parasites of the genus Plasmodium (one of the Apicomplexa), and the transmission vector for human malarial parasite is the female Anopheles mosquito. The P. falciparum variety of the parasite accounts for 80% of cases and 90% of deaths. Pregnant women and children under the age of five are most vulnerable to malaria.
For his discovery of the cause of malaria, French army doctor Charles Louis Alphonse Laveran was awarded the Nobel Prize for Physiology or Medicine in 1907. Britain's Sir Ronald Ross also received a Nobel prize (in 1902) for describing the life cycle of the malaria parasite as it develops in the bodies of its mosquito and human hosts.
Symptoms
Symptoms of malaria include fever, shivering, arthralgia (joint pain), vomiting, anemia, and convulsions. There may be the feeling of tingling in the skin, particularly with malaria caused by P. falciparum. Complications of malaria include coma and death if untreated—young children are especially vulnerable. Splenomegaly (enlarged spleen), intense headaches, cerebral ischemia and hemoglobinuria with renal failure may occur.
Mechanism of the disease
Infected female Anopheles mosquitoes carry Plasmodium sporozoites in their salivary glands. If they pierce a person's skin, which they usually do starting at dusk and continuing throughout the night, the sporozoites enter the person's body via the mosquito's saliva, migrate to the liver where they multiply within hepatic liver cells asexually. There they develop into merozoites which then enter red blood cells, where they multiply further, again asexually, periodically breaking out of the exploited red blood cells. The classical description of waves of fever coming every two or three days arises from simultaneous waves of merozoites breaking out of red blood cells during the same day. Development in the hepatic cell takes 6 to 15 days depending on the species. Some of the sporozoites in vivax and ovale malaria do not develop into merozoites immediately, but produce hypnozoites that remain dormant for several months (typically, from 6 to 12, but sometimes up to 3 years). After a period of dormancy, they reactivate and produce merozoites. Hypnozoites are responsible for long incubation and late relapses in these two species of malaria. About a half of the cases of vivax infection in temperate areas start after having overwintered, i.e. during the next year after the mosquito bite. The parasite is relatively protected from attack by the body's immune system because for most of its human life cycle it stays inside liver and blood cells. However, circulating infected blood cells are destroyed in the spleen. To avoid this fate, the parasite produces certain surface proteins which infected blood cells present on their cell surface, causing the blood cells to stick to the walls of blood vessels. These surface proteins known as PfEMP1 are highly variable (there are at least 50 variations) and cannot serve as a reliable target for the immune systeme.
Read more at Wikipedia.org