Khan A, Khan S, Kolts R, Brown WA. Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: analysis of FDA reports. Am J Psychiatry 2003; 160:790-792.
* PRACTICE RECOMMENDATIONS
Depressed adult patients are no more likely to commit suicide while taking selective serotonin reuptake inhibitors (SSRIs) than any other class of antidepressants.
The low suicide rate in the non-SSRI category, which included tricyclic antidepressants (TCAs), reminds us that no evidence exists to consider tricyclics more dangerous than other antidepressants, despite what is commonly believed. Thus, clinicians who avoid prescribing any antidepressant because of risk of suicide may change their clinical practice. It is important to remember that these patients are adults and had mild to moderate depression without any significant comorbid conditions.
* BACKGROUND
Several case reports and experts have speculated that SSRIs carry higher risks of agitation, suicidal ideation, and suicidal impulses. Media coverage and lawsuits involving patients who committed suicide while on antidepressants fueled the debate. Besides SSRIs, TCA and monoamine oxidase inhibitor (MAOI) medications may carry higher risk of suicide because of their toxicity in overdose.
The annual suicide rates for patients with major affective disorders is estimated to be 0.30% to 0.80%. (1) Psychiatric illness--including major depression and bipolar disorder, chronic illness, alcohol abuse, and other factors--are associated with increased risk of suicide. This study attempted to determine whether SSRIs are dangerous in and of themselves.
* POPULATION STUDIED
The study analyzed a US Food and Drug Administration (FDA) database to obtain suicide rates for 48,277 outpatients enrolled in controlled trials of antidepressants. The authors stated that antidepressant clinical trial participants tend to be mildly to moderately depressed and that studies tend to enroll patients who are not suicidal; do not have other psychiatric illnesses, and do not have known substance abuse problems.
* STUDY DESIGN AND VALIDITY
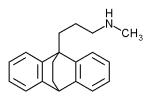
This retrospective cohort study used FDA clinical trial data from 1985 to 2000 for 4 SSRIs (fluoxetine, sertraline, paroxetine, and citalopram) and 5 other antidepressants (venlafaxine, nefazodone, mirtazapine, sustained-release buproprion, and extended-release venlafaxine). Any suicides reported in the database were assigned to the antidepressant the patient was taking at the time they committed suicide.
Many of the patients were talking an active control medication; therefore, data were obtained for another SSRI (fluvoxamine), 4 TCAs (imipramine, amitriptyline, mianserin, and dothiepin), and 2 other antidepressants (trazodone and maprotiline). The length of time patients were followed in the studies was between 4 and 8 weeks. (1)
The study was adequately powered to detect a difference between the SSRI and non-SSRI antidepressant groups. Whether the population studied represents patients primary care physicians are likely to see in the office is unclear. The study did not summarize patient characteristics, report whether they were enrolled from specialty clinics, or assess the validity of the underlying individual studies.
* OUTCOMES MEASURED
The study compared rates of completed suicide for the subjects taking SSRIs compared with the subjects taking non-SSRI antidepressants and placebo. Data were not available to assess whether suicidal ideation or attempts were different between the 2 groups.
* RESULTS
The FDA database contained information for 48,277 patients enrolled in antidepressant trials. Of these, 26,109 were randomly assigned to SSRIs, 17,273 were assigned to non-SSRI antidepressants, and 4895 were given placebo. No statistically significant differences in rates of completed suicide were found between SSRIs, non-SSRIs, and placebo. Seventy-seven (0.15%) subjects committed suicide (0.15% of the SSRI group, 0.20% in the non-SSRI category, and 0.10% in the placebo group).
Similarly, analyzing the results by patient exposure years did not show a significant difference (0.59%, 0.76%, and 0.45% for SSRIs, non-SSRIs, and placebo, respectively). The method of suicide was given for ball of the suicides, but no clear differences in type of suicide or impulsivity could be drawn.
REFERENCES
(1.) Khan A. Symptom reduction and suicide risk in patients treated with placebo in antidepressant clinical trials: an analysis of the Food and Drug Administration database. Arch Gen Psychiatry 2000; 57:311-317.
Peter Ham, MD, University of Virginia Family Medicine, Charlottesville. E-mail: ph2t@virginia.edu.
COPYRIGHT 2003 Dowden Health Media, Inc.
COPYRIGHT 2003 Gale Group