The Tower of Hanoi (TOH) is a well-established test of executive functions, processes which have been proposed as central to the cognitive deficits of ADHD (Barkley, 1997; Pennington & Ozonoff, 1996; Sergeant, Geurts, & Oosterlaan, 2002). We utilized the TOH to pursue recent research findings suggesting that the major subtypes of ADHD may differ in the degree of their executive deficits. We also sought to explore any differences between the major subtypes of ADHD in cognitive response to stimulant treatment. Specifically, we investigated differences in private speech and performance on TOH by control children and patients with the Inattentive and Combined subtypes of ADHD. We also evaluated the impact of stimulant treatment on measures obtained in TOH.
Private Speech
Barkley (1997) postulated four executive functions (nonverbal working memory, verbal working memory, self-regulation of affect, and reconstitution), which are controlled by behavioral inhibition. Barkley described verbal working memory as representing the internalization of speech, which promotes description, reflection, self-questioning, generation of rules and plans, and development of meta-rules. Verbal working memory, as defined by Barkley, is implicated in TOH because the task elicits private speech in children. Working memory, including verbal working memory, is a necessary element in planning, that is, purposive strategic effort toward meeting a goal. Admittedly, other models of executive dysfunction in ADHD, in contrast to Barkley's (1997), do not accord an overarching role to inhibition and may not equate private speech with verbal working memory (e.g. Douglas, 1999). However, our approach was to use Barkley's theory as a guide for the interpretation of children's behavior in the TOH.
Private speech is externalized thought that is addressed to the self rather than to a particular listener (Berk & Potts, 1991). Vygotsky (1934/1962) regarded private speech as having a critical role in self-regulation, including planning and monitoring one's actions. Further, Vygotsky outlined a developmental progression beginning with externalized utterances that structurally and functionally resemble social speech, followed by verbalizations with self-regulatory function, and ending with internal verbalizations in the form of silent thoughts.
Evidence supporting Vygotsky's assumption that private speech is implicated in self-regulation includes a link between private speech and task difficulty. Berk and Garvin (1984) reported that difficult academic tasks increased elementary school children's private verbalizations involving descriptions of their own activity and self-guidance as well as inaudible mutterings. Although similar findings have been obtained in other investigations, there is mixed evidence on the association between number of verbalizations and task performance (Beaudichon, 1973; Berk, 1986; Frauenglass & Diaz, 1985; Goodman, 1981; Klein, 1964; Kohlberg, Yaeger, & Hjertholm, 1968; Murray, 1979; Zivin, 1972). Therefore, Berk (1986) proposed that the regulatory function of self-directed speech may not have an impact upon concurrent, but on future task performance. Indeed, some investigations (e.g., Bivens & Berk, 1990) have found a positive correlation between speech and future task success.
Also in agreement with Vygotsky, self-stimulating, task-irrelevant, and task-relevant externalized private verbalizations of children diminish with age whereas task-relevant external manifestations of inner speech (i.e., inaudible muttering and lip and tongue movement) increase with development (Bivens & Berk, 1990; Frauenglass & Diaz, 1985).
Children with ADHD engage in more private speech than do controls during task transitions, academic activities, and free-play activity (Campbell, 1973; Copeland, 1979; Winsler, 1998; Zentall, Gohs, & Culatta, 1983). Copeland (1979) also reported that the private speech of ADHD children more often included developmentally less mature forms (e.g., exclamations and descriptions of environment) as opposed to more advanced forms of speech (e.g., planning). Analogously, Berk and Potts (1991) and Winsler (1998) found that, in comparison to controls, youngsters with ADHD engaged in more externalized task-relevant speech (level II) and less relatively internalized task-relevant private speech (level III). However, children with ADHD did not exhibit more externalized task-irrelevant speech (level I) than did controls. Interestingly, Berk and Potts (1991) reported that over ages 6-9, children with ADHD, compared with control participants, displayed the same developmental trends for private speech at levels I-III but with a noticeable delay in the transition toward internalization.
The single study that examined the effects of stimulant medication on private speech in children with ADHD evaluated a small sample of patients on and off their clinical doses of methylphenidate. Under the stimulant, these youngsters exhibited less level II and more level III private speech but did not reduce their level I verbalizations (Berk & Potts, 1991). These findings suggest that methylphenidate enhances internalization of private speech in participants with ADHD, but this interpretation would be strengthened by a replication under blind drug administration, as accomplished in the present work.
Tower of Hanoi
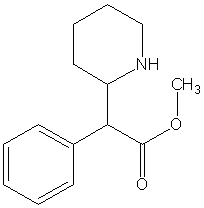
The TOH (Simon, 1975) and its variant the Tower of London (TOL) require participants to transform an arrangement of disks into a different configuration in the minimum number of moves possible. In the two illustrative TOH puzzles presented in Fig. 1, the start state is the arrangement of disks of different sizes that a participant must modify by moving one disk at a time in the minimum number of steps so as to reach the end state configuration. TOH has been described as a measure of planning (Borys, Spitz, & Dorans, 1982; Spitz, Minsky, & Bessellieu, 1985). Consistent with that position, patients with prefrontal lesions have impaired performance on TOH and TOL (Goel & Grafman, 1995; Owen, Downes, Sahakian, Polkey, & Robbins, 1990; Shallice, 1982).
The TOH is conventionally administered so that the puzzles require an increasing number of moves for a solution, and the task is scored as the number of puzzles solved or the highest level (number of steps to solution) reached. However, Spitz (Spitz, Webster, & Borys, 1982; Spitz, Minsky, & Bessellieu, 1984; Spitz et al., 1985) proposed that a more sensitive index of task mastery is subgoal length, which reflects depth of search (DOS), that is, the capacity to mentally search ahead by several moves. As illustrated in Fig. 1, DOS is defined as the number of moves needed to complete the subgoal of transferring the largest disk to its end position in a minimum sequence of steps before the complete puzzle solution is achieved.
[FIGURE 1 OMITTED]
In addition to verbal working memory, TOH involves nonverbal working memory, another of the executive functions postulated by Barkley (1997). Nonverbal (spatial) working memory is required by the task because sequences of moves must be held in mind to achieve correct solutions. In accord with the views that patients with ADHD are impaired on the executive functions measured by TOH, many studies have found that children with ADHD have deficient performance on TOH (Aman, Roberts, & Pennington, 1998; Klorman et al., 1999; Pennington, Groisser, & Welsh, 1993; Weyandt & Willis, 1994; but see Ozonoff & Jensen, 1999). In contrast, the limited research on the impact of stimulants on TOH consists of a single open-label study documenting improved TOH performance for ADHD boys tested in a fixed order (Aman et al., 1998). Thus, the present study was aimed at addressing limitations in present understanding of the impact of stimulants on TOH.
Subtypes of ADHD
Children with Predominantly Hyperactive-Impulsive and Combined Types of ADHD are more aggressive, impulsive, and unpopular than their peers with Predominantly Inattentive Type of ADHD (Barkley, DuPaul, & McMurray, 1990; Carlson & Mann, 2000). There is mixed evidence on differences in cognitive deficits between children with ADHD who differ on hyperactivity, particularly for Wechsler IQ tests and for the Continuous Performance Test (Ackerman, Anhalt, Dykman, & Holcomb, 1986; Barkley et al., 1990; Faraone, Biederman, Weber, & Russell, 1998; Lahey & Carlson, 1991; Paternite, Loney, & Roberts, 1996). In contrast, more clearcut differences between ADHD subtypes have often emerged on measures of executive functions. Specifically, children with the Combined subtype of ADHD, in comparison with those with the Inattentive subtype, were more impaired on tests of planning like TOH/TOL (Klorman et al., 1999; Nigg, Blaskey, Huang-Pollock, & Rappley, 2002); motor inhibition, as measured by the Stop task (Nigg et al., 2002); and, less consistently, set shifting, generally measured by the Wisconsin Card Sorting Test (Barkley, Grodzinsky, & DuPaul, 1992; Houghton et al., 1999; Klorman et al., 1999; Nigg et al., 2002). However, in contrast to these reports, Chhabildas, Pennington, and Willcutt (2001) found that symptoms of inattention, rather than those of hyperactivity/impulsivity, were closely associated with deficits of inhibition, vigilance, and processing speed. Considering the weight of this evidence, Barkley et al. (1990) proposed that the two ADHD subtypes represent two different disorders.
There is limited evidence of differences between ADHD subtypes in the impact of stimulant therapy (McBurnett, 2000). Barkley, DuPaul, and McMurray (1991) reported that children with the Combined and Inattentive types of ADHD benefited comparably from methylphenidate treatment with respect to ratings of behavior at home and school as well as performance on Continuous Performance and math tests. However, a global review of all outcome measures by the investigators disclosed that patients with the Inattentive type displayed better clinical responses to low doses of methylphenidate whereas those with the Combined type tended to exhibit optimal responses to higher dosages. These intriguing results prompt further examination of differences between ADHD subtypes in response to stimulant administration, particularly in view of the dearth of research on this topic. In pursuing this aim, we were able to expand on Barkley et al.'s (1991) procedure for defining subtypes of ADHD by using, not only teacher ratings, but also parent interviews.
The Present Study
In the present study, we administered TOH under two levels of depth of search in order to more directly manipulate spatial working memory load. Children with ADHD were tested without any medication as well as under methylphenidate and placebo; comparison children were tested without medication on three occasions. If increasing depth of search lowered TOH performance to a greater extent among patients with ADHD than for control children, this finding would suggest that spatial working memory may account for the performance deficits of participants with ADHD on TOH. Similarly, if the effects of depth of search on ADHD children were attenuated by methylphenidate in comparison with placebo, this result would imply that the stimulant improves performance on TOH by its impact on spatial working memory and planning. By analogous reasoning, if children with ADHD engaged in more private speech than controls and methylphenidate reduced these children's self speech, these findings would implicate verbal working memory in these effects. These potential interpretations were based on our assumptions that DOS measures spatial working memory (Klorman, unpublished data) and private speech reflects verbal working memory (Barkley, 1997).
We hypothesized that we would replicate our finding of relatively worse performance deficits on TOH by children with the Combined subtype of ADHD than patients with the Inattentive subtype (Klorman et al., 1999), particularly for problems with greater depth of search requirements. We also predicted that methylphenidate would improve task performance and reduce rule breaks, especially for TOH problems requiring greater depth of search. We hypothesized that children with ADHD would make more private utterances than controls, particularly for long DOS puzzles, and that these differences would be attenuated by methylphenidate. We did not have hypotheses concerning differences between subtypes of ADHD with respect to private speech.
METHOD
Participants
Participants were 41 children with ADHD and 34 control children. Participants received compensation of $6 for each hour of participation. Children with ADHD were referred by local professionals and were diagnosed based on a combination of (a) the Parent Interview for Child Symptoms--4 (P. I. C. S.--4; Schachar, Ickowicz, & Wachsmuth, 1995, unpublished), a semistructured interview schedule administered by the third author. The choice of a semistructured over a structured interview was made because this format allowed the use of clinical judgment in eliciting and evaluating information provided by parents, although admittedly diagnostic bias despite the interviewer's best efforts cannot be eliminated. It was not practical to obtain reliability estimates for these diagnostic interviews but similar interviews have yielded high inter-judge reliability in previous research (Kaufman et al., 1998); and (b) the Teacher ADHD Scale (DuPaul, 1991), a questionnaire presenting the nine symptoms for inattention and hyperactivity/impulsivity, respectively, in a Likert scale. For a diagnosis of ADHD we required the child's parent to endorse the requisite number of DSM-IV symptoms for ADHD Combined Type or ADHD predominantly Inattentive Type, respectively, on the F.I.C.S.--4 and for teachers to endorse at least four symptoms of inattention and/or hyperactivity/impulsivity. Following the procedures of the MTA study (1999), we supplemented the count of inattention or hyperactivity/impulsivity symptoms endorsed by a parent by up to two ADHD symptoms for each cluster from the Teacher ADHD scale.
Four of the ADHD patients had undergone previous trials of stimulant therapy ranging from 2 weeks to 7 months. Families and patients were advised in informed consent procedures that cognitive tests including TOH would be administered in each phase of the trial in order to supplement the diagnostic evaluation and the outcome of a stimulant trial described below.
Controls were recruited from a local school district and did not receive a diagnosis of (1) any disruptive disorder on the P. I. C. S.--4, or (2) learning disorder, as assessed by the Woodcock-Johnson Test of Achievement-Revised (1989) and the Kaufman Test of Academic Spelling (Kaufman & Kaufman, 1985). Families of controls and their children were informed that we were interested in studying children without behavioral difficulties.
Children in both samples met these additional criteria: (1) ages 6-12; (2) Wechsler Intelligence Scale for Children III (Wechsler, 1991) Full Scale IQ > 80; (3) no history of neurologic disorder, chronic medical illness, Bipolar Disorder, Schizophrenia, or Pervasive Developmental Disorder; (4) no episode of Major Depressive Disorder in at least 6 months; (5) normal or corrected vision and hearing; (6) no current use of medication; and (7) no physical disabilities.
As shown in Table I, approximately half of the children referred to the ADHD sample were girls. This unusually high proportion of girls reflects increasing sensitivity by clinicians to the identification of girls with ADHD as well as the awareness of our referring sources that we were studying sex differences in ADHD.
As shown in Table I, the three diagnostic groups were comparable in gender composition, [chi square](df = 2, N = 75) = 2.04, ns; race makeup, [chi square](df = 2, N = 75) < 1, ns; age, F(2, 69) < 1, ns; and Hollingshead socioeconomic status, F(2, 69) < 1, ns. However, Full Scale IQ differed among samples, F(2, 69) = 11.20, p < .001; controls scored higher than children with ADHD with both the Combined (p < .001) and Inattentive types (p < .01). The two ADHD samples did not differ from each other on Full Scale IQ, F(1, 69) < 1, ns.
Table I shows that, as expected, children with ADHD, in comparison with controls, had a higher frequency of P. I. C. S.--4 psychiatric diagnoses besides ADHD, particularly so for externalizing disorders, [chi square](df = 2, N = 75) = 29.78, p < .001. Comparisons of samples indicated that children with the Combined subtype of ADHD were more likely to receive diagnoses of Oppositional Defiant Disorder or Conduct Disorder than were their Inattentive counterparts (p < .01), who, in turn, exceeded control participants in this respect (p < .01).
Medication Trial for Children with ADHD
Participants with ADHD took part in a randomly ordered, double-blind clinical drug trial comprised of 21 consecutive days of methylphenidate and 21 consecutive days of placebo. Methylphenidate was titrated in divided dosages according to the following schedule: 0.25 mg/kg b.i.d. (breakfast and lunch) on Days 1-2; 0.25 mg/kg b.i.d. plus 0.125 mg/kg at 4 pm on Days 3-7; 0.3 mg/kg b.i.d. and 0.15 mg/kg at 4 pm on Day 8-14; and 0.4 mg/kg b.i.d. and 0.2 mg/kg at 4 pm on Days 15-21. All dosages were administered to the nearest 2.5 mg. The minimum and maximum dosages of methylphenidate were 25 and 50 mg/day, respectively. Placebo capsules, which were identical in appearance and taste to those containing methylphenidate, were administered on the same schedule as the active medication. One obese child was assigned a lower dosage (.75 mg/kg/day) than he would have received based on his weight. When parents reported serious side effects (n = 5), their children's dosages were reduced or planned increments were OMITTED. When these unavoidable departures from the original dosage schedule were made, neither the investigators nor the parents were informed of the nature of the substance administered in the affected phase until the end of the study. It would have been unethical to maintain patients on an excessive dosage, and dosage adjustments are consistent with clinical practice. On the other hand, eliminating participants who could not tolerate their assigned dosage might potentially skew the sample. Notably, all these reductions were made in the methylphenidate phase. The mean [+ or -] SE of the final daily dose of methylphenidate was 33.12 [+ or -] 1.36 mg = 0.94 [+ or -] 0.02 mg/kg.
Testing for patients with ADHD took place in three sessions held at noon: a no-medication Baseline session, and the 21st day of the methylphenidate and placebo phases, respectively. Control children were tested without medication on three occasions spaced at intervals approximating those for the sessions of participants with ADHD. After ingestion of the appropriate capsule (or onset of the session for control participants), approximately 2 h elapsed during which EEG was recorded, and the child participated in procedures that will be subject of a separate paper. Subsequently, the TOH was administered, and this task took up approximately 30 min.
Task
As illustrated in Fig. 1, the TOH task was administered by means of two boards, each of which contained three (or four) graduated disks arranged on three pegs. The examiner's board displayed the goal arrangement (end state), and the child's board, showed the start state. The participant was asked to rearrange the display on his/her board in as few moves as possible so that it looked exactly like the examiner's board. The number of minimum moves possible for the puzzle was announced at the start of each trial. The examiner stated three rules for the test and subsequently asked the child to repeat them in his/her own words: (1) The child was permitted to move only one disk at a time; (2) The child was not allowed to place a larger disk on a smaller disk; and (3) At all times, a disk was to be either in the child's hand or on a peg.
There were three matched forms of TOH problems, corresponding to each session, and assigned to sessions according to a Latin Square arrangement. Each form consisted of one short and one long DOS set, which were administered in a counterbalanced order across participants. The two DOS sets were balanced for the minimum number of steps to solution and were presented in order of increasing solution length (3, 4, 5, and 6 moves [three-disk problems] and 7, 8, 9, and 10 moves [four-disk problems]). As noted by Spitz et al. (1982), each puzzle was easily solved after completing the subgoal of moving the largest disk to its end position in the minimum number of steps (See Fig. 1). DOS was defined as the minimum number of moves to accomplish this subgoal. Following Spitz et al. (1984), the short DOS set required 0-7 moves to the first subgoal whereas the matched long DOS set required one additional move to the first subgoal (i.e., 1-8 moves, respectively). As noted earlier, puzzles on the two DOS sets were matched pairwise on the total number of steps required for solving the puzzle.
At each session, the test started with a review of the rules and two practice problems involving two moves to solution. Next, each puzzle on the two DOS sets was administered up to three times, beginning with the four-move problem. If the child passed two out of three trials of the four-move problem, he/she received credit for the three-move problem and progressed to the five-move problem Otherwise, a three-step problem was administered before continuing. For all puzzles, a trial was terminated and scored as failed when the number of moves exceeded the minimum number of moves to solution or when a rule violation occurred. In addition, when a minimum solution path was not attained, the participant was informed that he/she had made too many moves. If the minimum path solution for a given problem was reached in the first two trials, the third trial was OMITTED and credited as correct. For each DOS set, testing stopped when the child failed all three trials for two consecutive problems. The TOH test ended when both sets of DOS problems were administered.
For each puzzle, planning time (latency from the examiner's signal to start to the first move by the child) was measured to the nearest second by means of a digital stopwatch.
Scoring
Performance was scored as the number of correctly solved puzzles for each DOS set. We also counted the number of rule breaks and mean latency for the first move, separately for passed and failed puzzles within each DOS set.
The verbalizations made by participants while solving the TOH puzzles were classified into separate speech units, defined as a phrase or sentence (a) characterized by natural phrasing and representing a thought, and/or (b) followed by pauses [greater than or equal to]4 s. Only audible, spontaneous verbalizations were rated.
Each speech unit was categorized as either self-regulatory or not self-regulatory. Following Meichenbaum and Biemiller (1990), we considered four categories of self-regulatory utterances: defining, planning, monitoring, and evaluating. Defining included those utterances reflecting a subject's attempt to label the task, procedures, or objects (e.g., "This is a disk."). Planning subsumed statements or questions about procedures or steps that would be carried out, such as figuring out an idea before an action was carried out (e.g., "I'm going to move this here."). Monitoring comprised a child's noticing, checking, or commenting on his/her own performance (e.g., "I need to slow down."). Evaluating incorporated statements or inquiries about the correctness of previous actions (e.g., "I messed up."). All verbalizations that did not belong to these four categories were classified not self-regulatory (e.g. "I went to my grandmother's house before I came here."). However, participants' responses to the examiner's questions, incomprehensible utterances, humming, repetitive motor play, sighs, and lip movements were not scored. The present task was more structured and involved briefer trials than those used in many previous studies, and these factors may have militated against whispering, mumbling, or lip movements.
Judges blind to drug condition and diagnosis classified children's units of speech from audio (n = 6) or videotapes (n = 69) as regulatory or not self-regulatory. For statistical analyses, we totaled the number of self-regulatory and not self-regulatory verbalizations, separately for levels of DOS and sessions.
The first 20 records were scored by one judge and the remainder by a second judge. Reliability of total scores for each record was assessed by comparing ratings by a reliability judge for 16 randomly selected tapes scored by the first judge and 13 randomly selected records evaluated by the second judge. The resulting intraclass correlations were .98 and .97, respectively.
RESULTS
Potential Confounding Factors
All analyses of variance reported below were repeated with gender as a factor, but none of the findings that we report were qualified by gender. Similarly, separate analyses of ADHD subtypes considering presence or absence of comorbidity with Oppositional Defiant Disorder or Conduct Disorder did not reveal interactions of subtypes of ADHD with these comorbid conditions. Therefore, we will not refer further to either gender or comorbidity with externalizing disorders.
In principle, group differences regarding performance on TOH might reflect the lower IQ scores of children with ADHD. However, Barkley (1997, p. 298) has argued vigorously against statistical adjustment for IQ in comparing ADHD and control samples because these procedures may remove differences that are due to the effects of ADHD on executive functions. Nevertheless, we evaluated whether statistical adjustment for IQ was likely to affect the results. Specifically, we computed the correlation between WISC III IQ scores and number of TOH solutions, separately for the six Session X DOS combinations. The average r derived from r to z transformations was .06, ns, for control children (df = 32) and .13, ns, for ADHD children (df = 39). These nonsignificant correlations indicated that a covariance adjustment would have minimal effect and, therefore, was not indicated on statistical as well as on theoretical grounds.
We also examined the possibility that any diagnostic differences in number of private speech units might be influenced by the ADHD sample's interior IQ scores. We computed correlations between IQ scores and number of private utterances in the Baseline session, separately for self-regulatory and non-self regulatory speech on passed and failed puzzles. The mean resulting correlations, based on r-z transformations, were .02 (df = 32) for controls, ns, and .13 (df = 37), ns, for children with ADHD. Once again, in addition to theoretical arguments against statistical adjustment for IQ in ADHD samples, these results indicate that a covariance adjustment would have negligible effects.
Analyses of Number of Correct Solutions
For this and other analyses, control participants were assigned to pseudo drug orders, such that the resulting subsamples were matched as closely as possible in mean age and gender composition to children with ADHD who received methylphenidate first or second, respectively.
The design for the analysis of variance involved two between-participant factors: diagnosis (controls, ADHD Inattentive, ADHD Combined) and drug order. The following within-participants factors were considered: DOS and session (Baseline, placebo, and methylphenidate). Planned comparisons evaluated contrasts between diagnostic groups. In addition, the effect of the pharmacological intervention was assessed by comparing the methylphenidate and placebo sessions in a separate analysis of the ADHD samples. Finally, the impact of change from the Baseline session was evaluated by contrasting results for the Baseline session with the average of the methylphenidate and placebo tests. Probabilities for tests of repeated measures reflect adjustments based on the Greenhouse-Geisser solution. Effect sizes are reported as partial omega squared ([[omega].sub.p.sup.2]).
Averaging over conditions and sessions, there were differences in performance among groups, Diagnosis F(2,69) = 9.55, p < .0001, [[omega].sub.p.sup.2] = .04. The control group (M [+ or -] SE = 18.10 [+ or -] 0.42) achieved marginally more solutions than the Inattentive sample (M [+ or -] SE = 15.95 [+ or -] 0.55), F(1,69) = 3.44, p < .10, [[omega].sub.p.sup.2] = .01, and also excelled over the Combined group (M [+ or -] SE = 13.47 [+ or -] 0.54), F(1,69) = 19.05, p < .001, [[omega].sub.p.sup.2] = .04. In turn, the Inattentive sample exceeded the Combined cohort in number of correctly solved puzzles, F(1,69) = 4.49, p < .04, [[omega].sub.p.sup.2] = .01. As expected, long DOS (M [+ or -] SE = 14.48 [+ or -] 0.44) resulted in fewer solutions than did short DOS (M [+ or -] SE = 17.92 [+ or -] 0.37), F(1,69) = 98.79, p < .001, [[omega].sub.p.sup.2] = .18, but diagnostic groups did not differ in this respect, Diagnosis X DOS F(2,69) < 1.
The analysis also disclosed significant improvement with repeated testing irrespective of drug conditions. Sessions X Drug order F(2, 138) = 129.61, p < .001, [[omega].sub.p.sup.2] = .36. Similarly, a separate analysis of the results of controls also revealed significant improvement over successive sessions, F(2, 64) = 45.66, p < .0001, [[omega].sub.p.sup.2] = .30. Therefore, we limited the analysis of drug effects to the Baseline and immediately ensuing session such that, depending on drug order, children with ADHD were evaluated under either placebo or methylphenidate. This strategy provided a less powerful test of drug effects but minimized the impact of practice effects while taking account of initial individual differences in competence in the task. Despite the low power available for this analysis, the crucial interaction of Sessions X Drug approached significance, F(1, 37) = 3.83, p < .06, [[omega].sub.p.sup.2] = .02. As illustrated in Table II, separate post hoc analyses for each subtype disclosed that gains over Baseline results under methylphenidate versus placebo were significant for patients with the Inattentive subtype, F(1, 17) = 6.36, p < .03, [[omega].sub.p.sup.2] = .07, but not for their Combined counterparts, F(1, 20) < 1, [[omega].sub.p.sup.2] = .00.
Rule Breaks
Rule breaks were quite infrequent and displayed heterogeneity of variance and a correlation between cell means and variances. One approach to deal with this difficulty involved an analysis of variance based on a square root transformation; in a second strategy, we performed chi-squared tests after dichotomizing rule breaks for each condition (0 or [greater than or equal to] 1 rule break). The results of these two analyses were entirely consistent with each other and with the analysis of variance of the original scores, so we report the latter results. As shown in Table III, averaging over sessions and conditions, diagnostic groups differed in the frequency of rule breaks, F(2, 69) = 11.65, p < .001, [[omega].sub.p.sup.2] = .05. Specifically, controls violated rules less often than Inattentive patients, F(1, 69) = 4.17, p < .02, [[omega].sub.p.sup.2] = .01, who, in turn, broke rules less frequently than children with the Combined subtype of ADHD, F(1, 69) = 5.50, p < .03, [[omega].sub.p.sup.2] = .01. In contrast to our expectation, rule breaks were not significantly increased by DOS, F(1, 69) = 1.93, ns.
As also illustrated in Table III, irrespective of subtype, children with ADHD made fewer rule breaks under methylphenidate than placebo, F(1, 37) = 8.67, p < .01, [[omega].sub.p.sup.2] = .03; Drug X Subtypes F(1, 37) < 1.
Another pattern depicted in Table III is a pronounced reduction in rule breaks from the Baseline to subsequent sessions (mean of placebo and methylphenidate tests), F(1, 69) = 48.47, p < .0001, [[omega].sub.p.sup.2] = .10, and this progression differed across groups, Groups X Baseline versus later sessions F(2, 69) = 6.62, p < .005, [[omega].sub.p.sup.2] = .02. Simple effects analyses disclosed that the drop in rule violations after the Baseline session was less pronounced for controls than children with either the Inattentive, F(1, 69) = 3.66, p < .06, [[omega].sub.p.sup.2] = .01, or Combined subtype of ADHD, F(1, 69) = 12.86, p < .001, [[omega].sub.p.sup.2] = .03. This finding resulted from a floor effect due to the low rate of rule breaks among comparison children in the Baseline session.
Latency of Responses
After the Baseline session, several participants, particularly in the control sample, did not fail any puzzles in one or more DOS sets, so that we could not score latency for failed trials. To address this issue, we performed two partial analyses. In the Baseline session, for which all but one child had complete data, the only finding was that reaction times were slower for failed than for solved problems (M [+ or -] SE = 5.84 [+ or -] 0.37 vs. 4.12 [+ or -] 0.19 s), F(1, 68) = 21.70, p < .001, [[omega].sub.p.sup.2] = .07. A second analysis was limited to correctly solved puzzles, for which only three children had missing data. These analyses disclosed slower reactions to solved puzzles in the long than in the short DOS condition (M [+ or -] SE = 4.29 [+ or -] 0.18 vs. 3.59 [+ or -] 0.13 s), F(1, 66) = 10.18, p < .005, [[omega].sub.p.sup.2] = .02. No findings involving diagnostic groups or pharmacological conditions were obtained.
Private Speech
Design of Statistical Analyses
Because of the already noted missing data for failed puzzles, results for private speech were analyzed in two stages. Comparisons of controls and the two ADHD samples were limited to the Baseline session, for which only three participants lacked complete data. In turn, evaluation of the pharmacologic intervention was based exclusively on results of children with ADHD, four of whom did not have complete data. Initially, we used analyses of covariance adjusting for number of trials administered, which was related to the number of private verbalizations. However, similar results emerged without this adjustment, so we report the findings of the analyses of variance based on unadjusted number of private speech units while omitting mention of the single interaction that was not found in the analysis of covariance.
Baseline Session
The analysis of the Baseline session considered two between-participants effects (diagnosis and drug order) and the following repeated measures: self-regulatory/not self-regulatory speech, DOS, and failure/success on puzzles. Averaging results over groups and conditions, there was a higher frequency of self-regulatory than not self-regulatory speech units (M [+ or -] SE = 6.95 [+ or -] 0.55 vs. 4.14 [+ or -] 0.38), F(1, 66) = 25.79, p < .0001, [[omega].sub.p.sup.2] = .04. In addition, as shown in Table IV, children spoke more often when failing than when passing a puzzles, F(1, 66) = 84.08, p < .0001, [[omega].sub.p.sup.2] = .13.
There was no difference in the frequency of private speech on long versus short DOS puzzles, F(1, 66) = 1.95, ns. Self-regulation, DOS, and failure/success were complexly related, F(1, 66) = 4.85, p < .05, [[omega].sub.p.sup.2] = .01. Simple effects analyses indicated that self-regulatory speech reflected an interaction of DOS X Failure/success F(1, 66) = 5.48, p < .05, [[omega].sub.p.sup.2] = .02. Specifically, for self-regulatory speech the effect of failure/success was more pronounced for long DOS puzzles (M [+ or -] SE = 10.53 [+ or -] 1.26 vs. 2.67 [+ or -] 0.51, respectively) than for short DOS problems (M [+ or -] SE = 9.74 [+ or -] 1.34 vs. 4.86 [+ or -] 0.82, respectively). In contrast, not self-regulatory speech units were increased by failure versus success, independent of DOS (M [+ or -] SE = 6.48 [+ or -] 0.65 vs. 1.81 [+ or -] 0.27, respectively), F(1, 66) = 47.14, p < .001, [[omega].sub.p.sup.2] = .14.
As depicted in Table IV, differences among diagnostic groups in the Baseline session emerged in the increment of verbalizations when failing a puzzle, Diagnosis X Failure/success F(2, 66) = 6.06, p < .005, [[omega].sub.p.sup.2] = .02. Specifically, the control sample displayed a smaller increase in private speech under failure than did children with either the Inattentive, F(1, 66) = 6.86, p < .02, [[omega].sub.p.sup.2] = .01, or Combined subtype of ADHD, F(1, 66) = 9.63, p < .005, [[omega].sub.p.sup.2] = .02. Subtypes of ADHD did not differ in this respect, F(1, 66) < 1, ns.
Results for ADHD Children
The analysis of ADHD children considered the same factors as those used for the Baseline results with the addition of sessions (Baseline, placebo, methylphenidate) as a repeated measure. Planned orthogonal contrasts evaluated the effect of methylphenidate versus placebo and the difference between the Baseline and the mean of the placebo and methylphenidate sessions.
[FIGURE 2 OMITTED]
Figure 2 presents the findings for the analysis restricted to children with ADHD. Two major patterns were present in the results. First, children with ADHD made more verbalizations on the Baseline session than on later appointments, F(1, 27) = 8.93, p < .01, [[omega].sub.p.sup.2] = .01. Second, methylphenidate reduced the frequency of private speech, F(1, 27) = 10.20, p < .005, [[omega].sub.p.sup.2] = .01. However, the effect of medication involved an interaction of Methylphenidate/placebo X Subtype X Not/Self-regulatory speech X Failure/success F(1, 27) = 10.40, p < .005, [[omega].sub.p.sup.2] = .01. A separate analysis of variance of not self-regulatory speech disclosed an interaction of Methylphenidate/placebo X Failure/success F(1, 27) = 4.63, p < .05, [[omega].sub.p.sup.2] = .01, reflecting a reduction by stimulant medication of the increase in verbalizations during failure; this effect was comparable for the two ADHD subtypes. Methylphenidate/placebo X Failure/success X Subtype F(1, 27) < 1, ns. In contrast, for self-regulatory speech, there was an interaction of Subtypes X Methylphenidate/placebo X Failure/success F(1, 27) = 8.45, p < .01, [[omega].sub.p.sup.2] = .02. As depicted in Fig. 2, for children with the Inattentive subtype of ADHD, the effect of failure on the frequency of self-regulatory utterances was comparably small for the placebo and methylphenidate sessions, Methylphenidate/placebo X Failure/success F(1, 12) = 2.67, ns, [[omega].sub.p.sup.2] = .02. In contrast, for the ADHD Combined sample, methylphenidate decreased self-regulatory verbalizations under failure in comparison to placebo, Methylphenidate/placebo X Failure/success F(1, 15) = 6.63, p < .03, [[omega].sub.p.sup.2] = .04.
DISCUSSION
We employed the TOH to probe into differences in executive deficits by children with the two major subtypes of ADHD and the amelioration of these deficits by stimulant medication. Specifically, we used the TOH task to examine two aspects of working memory emphasized by Barkley's theory (1997): TOH performance, presumed to reflect spatial working memory, and private speech, assumed to index verbal working memory. The novel features of our design included: (1) enhanced diagnostic procedures for ADHD subtypes: (2) experimental manipulation of spatial working memory load in TOH through DOS; (3) comparison of private speech in subtypes of ADHD: and (4) use of a double-blind trial of methylphenidate.
TOH Performance
Patients with the Inattentive subtype of ADHD achieved more correct solutions on the TOH than did youngsters with the ADHD Combined subtype--a result that is consistent with past findings for TOH/TOL and other measures of executive function. Notably, in our previous study, ADHD children with the Inattentive subtype were comparable to controls and excelled over youngsters with the Combined type (Klorman et al., 1999) whereas the present ADHD Inattentive cohort was marginally inferior to controls but still superior to ADHD Combined patients. Conceivably, the extent of differences between children with the Inattentive subtype of ADHD and controls might be maximized if more talented control children are recruited. Nevertheless, as reviewed in the Introduction, throughout this emerging literature children with the Combined subtype of ADHD often display greater executive deficits than do their peers with the Inattentive subtype. Although these results are consistent with the view that the two subtypes may represent qualitatively different disorders (Barkley, 1997; Milich, Balentine, & Lynam, 2001), some have objected that the evidence does not allow for such a sharp differentiation (Hinshaw, 2001).
A further difference between ADHD subtypes was that the benefit of methylphenidate on TOH performance was found for only patients with the Inattentive subtype. However, this apparent difference is based on a comparison of participants who received placebo and methylphenidate in the session following the Baseline as opposed to more sensitive within-participant comparisons that were not possible because of practice effects. Nevertheless, these findings are intriguing and warrant replication. Importantly, the possibility remains that higher doses of methylphenidate might eliminate these differences between the two subtypes. Considering the ADHD sample as a whole, the present results are consistent with Aman et al.'s (1998) report of increased correct TOH solutions by boys with ADHD when treated with methylphenidate. Although the differences between subtypes of ADHD in responsiveness to stimulants require further investigation, it appears that methylphenidate attenuates these children's planning/working memory deficits as measured by the TOH.
Notably, we had not anticipated large practice effects on the TOH and expected TOH performance to stabilize after the Baseline session. Practice effects have been reported for mentally retarded participants on TOH (Borys et al., 1982) and for a normative population on TOL (Culbertson & Zillmer, 2001). However, Bishop, Aamodt-Leeper, Creswell, McGurk, and Skuse (2001) found little gain by children of normal intelligence on readministration of TOH.
As we previously reported (Klorman et al., 1999), children with the Combined subtype of ADHD committed more violations than both controls and patients with the Inattentive subtype of ADHD. However, whereas we previously found nearly identical rates of violations among controls and patients with the Inattentive subtype of ADHD, the present Inattentive sample broke rules more often than controls. Despite these differences between ADHD subtypes in the frequency of rule breaks in the medication-free Baseline, the reduction of violations by methylphenidate was comparable for ADHD children of both subtypes.
Rule breaks may represent disinhibition as well as memory lapses. It is unlikely that rule breaks result largely from oppositionality because these infractions were infrequent even in the Combined cohort, which had the highest proportion of diagnoses of Oppositional Defiant Disorder and Conduct Disorder. An alternative interpretation of rule breaks is that they reflect occasional confusion or failure to recall the rules, a hypothesis consistent with the reduction of rule violations with increased experience in the task over sessions. Further, as already mentioned, rule breaks were quite low in both of our studies, so that discrepancies in performance between diagnostic groups or pharmacologic conditions cannot be attributed to corresponding differences in rule violations.
Depth of Search
Although long DOS reduced correct solutions and lengthened response latencies for all three groups, the results did not confirm our expectation that long DOS would amplify TOH performance deficits by patients with ADHD. The rationale behind the DOS manipulation was that it reflects cognitive processing required for a minimum path solution, and, hence, DOS is arguably a more valid way of quantifying planning in TOH than full solution length (Spitz et al., 1984). Although solutions were indeed lower on puzzles with long DOS, control children outperformed participants with ADHD to a similar extent on low- and high-DOS puzzles. Thus, the present results suggest that planning or spatial working memory, as defined by our manipulation of DOS, does not underlie ADHD children's TOH deficits.
The present paradigm may not have been optimal in at least two respects. First, short and long DOS sets differed by only one move, so that planning demands might be deemed as insufficiently discrepant across conditions, However, in both Spitz et al.'s (1984) and our study, this long DOS manipulation resulted in lower performance as well as slower reactions and more self-regulatory utterances under failure, all indications of greater cognitive challenge. A second possible limitation of our task is that, also following Spitz et al. (1984), solutions to consecutive problems within each DOS level included all the steps of the preceding puzzle plus one novel additional step. This feature of the task may have potentiated practice effects within each DOS set, and consequently, may have attenuated the need for planning in subsequent problems.
Private Speech
Children in all groups exhibited higher rates of self-regulatory than not self-regulatory verbalizations during the TOH task. This finding is consistent with previous results for children with learning disability, children with ADHD, and comparison children (Berk & Landau, 1993; Winsler, 1998). As also reported by Winsler (1998), private utterances were more frequent under failure than success. Vygotsky's (1934/1962) theory that private speech hones children's ability to attend to their environments and master their actions is supported by evidence that private speech increases with task difficulty (Berk, 1986; Berk & Garvin, 1984; Goodman, 1981) and at points of failure during problem solving (Goodman, 1981). An alternative, but not incompatible view, is that responses to failed puzzles may have been executed more slowly, thereby affording a greater opportunity for private utterances.
In contrast to our prediction, DOS did not affect the number of private verbalizations of any diagnostic group. This result was surprising because long DOS puzzles elicited fewer correct solutions and, as summarized earlier, task difficulty generally increases private speech through a hypothesized mechanism of self-regulation. This negative finding suggests that our participants did not experience the present DOS manipulation as a challenge that necessitated heightened self-regulation.
The main diagnostic differences regarding private speech involved a greater number of verbalizations under failure by patients with both types of ADHD than by controls, a result consistent with past research (Berk & Landau, 1993; Berk & Potts, 1991). Berk and Potts (1991) proposed that impaired attentional processes in ADHD undermine effective functioning of self-directed speech and, therefore, children with ADHD progress more slowly toward the internalization of private speech. Failure may have exacerbated the higher rate of private verbalizations by children with ADHD because instructions and feedback on performance heightened awareness of failure. Notably, other paradigms like self-administered arithmetic tests sometimes used in this research do not provide immediate external feedback to the student.
The greater preponderance of self-regulatory speech versus not self-regulatory utterances in all samples implies that, as noted by Winsler (1998), it is not fruitful merely to foster increased self-regulatory utterances by children with ADHD, insofar as they spontaneously produce these verbalizations at a higher rate than unaffected controls. Rather, therapy should aim at increasing private speech that prompts attention to strategies that enhance performance on the task at hand (Meichenbaum & Goodman, 1979).
Contrary to prediction, notwithstanding their discrepant TOH performance, the two subtypes of ADHD were comparable in their overall rate of private verbalizations in the Baseline session. This result suggests that spontaneous speech is complexly related to task difficulty.
Differences in the rate of private verbalizations of the two subtypes of ADHD were obtained in the pattern of change with repeated testing. Over sessions children with the Inattentive subtype, compared with their Combined counterparts, displayed a greater attenuation of the effect of failure on self-regulatory speech. Specifically, patients with the Inattentive subtype reduced their volubility under failure independent of pharmacologic condition. Importantly, this change by the Inattentive cohort represents a move towards the pattern exhibited by control participants in the Baseline session. Unfortunately, the low rate of failure by controls in later sessions made it difficult to determine whether they also react less to failure over sessions in the rate of private speech. Notably, though, patients with the Combined type of ADHD lowered their rate of self-regulatory speech only with methylphenidate treatment. Following Vygotsky's position, patients with the Inattentive subtype of ADHD achieved sufficient mastery of the task after one session's experience so that they did not use increased self-regulatory speech to deal with challenging puzzles. In contrast, patients with the Combined subtype of ADHD required stimulant therapy to approach the pattern of reaction exhibited by control participants in the Baseline session.
Importantly, several effects of practice emerged in this study: marked improvement in TOH performance, reduction of rule breaks, and attenuation in the inattentive sample of increased self-regulatory utterances under failure. One implication of these results is that enhancement of some executive skills may be attained by children with ADHD through sheer practice without more intensive interventions like medication or training. However, a rigorous test of this hypothesis requires testing for transfer on a related but structurally different task.
CONCLUSION
We found both similarities and differences between subtypes of ADHD in TOH performance and private speech in both the medication-free Baseline session as well as under double-blind stimulant administration. Admittedly, some of the similarities between subtypes may reflect insufficient statistical power because of the relatively small size of our ADHD samples. Patients with the Inattentive subtype were less deficient on the task in the medication-free Baseline than those with the Combined subtype and improved more under methylphenidate. In contrast, although children with the Combined subtype broke rules more often than those with the Inattentive type, both subtypes of ADHD exceeded controls in this respect and benefited comparably from stimulant treatment. Overall, the results point to greater deficits by children with the Combined subtype of ADHD in the executive functions tapped by TOH, and possibly lesser benefit in this respect from stimulant therapy. Another similarity between subtypes of ADHD was a larger increase in the Baseline session than controls for spontaneous utterances under failure. However, patients with the Inattentive subtype decreased their self-regulatory speech under failure merely through experience with the task whereas ADHD Combined patients required stimulant treatment to exhibit this normative pattern. These results point to both contrasting and shared characteristics of children with the inattentive and combined subtypes of ADHD.
ACKNOWLEDGMENTS
This research was supported by NIMH Grant MH56571. We thank Chad Swenson and the Strong Memorial Hospital Pharmacy Department for help with the drug trial, Erin Gorman and Nora Ilniczky for assistance in testing participants. Loisa Bennetto for her comments on an earlier draft, and Rosemary Tannock for making available the P. I. C. S.--4.
REFERENCES
Ackerman, R. T., Anhalt, J. M., Dykman, R. A., & Holcomb, P. J. (1986). Effortful processing deficits in children with reading and/or attention disorders. Brain and Cognition, 5, 22-40.
Aman, C. J., Roberts, R. J., Jr., & Pennington, B. F. (1998). A neuropsychological examination of the underlying deficit in attention deficit hyperactivity disorder: Frontal lobe versus right parietal lobe theories. Developmental Psychology, 34, 956-969.
Barkley, R. A. (1997). ADHD and the nature of self-control. New York: Guilford.
Barkley, R. A., DuPaul, G. J., & McMurray, B. (1990). Comprehensive evaluation of attention deficit disorder with and without hyperactivity as defined by research criteria. Journal of Consulting and Clinical Psychology, 58, 775-789.
Barkley, R. A., DuPaul, G. J., & McMurray, B. (1991). Attention Deficit Disorder with and without hyperactivity: Clinical response to three dose levels of methylphenidate. Pediatrics, 87, 519-531.
Barkley, R. A., Grodzinsky, G., & DuPaul, G. J. (1992). Frontal lobe functions in Attention Deficit Disorder with and without hyperactivity: A review and research report. Journal of Abnormal Child Psychology, 20, 163-188.
Beaudichon, J. (1973). Nature and instrumental function of private speech in problem solving situations. Merrill-Palmer Quarterly, 19, 117-135.
Berk, L. E. (1986). Relationship of elementary school children's private speech to behavioral accompaniment to task, attention, and task performance. Developmental Psychology, 22, 671-680.
Berk, L. E., & Garvin, R. A. (1984). Development of private speech among low-income Appalachian children. Developmental Psychology, 20, 271-286.
Berk, L. E., & Landau, S. (1993). Private speech of learning disabled and normally achieving children in classroom academic and laboratory contexts. Child Development, 64, 556-571.
Berk, L. E., & Potts, M. (1991). Development and functional significance of private speech among attention-deficit hyperactivity disordered and normal boys. Journal of Abnormal Child Psychology, 19, 357-377.
Bishop, D. V. M., Aamodt-Leeper, G., Creswell, C., McGurk, R., & Skuse, D. H. (2001). Individual differences in cognitive planning on the Tower of Hanoi task: Neuropsychological maturity or measurement error? Journal of Child Psychology and Psychiatry, 42, 551-556.
Bivens, J. A., & Berk, L. E. (1990). A longitudinal study of the development of elementary school children's private speech. Merrill-Palmer Quarterly, 36, 443-463.
Borys, S. V., Spitz, H. H., & Dorans, B. A. (1982). Tower of Hanoi performance of retarded young adults and nonretarded children as a function of solution length and goal state. Journal of Experimental Child Psychology, 33, 87-110.
Campbell, S. B. (1973). Cognitive styles in reflective, impulsive, and hyperactive boys and their mothers. Perceptual and Motor Skills. 36, 747-752.
Carlson, C. L., & Mann, M. (2000). Attention-Deficit/Hyperactivity Disorder, predominantly inattentive subtype. Child and Adolescent Psychiatric Clinics of North America, 9, 499-510.
Chhabildas, N. Pennington, B. F., & Willcutt, E. G. (2001). A comparison of the neuropsychological profiles of the DSM-IV subtypes of ADHD. Journal of Abnormal Child Psychology, 29, 529-540.
Chang, H. T. (2000). Effects of methylphenidate on performance and private speech of children with Attention-Deficit/Hyperactivity Disorder during the Tower of Hanoi Task. Unpublished doctoral dissertation, University of Rochester, Rochester, NY.
Copeland, A. P. (1979). Types of private speech produced by hyperactive and nonhyperactive boys. Journal of Abnormal Child Psychology. 7, 169-177.
Culbertson, W. C., & Zillmer, E. A. (2001). Tower of London. North Tonawanda, NY: Multi-Health Systems.
Douglas, V. I. (1999). Cognitive control processes in Attention-Deficit/Hyperactivity Disorder. In H. C. Quay & A. E. Hogan (Eds.), Handbook of disruptive behavior disorders (pp. 105-138). New York: Kluwer Academic/Plenum.
DuPaul, G. J. (1991). Parent and teacher ratings of ADHD symptoms; Psychometric properties in a community-based sample. Journal of Clinical Child Psychology, 20, 242-253.
Faraone, S. V., Biederman, J., Weber, W., & Russell, R. L. (1998). Psychiatric, neuropsychological, and psychosocial features of DSM-IV subtypes of Attention-Deficit/Hyperactivity Disorder: Results from a clinically referred sample. Journal of the American Academy of Child and Adolescent Psychiatry, 37, 185-193.
Frauenglass, M., & Diaz, R. (1985). Self-regulatory functions of children's private speech: A critical analysis of recent challenges to Vygotsky's theory. Developmental Psychology, 21, 357-364.
Goel, V., & Grafman, J. (1995). Are the frontal lobes implicated in planning functions? Interpreting data from the Tower of Hanoi. Neuropsychologia, 5, 623-642.
Goodman, S. H. (1981). The integration of verbal and motor behavior in preschool children. Child Development, 52, 280-289.
Hinshaw, S. P. (2001). Is the inattentive type of ADHD a separate disorder? Clinical Psychology: Science and Practice. 8, 498-501.
Houghton, S., Douglas. G., West, J., Whiting, K., Wall, M., Langsford, S., Powell, L., & Carroll, A. (1999). Differential patterns of executive function in children with Attention-Deficit Hyperactivity Disorder according to gender and subtype. Journal of Child Neurology, 14, 801-805.
Kaufman, A. S., & Kaufman, N. C. (1985). Kaufman tests of academic achievement. Circle Pines, MN: American Guidance Service.
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., Williamson, D., & Ryan, N. (1998). Schedule for affective disorders and schizophrenia for school-age children--Present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of American Academy of Child & Adolescent Psychiatry, 36, 980-988.
Klein, W. L. (1964). An investigation of the spontaneous speech of children during problem solving. Dissertation Abstracts International, 25, 2031. (University Microfilms No. 64-09, 240).
Klorman, R., Hazel-Fernandez, L. A., Shaywitz, S. L., Fletcher, J. M., Marchione, K. E., Holahan, J. M., Stuebing, K. K., Brumaghim, J. T., & Shaywitz, B. A. (1999). Executive functioning deficits in attention deficit/hyperactivity disorder are independent of oppositional defiant or reading disorder. Journal of American Academy of Child and Adolescent Psychiatry, 38, 1148-1155.
Kohlberg, L. Yaeger, J., & Hjertholm, E. (1968). Private speech: Four studies and a review of theories. Child Development, 39, 691-736.
Lahey, B., & Carlson, C. (1991). Validity of diagnostic category of attention deficit disorder without hyperactivity: A review of the literature. Journal of Learning Disabilities, 24, 110-120.
McBurnett, K. (2000). Methylphenidate treatment of DSM-IV types of Attention Deficit Hyperactivity Disorder. In L. Greenhill, and B. Osman (Eds.), Ritalin Theory and practice (2nd ed., pp. 253-263). Larchmont, NY: M. A. Liebert.
Meichenbaum, D., & Biemiller, A. (1990, May). In search of student expertise in the classroom: A metacognitive analysis. Paper presented at the conference on Cognitive Research for Instructional Innovation, University of Maryland, College Park, Maryland.
Meichenbaum, D., & Goodman, S. (1979). Clinical use of private speech and critical questions about its study in natural settings. In G. Zivin (Ed.), The development of self-regulation through private speech (pp. 325-360). New York: Wiley.
Milich, R., Balentine, A. C., & Lynam, D. R. (2001). ADHD combined type and ADHD predominantly inattentive type are distinct and unrelated disorders. Clinical Psychology: Science and Practice, 8, 463-488.
MTA Cooperative Group (1999). A 14-month randomized clinical trial of treatment strategies for Attention-Deficit/Hyperactivity Disorder. Archives of General Psychiatry, 56, 1073-1086.
Murray, J. D. (1979). Spontaneous private speech and performance on a delayed match-to-sample task. Journal of Experimental Child Psychology, 27, 286-302.
Nigg, J. T., Blaskey, L. G., Huang-Pollock, C., & Rappley, M. D. (2002). Neuropsychological executive functions and DSM-IV ADHD subtypes. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 59-66.
Owen, A. M., Downes, J. J., Sahakian, B. J., Polkey, C. E., & Robbins, T. W. (1990). Planning and spatial working memory following frontal lobe lesions in man. Neuropsychologia, 28, 1021-1034.
Ozonoff, S., & Jensen, J. (1999). Specific executive function profiles in three neurodevelopmental disorders. Journal of Autism and Developmental Disorders, 29, 171-177.
Paternite, C. E., Loney, J., & Roberts, M. A. (1996). A preliminary validation of subtypes of DSM-IV Attention-Deficit/Hyperactivity Disorder. Journal of Attention Disorders, 1, 70-86.
Pennington, B. F., Groisser, D., & Welsh, M. C. (1993). Contrasting cognitive deficits in attention deficit hyperactivity disorder versus reading disability. Developmental Psychology, 29, 511-523.
Pennington, B. F., & Ozonoff, S. (1996). Executive functions and developmental psychopathology. Journal of Child Psychology and Psychiatry, 37, 51-87.
Schachar, R., Ickowicz, A., & Wachsmuth, R. (1995). Parent Interview for Child Symptoms (P.I.C.S.-4). Unpublished document, The Hospital for Sick Children, Toronto, ON Canada.
Sergeant, J. A., Geurts, H., & Oosterlaan, J. (2002). How specific is a deficit of executive functioning for Attention-Deficit/Hyperactivity Disorder? Behavioural Brain Research, 130, 3-28.
Shallice, T. (1982). Specific impairments of planning. Philosophical Transactions of the Royal Society of London, 298, 199-209.
Simon, H. (1975). The functional equivalence of problem solving skills. Cognitive Psychology, 7, 268-288.
Spitz, H. H., Minsky, S. K., & Bessellieu, C. L. (1984). Subgoal length versus full solution length in predicting Tower of Hanoi problem-solving performance. Bulletin of Psychonomic Society, 22, 301-304.
Spitz, H. H., Minsky, S. K., & Bessellieu, C. L. (1985). Influence of planning time and first-move strategy on Tower of Hanoi problem-solving performance of mentally retarded young adults and nonretarded children. American Journal of Mental Deficiency, 90, 49-56.
Spitz, H. H., Webster, N. A., & Borys, S. V. (1982). Further studies of the Tower of Hanoi problem-solving performance of retarded young adults and nonretarded children. Developmental Psychology, 18, 922-930.
Vygotsky, L. (1934/1962). Thought and language. Cambridge, MA: MIT Press.
Wechsler, D. (1991). Manual for the Wechsler Intelligence Scale for Children--Third edition. San Antonio, TX: The Psychological Corporation.
Weyandt, L. L. & Willis, W. G. (1994). Executive functions in school-aged children: Potential efficacy of tasks in discriminating clinical groups. Developmental Neuropsychology, 10, 27-38.
Winsler, A. (1998). Parent-child interactions and private speech in boys with ADHD. Applied Developmental Science, 2, 17-39.
Woodcock, R. W., & Johnson, M. B. (1989). Woodcock Johnson Psychoeducational Battery--Revised Allen. TX: DLM Teaching Resources.
Zentall, S. S., Gohs, D. E., & Culatta, B. (1983). Language and activity of hyperactive and comparison children during listening tasks. Exceptional Children, 50, 255-266.
Zivin, G. (1972). Functions of private speech during problem-solving in preschool children. Dissertation Abstracts International, 33 (2-B), 1834. (University Microfilms No. 72-26, 224).
Helena Kopecky, (2) H. Theresa Chang, (2,3) Rafael Klorman, (2,5) Joan E. Thatcher, (2) and Agneta D. Borgstedt (4)
Received March 15, 2004; revision received July 29, 2004; accepted November 24, 2004
(1) Portions of these results were submitted as part of H. Theresa Chang's PhD dissertation (Chang, 2000) and Helena Kopecky's unpublished master's research, both conducted at the University of Rochester and supervised by Rafael Klorman.
(2) Department of Clinical and Social Sciences in Psychology, University of Rochester, Rochester, NY.
(3) Currently at Carle Clinic Association, Urbana-Champaign, IL.
(4) Department of Pediatrics, University of Rochester, Rochester, NY.
(5) Address all correspondence to, Rafael Klorman, RC Box 270266, Meliora Hall, University of Rochester, Rochester, NY 14627-0266; e-mail: rafael.klorman@rochester.edu.
COPYRIGHT 2005 Plenum Publishing Corporation
COPYRIGHT 2005 Gale Group