Abstract
Since rosacea is a chronic disease and many patients find prescription therapies unsatisfactory, they frequently turn to herbal ingredients for relief of their persistent facial redness. The most useful and frequently used herbal compounds include licorice, feverfew, green tea, oatmeal, lavender, chamomile, tea tree oil, and camphor oil. The utility of most of these herbs is based on their purported anti-inflammatory properties. Some of these herbs have proven effects, many have potential benefits, and some may aggravate rosacea. Due to the fact that many patients fail to inform their physicians about their use of herbal ingredients, dermatologists should be aware of what patients may be using and be able to advise them about the efficacy of these ingredients or the potential for adverse effects.
Introduction
Since the skin of the face is the most common site of involvement, rosacea often has an adverse impact on patient quality of life. In recent surveys by the National Rosacea Society, nearly 70% of rosacea patients indicated that their rosacea decreased their self-confidence and self-esteem, and 41% reported that rosacea had caused them to avoid public contact or cancel social engagements. (1) Among rosacea patients with severe symptoms, nearly 70% said the disorder had adversely affected their professional interactions, and nearly 30% said they had even missed work. (1)
Treatment of rosacea is chronic and the results achieved with pharmacologic therapies are often unsatisfactory. In addition, many patients exhibit sensitivity to topical therapeutic agents and the resulting inflammation may aggravate and accelerate the progression of the disease. Many patients use topical over-the-counter (OTC) agents to treat the symptoms of rosacea, either as an alternative to traditional prescriptions or to complement their prescription regimen. Increasingly, many of these OTC preparations contain herbs. Current estimates report that consumers in the US spend more than 21 billion dollars on alternative medicine and the use of herbal remedies saw an unprecedented 380% increase between 1990 and 1997. (2)
By definition, herbs are botanicals used for medicinal purposes, flavoring, or fragrance. Herbal medicine is based upon the principle that the naturally occurring mixture of active plant compounds is more effective and safer than individual molecules and manufactured combinations of synthetic compounds. (3) Herbal medicine plays several roles in the American medical system by providing alternatives to prescription medications, enhancing the therapeutic effects of other prescriptions and protecting against allopathic side effects, and providing treatments for conditions lacking prescriptive cures or for which there are only high-risk or ineffective therapies.
Quality control in the formulation of herbal preparations poses the challenge of balancing the need for consistency in processing the raw materials while maintaining the potency of the bioactivity of the botanical. The greatest task in producing an effective herbal preparation or herbal cosmeceutical is standardization of the herbal extract as each source plant may contain variability in marker compounds as well as individual components due to variable growing conditions and differences in harvesting procedures that may impact the composition of the herb and the active ingredients. Other issues include appropriate plant identification, genetic variability, adulteration, and batch-to-batch variation.
Herbs Used to Treat Rosacea
Licorice
Licorice plants of the genus Glycyrrhiza have long been used in Chinese medicine for their noted therapeutic effects against a wide range of diseases. The plant was introduced to the Ancient Greeks by the Scythians and has been used since the Middle Ages. Today, several varieties of licorice grow wildly in the lands between southeastern Europe, south-western Asia, and Iraq.
Glycyrrhizin, one of the main ingredients in licorice, is believed to contribute to the herb's many healing properties. Laboratory studies have shown that glycyrrhizin reduces inflammation, promotes mucous secretion, soothes irritation, and stimulates adrenal gland activity. (4) Glycyrrhizin also appears to have antiviral properties, combating hepatitis B, influenza, and HIV by boosting T-cell counts and stimulating production of interferon and other protective compounds. (5) Other ingredients improve stomach ulcers (glycyrrhizinic acid) and soothe inflammation (glabridin and licoicidin).
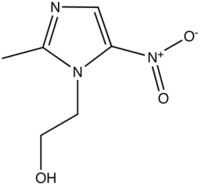
The genus is diverse, with more than 30 species of Glycyrrhiza. G glabra and G inflata are the two most-studied. Glabridin is the active component of G glabra (Figure 1). A study by Yokota and associates reported that a 0.5% glabridin solution inhibited UVB-induced pigmentation and erythema. (6) The compound's anti-inflammatory properties are due to the inhibition of superoxide anion production and cyclooxygenase activity.
Glycyrrhizinic acid has also been shown to improve dermatitis. In a study by Saeedi and associates, 2% glycyrrhizinic acid gel was reported to significantly decrease scores for erythema, edema, and itching over the 2-week treatment period. (7)
Licochalcone A, a retrochalcone derived from Glycyrrhiza inflata has been shown to inhibit proinflammatory cytokines, eicosanoids, and reactive oxygen species in human skin cells. (8,9) Licochalcone has also been reported to have antimicrobial and immunosuppressive properties. (10,11) A recent study by Dieck and associates found that licochalcone A exhibited a potent anti-inflammatory action on a broad range of skin cells involved in skin inflammation. (9) The authors concluded that the observed high therapeutic index of the compound indicated that licochalcone A may be a promising candidate for dermatologic or cosmetic applications. In a recent study by Weber et al, 8 weeks of a skin care regimen containing licochalcone (Eucerin Redness Relief) provided statistically significant improvements in mean erythema scores of patients with mild-to-moderate erythematotelangiectatic rosacea or red facial skin not attributable to rosacea. (12) These patients also reported an improved quality of life that corresponded with the reduction in redness. Formulations containing licochalcone are compatible with Metrogel and Azelex.
Feverfew
Feverfew (Tanacetum parthenium), a member of the composite family which also includes Marigold, Echinacea, and Chamomile, has long been used in traditional and folk medicine to treat migraines, fever, and arthritis (5) (Figure 2). One of the primary active components of feverfew, parthenolide, inhibits serotonin release from platelets. (5,13) Feverfew inhibits 5-lipoxygenase and cyclooxygenase, resulting in a reduction in human blood platelet aggregation.
[FIGURE 1 OMITTED]
Although the potential of the herb for the treatment of inflammatory skin disorders has long been postulated, parthenolide is a known skin sensitizer and its use, therefore, is contraindicated in a skin care product. To address this issue, a parthenolide-free extract of feverfew was developed (feverfew PFE[TM]). As expected, this compound eliminated the risk of skin sensitization. An unexpected effect, however, was the finding that the compound exhibited strong immunomodulatory activity. (14) In a recent study by Martin and associates, 45 days of treatment with 1% feverfew PFE[TM] (Aveeno Daily Moisturizer Ultracalming[TM]) improved mild inflammatory acne by inhibiting the release of inflammatory markers from activated lymphocytes and reducing neutrophil chemotaxis. (14) It is these immunomodulating properties that suggest feverfew PFE[TM] may be a useful treatment for rosacea.
Green Tea
Green tea extracts have gained popularity in recent years as a treatment for signs of skin aging. Green tea extracts, derived from the bud and leaf of the plant Camellia sinensis, contain large amounts of polyphenolic compounds. The green tea derivatives epicatechin, epigallocatechin, epicatechin-3-gallate, and epigallocatechin-3-gallate possess well-documented anticarcinogenic properties and anti-inflammatory and antioxidant capabilities. (15) These properties are especially useful for patients with rosacea as inherent sun sensitivity is a hallmark of the disease. The photoprotective properties of green tea may lessen reactivity to ultraviolet light, thereby reducing the signs and symptoms of rosacea. Moreover, green tea extract has been shown to reduce the disruption of the skin barrier often seen in patients with the disease. (16) Green tea may also directly improve the signs of rosacea by reducing the number and appearance of telangiectasias. (17)
[FIGURE 2 OMITTED]
Oatmeal
The US Food and Drug Administration classifies colloidal oatmeal (the powder resulting from the grinding and processing of whole oat grain) as a skin protectant ingredient that "provides temporary skin protection and relieves minor skin irritation and itching due to poison oak, poison ivy, poison sumac, and insect bites." The properties that make oatmeal useful for these itchy and allergic conditions, however, make it an especially efficacious ingredient for rosacea therapies.
First, oatmeal is a potent antipruritic. The moisturizing properties of colloidal oatmeal alleviate itch due to dry skin. These properties, in turn, promote protection of barrier function, which is often impaired in rosacea patients. Oatmeal also works as a skin protectant and enhancer of barrier function as the proteins and polysaccharides bind to skin to provide a protective barrier, while proteins buffer both acids and bases. Further, oat flour has been shown to display antioxidant properties and oil emulsions prevent transepidermal water loss. (18)
Oatmeal has anti-inflammatory properties. A study by Saeed and associates reported that a 10% colloidal oatmeal suspension inhibited prostaglandin synthesis by as much as 85%. (19) The magnitude of prostaglandin inhibition was similar to that reported with indomethacin.
Finally, oatmeal is an effective cleanser that contains saponins that absorb dirt, oil, and sebaceous secretions while hydrophilic and lipophilic components absorb and solubilize aqueous debris. (18)
Other Botanicals
Lavender
Essential oils distilled from members of the genus Lavandula have been used both cosmetically and therapeutically for centuries with the most commonly used species being L. angustifolia, L. latifolia, L. stoechas, and L. x intermedia. Although there is considerable anecdotal information about the biological activity of these oils, most has not been substantiated by scientific or clinical evidence. Among the claims made for lavender oil are that is it antibacterial, antifungal, carminative (smooth muscle relaxing), sedative, antidepressive and effective for burns and insect bites. (20)
Lavandula angustifolia has been used in Iranian medicine for centuries as a treatment for a variety of inflammatory pathologies. Although further research is needed to identify the active chemical ingredient(s), studies in animal models confirm the traditional use of Lavandula angustifolia for the treatment of painful and inflammatory conditions (21) (including gastrointestinal disorders, migraines, and generalized pain).
Chamomile
Chamomile extracts and tea are widely used for the treatment of indigestion and inflammation. Chamomile refers to 2 distinct plants. Matricaria recutita is known as German or Hungarian chamomile, and Chamaemelum nobile is known as Roman or English chamomile. Both plants are used for the same indications. The active constituents of chamomile include the terpenoids (bisoprolol, matricin, chamazulene) and flavonoids (apigenin, luteolin). (22) Studies have documented the anti-inflammatory and soothing effects of creams containing chamomile in patients with various inflammatory dermatoses. (23) Chamomile is used in a variety of cosmetic products and as soothing compresses.
Tea Tree Oil
Tea tree oil is the essential oil steam-distilled from Melaleuca alternifolia, an Australian native plant. In recent years it has become increasingly popular as an antimicrobial agent and has also been demonstrated to possess anti-inflammatory properties. (24) Tea tree oil should be used with caution, however, as it has been associated with a wide variety of side effects including allergic contact dermatitis, systemic contact dermatitis, erythema, and systemic hypersensitivity reactions as well as conditions such as linear immunoglobulin A disease. (25)
Camphor Oil
Camphor is a white crystalline substance, obtained from the tree Cinnamonum camphora, but the name has been given to various odorous volatile products derived from different aromatic plants. The commercial camphor is extracted from C. camphora and Dryobalanops camphora (fam. Dipterocarpacaea). Camphor has been used historically for its calming influence in hysteria, nervousness and neuralgia, and for diarrhea, arthritis, sprains, bronchitis, and in inflammatory conditions. It is also often used to relieve symptoms of colds, chills, and for the treatment of anti-inflammatory conditions.
Recently, camphor oil has been evaluated for its efficacy in treating the demodicoses that are frequently comorbid with rosacea. (26) In a study by Morsy, marked reduction in the infestation density were noted following application of diluted camphor oil at concentrations of 20% to 25%. (27) Caution is warranted with the use of camphor oil, however, as it is a known skin irritant.
Discussion
The therapeutic value of medicinal herbs has gained increased acceptance by the medical profession. However, there are a number of variables which can influence the composition, concentration, and bioavailability of the herbal compound. Moreover, few of these ingredients have been evaluated in clinical trials. Despite these issues, many patients may benefit from the use of herbal remedies and a growing number of patients are using "natural" ingredients to treat their rosacea. Some have proven effects, many have potential benefits, and some may, in fact, aggravate rosacea. Of particular concern is the finding that patients using alternative therapies are unlikely to tell their doctor. (2) Dermatologists should be aware of what patients are using and be able to advise them, beyond what is prescribed or the procedures performed.
Disclosure
Dr. Wu is a consultant for Johnson and Johnson Consumer Products and is Founder and President of Dr. Jessica Wu Cosmeceuticals.
References
1. National Rosacea Society. 14 million Americans have rosacea and most of them don't even know it. Available at: http://www.rosacea.org. Accessed November 3, 2005.
2. Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990-1997: results of a follow-up national survey. JAMA. 1998;280:1569-75.
3. Thornfeldt C. Cosmeceuticals containing herbs: fact, fiction, and future. Dermatol Surg. 2005;31:873-80; discussion 880.
4. University of Maryland Medical Center. Available at: http://www.umm.edu/altmed/ConsHerbs/Licoricech.html. Accessed November 7, 2005.
5. PDR for herbal medicines. Montvale (NJ): Thompson Medical Economics; 2000. Ginseng: 346-51.
6. Yokota T, Nishio H, Kubota Y, Mizoguchi M. The inhibitory effect of glabridin from licorice extracts on melanogenesis and inflammation. Pigment Cell Res. 1998;11:355-61.
7. Saeedi M, Morteza-Semnani K, Ghoreishi MR. The treatment of atopic dermatitis with licorice gel. J Dermatolog Treat. 2003;14:1537.
8. Immeyer J, Wensorra U, Dieck K, et al. Anti-inflammatory properties of synthetic licochalcone A and aqueous extracts from Glycyrrhiza inflata. In press.
9. Dieck K, Ceilley RI, Immeyer J, et al. Anti-inflammatory properties of licochalone A from Glycyrrhiza inflate on various human cells. Presented at the Annual Meeting of the American Academy of Dermatology, 2005, New Orleans, LA.
10. Fukai T, Marumo A, Kaitou K, et al. Anti-Helicobacter pylori flavonoids from licorice extract. Life Sci. 2002;71:1449-63.
11. Barfod I, Kemp K, Hansen M, Kharazmi A. Chalcones from Chinese licorice inhibit proliferation of T cells ans production of cytokines. Int Immunopharmacol. 2002;2:545-55.
12. Weber TM, Scholermann A, Burger A, et al. Tolerance and efficacy of a skin care regimen containing licochalcone A for adults with erythematic rosacea and facial redness. Presented at the Annual Meeting of the American Academy of Dermatology, 2005, New Orelans, LA.
13. Groenewegen WA, Heptinstall S. A comparison of the effects of an extract of feverfew and parthenolide, a component of feverfew, on human platelet activity in-vitro. J Pharm Pharmacol. 1990;42:553-7.
14. Martin K, Southall C, Saliou C. Clinical and immunomodulatory effects of parthenolide-depleted Tanacetum. European Academy of Dermatology and Venereology, November 17-21, 2004, Florence, Italy.
15. Katiyar SK, Elmets CA. Green tea polyphenolic antioxidants and skin photoprotection. Int J Oncol. 2001;18:1307-13.
16. Hsu S. Green tea and the skin. J Am Acad Dermatol. 2005;52:1049-59.
17. Chiu AE, Chan JL, Kern DG, et al. Double-blinded, placebo-controlled trial of green tea extracts in the clinical and histologic appearance of photoaging skin. Dermatol Surg. 2005;31:855-859.
18. Webster FH. Oat utilization: past, present, and future. In: Webster FH, ed. Oats: Chemistry and Technology. St Paul, Minn: American Association of Cereal Chemists. Inc; 1986:413-426.
19. Saeed SA, Butt NM, McDonald-Gibson WJ, Collier HOJ. Inhibitor(s) of prostaglandin biosynthesis in extracts of oat (Avena sativa) seeds. Biochemical Soc Trans. 1981;9:444.
20. Cavanagh HM, Wilkinson JM. Biological activities of lavender essential oil. Phytother Res. 2002;16:301-8.
21. Hajhashemi V, Ghannadi A, Sharif B. Anti-inflammatory and analgesic properties of the leaf extracts and essential oil of Lavandula angustifolia Mill. J Ethnopharmacol. 2003;89:67-71.
22. Merfort I, Heilmann J. Hagedorn-Leweke U, Lippold BC. In vivo skin penetration studies of camomile flavones. Pharmazie. 1994;49:509-11.
23. Della Loggia R. Chamomile extracts exerted anti-inflammatory effects when applied topically in animal models of inflammation. Plant Med. 1990;56:657-8.
24. Koh KJ, Pearce AL, Marshman G, Finlay-Jones JJ, Hart PH. Tea tree oil reduces histamine-induced skin inflammation. Br J Dermatol. 2002;147:1212-7.
25. Crawford GH, Sciacca JR, James WD. Tea tree oil: cutaneous effects of the extracted oil of Melaleuca alternifolia. Dermatitis. 2004;15:59-66.
26. Forton F, Germaux MA, Brasseur T, et al. Demodicosis and rosacea: epidemiology and significance in daily dermatologic practice. J Am Acad Dermatol. 2005;52:74-87.
27. Morsy TA, Rahem MA, el-Sharkawy EM, Shatat MA. Eucalyptus globulus (camphor oil) against the zoonotic scabies, Sarcoptes scabiei. J Egypt Soc Parasitol. 2003;33:47-53.
Address for Correspondence
Jessica Wu MD
11600 Wilshire Blvd. Suite 322
Los Angeles, CA 90025
Phone: 310-473-5878
Fax: 310-231-8661
e-mail: drwu@drjessicawu.com
Jessica Wu MD
Private Practice, Los Angeles, CA
COPYRIGHT 2006 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2006 Gale Group