Abstract
Background: Metronidazole 0.75% gel and azelaic acid 15% gel are commonly used to treat rosacea. Irritation is a common side effect.
Objective: To assess the cumulative irritation potential of metronidazole 0.75% gel and azelaic acid 15% gel.
Methods: Metronidazole 0.75% gel, azelaic acid 15% gel, and a white petrolatum negative control were applied under occlusive conditions to the upper back of a total of 33 healthy subjects. There were twelve 24-hour applications (4 times a week) and three 72-hour applications on weekends during a 3-week period. Skin reactions (erythema score [+ or -] other local reaction) were assessed within 15 to 30 minutes of removal of the products.
Results: The mean cumulative irritancy index of metronidazole 0.75% gel was significantly lower than that of azelaic acid 15% gel and not significantly higher than the negative control product. There was increasing cumulative irritancy with azelaic acid; no cumulative irritancy was seen for either metronidazole or white petrolatum.
Conclusion: Metronidazole 0.75% gel is less irritating in sustained use than azelaic acid 15% gel.
Introduction
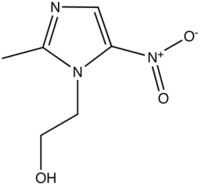
Topical medications, such as metronidazole and azelaic acid, are effective treatments for rosacea (1) and can enhance the efficacy of oral antibiotics. (2,3) One limitation to topical treatment of rosacea is irritation--including dry skin, redness, stinging, and burning. (4,5) Because these irritation reactions can exacerbate the inflammatory component of rosacea, minimizing the irritation potential of topical treatment may be beneficial.
Few studies have been done to compare the irritancy of rosacea medications. Overall, metronidazole has shown a low incidence of adverse events and unwanted side effects. (6) In a comparative trial, symptoms of burning, stinging, and pruritus were less frequent in patients treated with topical metronidazole (7% of subjects) than in those who were treated with topical azelaic acid (26% of subjects). (7)
A cumulative irritation test is a widely-accepted way of determining the irritation potential of certain substances. (8-10) These irritant reactions are the result of direct damage to epidermal cells of the skin and have no immunologic component. After initial and repeated contact with the substance, the skin gradually becomes erythematous and may demonstrate drying, cracking, crusting, and erosion. Vesicles and edema may also develop after repeated exposure to the irritant. (8) In this study, we conducted a single center, active- and negative-controlled, randomized, investigator-blinded, intra-individual study to compare the irritation potential of metronidazole 0.75% gel and azelaic acid 15% gel using a 21-day cumulative irritation patch test.
Methods
Subjects
A total of 33 healthy subjects, 31 females and 2 males between the ages of 20 and 75, were enrolled. Of the 33 subjects enrolled into the study, 31 (94%) completed the study. Two subjects (6%) discontinued. One of the discontinued subjects withdrew due to an adverse event and the other requested withdrawal because of a family emergency. Inclusion criteria required that subjects have a skin photo-type between I and IV on the Fitzpatrick scale (11) so as not to interfere with the reading of skin reactions. Females of childbearing potential were required a negative urine pregnancy test and practice of an effective method of contraception during the study. All subjects had to be willing to comply with the requirements of the frequent visit schedule and concomitant therapy prohibitions and signed a written informed consent.
Subjects who met any of the following criteria were excluded from the study: were pregnant, nursing or planning to become pregnant during the course of the study; had any surgical or medical condition (ie, history of atopic dermatitis or psoriasis) which, in the judgment of the investigator, might have put the subject at risk or interfered with interpretation of the study results; had any known allergies to any of the ingredients of the products or to adhesive tape; had scars, moles, hairs, sunburn, abnormal pigmentation of the skin, or other blemishes in the test area which would have interfered with grading; had participated in another investigational drug or device research study within 3 months or inclusion; and had not respected the washout periods for topical (metronidazole or azelaic acid, 4 weeks; other topicals, 1 week) and/or systemic treatments (corticosteroids or non-steroidal anti-inflammatory drugs, 2 weeks; oral metronidazole, 3 months).
Each subject received instructions as to specific requirements to follow while participating in the study. During the study, the subjects were to avoid exposure to the sun (no sunbathing or other excessive exposure or UV irradiation), use of any cosmetics on the study sites, and baths and showers of the upper back. Participation in any other clinical trial was prohibited during the course of the study.
Design
FDA-approved formulations of metronidazole 0.75% gel (MetroGel[R], Galderma Laboratories, L.P., Fort Worth, TX) and azelaic acid 15% gel (Finacea[TM] Gel, Berlex Laboratories, Montville, NJ) were used at the approved doses. A 0.2 g amount of each of the 2 products and white petrolatum was applied under occlusion to 3 pre-defined, randomized sites (2 cm X 2 cm) that were selected on the upper back of each subject, avoiding any moles, hairs, or non-flat areas. The occlusive dressings were replaced approximately every 24 hours on Monday through Thursday of each week for the 3 weeks of the study. The Friday applications were left in place over the weekend (approximately 72 hours). The Friday evening applications were left in place over the weekend (approximately 72 hours). Each patch site on each subject's back was assessed for erythema and other local cutaneous irritation prior to the initial patch application, and again at every study visit approximately 15 to 30 minutes after patch removal, prior to the following patch application.
All efforts were made to keep the investigator blinded as to the identification of the products applied to the various sites. Thus, an individual other than the investigator removed the product and dressing and applied them at the same sites after the investigator's evaluation and score. The investigator was not permitted to see the randomization list. At no time did the evaluator handle the test products or patches, or have access to the randomization scheme. No products were dispensed to the subjects.
The grading scale used to score erythema of the patch site is shown in Table 1 and other local reactions were documented using the notations shown in Table 2. In case of severe irritation (an erythema scored 3.0 by the investigator or designee according to the clinical evaluation or the symptoms described by the subject) at any site, the product application was discontinued for the incriminated sites which were no longer scored.
For evaluating the cutaneous tolerance, a Cumulative Irritancy Index (CII) was calculated for each treatment and each subject according to previously validated methodology (8,9,12) as follows: CII = Sum of irritation score/Number of readings (with a range for total irritation scores being 0 to 3.0).
The total number of readings in the study was 15 maximum, as there was no evaluation during weekends. Individual CIIs were averaged across subjects to obtain a Mean Cumulative Irritancy Index (MCII) for each treatment. CIIs were submitted to an analysis of variance with effects for subject, zone of involvement, and formulation. Paired two-sided t tests were used to compare CII means across treatment groups. To adjust for multiple comparisons, MCIIs were compared and formulations were classified using the Tukey multiple comparison test, performed at the 1% and 5% significance levels.
Results
The Mean Cumulative Irritancy Index ranged from 0.0253 to 1.0525 for the 2 test products and the negative control, with the lowest irritation observed in sites treated with the negative control and the highest irritation observed in sites treated with azelaic acid (Table 3, Figure 1). Both metronidazole and white petrolatum were significantly less irritating than azelaic acid at both the [alpha] = 0.01 level and the [alpha] = 0.05 level and had MCIIs similar to each other.
Individual reactions to metronidazole and white petrolatum ranged from "0" (no reaction) to "0.5" (erythema barely visible). Individual reactions to azelaic acid ranged from "0" (no reaction) to "3" (severe erythema). A total of 5 subjects had patch discontinuations due to an erythema score of 3.0 or greater; in all cases, these were azelaic acid patches. There was increasing cumulative irritancy with azelaic acid; no cumulative irritancy was seen for either metronidazole or white petrolatum (Figure 2). The efficacy of metronidazole and azelaic acid were not investigated in this study.
Discussion
Irritancy potential is a factor in deciding which agents to use for rosacea. Overall, the tolerability of metronidazole gel and the negative control were relatively similar with a low irritancy potential, meaning that neither of these products caused significant irritancy of the skin over time. In contrast, azelaic acid was significantly less tolerable. These results are in accord with clinical experience. (5,6)
[FIGURE 1 OMITTED]
[FIGURE 2 OMITTED]
Both the product vehicle and mechanism may play roles in the irritancy potential. The metronidazole preparation used in this study is 95% water (personal communication, Cris Osborn, Galderma Laboratories). Though the primary vehicles for metronidazole and azelaic acid were not included among our controls, petrolatum was used because it is generally thought to be non-irritating. Therefore, we are unable to conclude with absolute certainty what component(s) in the azelaic acid gel are more irritating based on this study, and further research may be warranted.
The sample size utilized in this study was small compared to those used in clinical trials evaluating the efficacy and safety of these compounds. However, an n > 30 is generally considered to be a number sufficient to constitute a normal distribution, and our results do not directly conflict with the results of those trials. While the cumulative irritation assay is validated, other potential limitations include variation in the skin irritation response, and intra- and inter-individual variability. (13,14) The severe erythema scores seen in the 5 subjects that dropped out could indicate several things. As no pre-screening patch tests were conducted to ensure that each subject was not allergic to the ingredients of the medications, we cannot definitively say that these scores indicate irritation only and not preexisting sensitization to a component of the azelaic acid gel. Neither can we rule out the induction of sensitization without performing a patch test at an untreated site following the 3-week induction phase. Another limitation is that the irritancy test system is done on the back of healthy volunteers, not the faces of patients with rosacea. However, this is not a major limitation as the validity of the methodology has been well-documented and is suitable for assessing the irritancy of topical agents used on acneiform facial eruptions. (10,15)
Disclosure: This study was funded by Galderma Laboratories, L.P.
References
1. Maddin S. A comparison of topical azelaic acid 20% cream and topical metronidazole 0.75% cream in the treatment of patients with papulopustular rosacea. J Am Acad Dermatol. 1999;40(6 Pt 1):961-5.
2. Altinyazar H, Koca R, Tekin N, Esturk E. Adapalene vs. metronidazole gel for the treatment of rosacea. Int J Dermatol. 2005;44(3):252.
3. Ratnavel R. Rosacea. eMedicine. June 18, 2003. Available from: www.emedicine.com/derm/topic377.htm. Accessed November 3, 2004.
4. Gupta A, Chaudhry M. Topical metronidazole for rosacea. Skin Therapy Lett. 2002;7(1).
5. Drugs Approved by the FDA, Drug Name: Finacea (azelaic acid) Gel, 15%. June 29, 2004. Available from: www.centerwatch.com/patient/drugs/dru818.html. Accessed November 3, 2004.
6. McClellan KJ, Noble S. Topical metronidazole. A review of its use in rosacea. Am J Clin Dermatol. 2000;1(3):191-9.
7. Elewski BE, Fleischer AB, Jr., Pariser DM. A comparison of 15% azelaic acid gel and 0.75% metronidazole gel in the topical treatment of papulopustular rosacea: results of a randomized trial. Arch Dermatol. 2003;139(11):1444-50.
8. Philips L, Steinberg M, Maibach HI, Akers WA. Comparison of rabbit and human skin response to certain irritants. Toxicol Appl Pharmacol. 1972;21:369.
9. Berger RS, Bowman JP. A reappraisal of the 21-day cumulative irritation test in man. J Toxicol--Cut and Ocular Toxical. 1982;1(2):109-15.
10. Queille-Roussel C, Poncet M. Comparison of the cumulative irritation potential of adapolene solution (0.1%) with tazarotene gel and several tretinoin formulations. Clinical Therapeutics. 2001;23(2):205-12.
11. Irwin M. Freedberg, Arthur Z. Eisen, Klaus Wolff, K. Frank Austen, Lowell A. Goldsmith, and Stephen I. Katz, eds. Fitzpatrick's Dermatology in General Medicine, 6th ed. New York, NY; McGraw-Hill, 2003.
12. Cua AB, Wilhelm KP, Maibach HI. Cutaneous sodium lauryl sulphate irritation potential: age and regional variability. Br J Dermatol. 1990;123(5):607-13.
13. Green BG. Regional and individual differences in cutaneous sensitivity to chemical irritants: Capsaicin and menthol. J Toxicol--Cut and Ocular Toxical. 1996;15:277-295.
14. Robinson MK. Intra-individual variations in acute and cumulative skin irritation responses. Contact Dermatitis. 2001;45(2):75-83.
15. Caron D, Sorba V. Skin tolerance of adapalene 0.1% gel in combination with other topical anti-acne treatments. J Amer Acad Child Adol Psych. 1997;36(6):S113-S115.
Address for Correspondence
Steven R. Feldman MD PhD
Department of Dermatology
Wake Forest University School of Medicine
Medical Center Boulevard
Winston-Salem, NC 27157-1071
Phone: 336-716-7740
Fax: 336-716-7732
e-mail: sfeldman@wfubmc.edu
Kristin Ziel MS IV, (a) Christopher B. Yelverton MD MBA, (a) Rajesh Balkrishnan PhD, (b) Steven R. Feldman MD PhD (a)
a. Center for Dermatology Research, Department of Dermatology, Wake Forest, Winston-Salem, NC
b. University School of Medicine, Winston-Salem, NC; Division of Pharmacy Practice and Administration, The Ohio State University, Columbus, OH
COPYRIGHT 2005 Journal of Drugs in Dermatology, Inc.
COPYRIGHT 2005 Gale Group