PHILADELPHIA -- Enzyme replacement therapy has conquered Fabry disease, a rare, lysosomal storage disease.
In two independent reports at the annual meeting of the American Society of Human Genetics, researchers reported successfully resolving Fabry disease symptoms with an infusion of a normal, human enzyme once every 2 weeks.
The enzyme, [alpha]-galactosidase, is now being made by two competing U.S. pharmaceutical companies. Based on the results of the two separate studies reported at the meeting, both companies have submitted licensing applications to the Food and Drug Administration under the Orphan Drug law, and expect a ruling this year. About 2,500 patients in the United States have Fabry disease.
The pathophysiology of Fabry disease centers on the accumulation of glycolipids that cannot be metabolized, and, instead, become deposited in the vascular endothelium. This eventually leads to damage of the skin, heart, and kidneys.
The results from one of the studies reported at the meeting--a 58-patient, placebo-controlled trial--documented that after 20 weeks of enzyme replacement therapy, the stored glycolipid completely disappeared from the renal vasculature in 20 of 29 treated patients. In contrast, none of the 29 patients treated with placebo infusions had clearance of their blood vessels, reported Dr. Christine M. Eng of Baylor College of Medicine in Houston.
"What we expected was that enzyme replacement would stabilize the disease, but what we see is a dramatic reversal," noted Dr. Robert J. Desnick, chairman of the department of human genetics at Mount Sinai Medical Center in New York, and a collaborator on the study A similar reversal of pathology has also been seen with enzyme replacement used to treat another lysosomal storage disease, Gaucher's disease.
"There is a pipeline of treatments that will soon become available for a variety of rare, lysosomal storage diseases," such as Niemann-Pick disease and Pompe's disease, Dr. Desnick said at a news conference at the meeting. The ability to treat these diseases effectively will place a new emphasis on early diagnosis, so that treatment can begin before irreversible pathology and sequelae occur, he added.
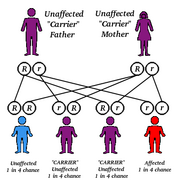
Early diagnosis of Fabry disease is challenging, Dr. Eng noted. It usually manifests first as pain in the hands and feet with no discernible cause. This symptom can be particularly suggestive if it occurs in two or more brothers (Fabry disease is X-linked, and so occurs overwhelmingly in males, although cases in females are possible). But the diagnosis is usually missed in childhood because the disease is so rare and therefore not near the top of a differential diagnosis list, she said.
As patients become teenagers and young adults, the pain becomes more intense, and can be accompanied by fever, rash in the genital region, and ocular findings. Damage to the skin, heart, and liver usually doesn't appear until the late 20s.
The second study that was reported at the meeting was an uncontrolled treatment trial with 26 patients. After 6 months of infusions every 2 weeks, all of the the patients had reductions in pain and in the glycolipid deposits in their vascular linings, reported Dr. Raphael Schiffmann, chief of the clinical investigation section in the developmental and metabolic neurology branch of the National Institute of Neurological Disorders and Stroke in Bethesda, Md.
Although both studies exclusively enrolled young adults who were at least 16 years old, tests for future treatment in children may eventually occur.
In both studies, the enzyme infusion was well tolerated, with no evidence of an allergic reaction to the infused protein.
COPYRIGHT 2001 International Medical News Group
COPYRIGHT 2001 Gale Group