The effect of norepinephrine administration on pulmonary blood flow during the neonatal period is unclear. Therefore, norepinephrine responses were studied in isolated pulmonary arteries, pulmonary veins, and femoral arteries taken from normal pigs from birth to adulthood and from pigs subjected to chronic hypoxia either from birth for 3 days or from 3 to 14 days of age. Normally, the contractile response of pulmonary arteries and veins to norepinephrine decreased after birth (p
Keywords: adrenoceptors; noradrenaline; pulmonary hypertension
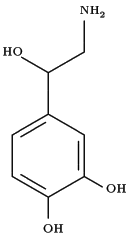
Evidence is accumulating to suggest that increased adrenergic activity may contribute to the pathogenesis of primary and secondary pulmonary hypertension in adults (1). Prolonged exposure to hypoxia increases the levels of circulating norepinephrine in adults (2). In cultured pulmonary arterial smooth muscle cells, hypoxia stimulates aradrenoceptors, which leads to increased smooth muscle contraction (3) and cell proliferation via stimulation of protein kinase C (4). In addition to upregulation of aradrenoceptors, hypoxia produces a concomitant downregulation of [beta]-adrenoceptor density on pulmonary vessels in adult rats (5), shifting the balance further in favor of vasoconstriction and smooth muscle proliferation. The role of the adrenergic system in the pathogenesis of persistent pulmonary hypertension of the newborn and pulmonary hypertension in childhood, if any, is unclear. Nevertheless, norepinephrine is widely used in clinical practice in both children and adults to induce systemic vasoconstriction, raise systemic vascular resistance, and thus elevate systemic arterial pressure (6).
The extent to which the use of norepinephrine compromises the pulmonary circulation is not clear. Hypothesizing that it could compromise the unstable pulmonary vasculature of sick newborns with persistent pulmonary hypertension of the newborn, we investigated the adrenergic responses of isolated pulmonary arteries and veins taken from chronically hypoxic pulmonary hypertensive newborn piglets. The study also entailed an assessment of the adrenergic responses in normal animals from fetal to adult life, about which little is known. We compared the responses in the pulmonary arteries with those in the femoral artery. A porcine model was used, as it has previously been shown to be a good model for the study of pulmonary adaptation to extrauterine life (7) and neonatal pulmonary hypertension (8). Some of the results of these studies have been previously reported in the form of an abstract (9).
METHODS
Pulmonary and femoral vessels were studied from a total of 62 large white pigs, which included fetal pigs (5 days preterm), 3- and 14-day-old animals, and adult pigs. To study the effect of pulmonary hypertension, newborn piglets were placed in a hypobaric chamber (50.8 kPa, FI^sub O^sub 2^^, 0.096) and cared for in an hypoxic environment for 3 days. A second group of 3-day-old piglets were placed in the hypobaric chamber for 11 days. The animals received humane care in compliance with the "Guide for the Care and use of Laboratory Animals," which is published by the National Institutes of Health (National Institutes of Health publication No. 80-23, revised 1996).
The animals were killed with an overdose of pentobarbital sodium, and the intralobar pulmonary arteries, pulmonary veins, and femoral arteries 1- to 2-mm diameter were dissected free and cut into rings 2-3 mm long. The rings were suspended in a 10-ml organ chamber, and isometric tension was measured as previously described (10). The organ chambers were filled with modified Krebs-Ringer solution and gassed with 95% O2-5% CO2 at 37°C. The rings were stretched to their optimum resting tension and contracted with potassium chloride 40 mM to assess their viability.
A cumulative dose-response curve to norepinephrine (10^sup -8^-10^sup -4^ M) was performed from baseline resting tension in the pulmonary arteries, veins, and femoral arteries from all animals. For comparison, a cumulative dose-response study was made in the pulmonary arteries using the thromboxane mimetic U46619 (10^sup -10^-10-^sup 5.5^ M).
The relaxant response to norepinephrine was assessed in the pulmonary arteries, veins, and femoral arteries by performing a norepinephrine cumulative dose-response curve after the baseline tone had been elevated to approximately 50% of the potassium chloride 40 mM contraction using U46619.
To determine the adrenoceptors involved in norepinephrine-induced contraction and relaxation, pulmonary artery, vein, and femoral artery rings were preincubated for 20 minutes with either Krebs-Ringer solution (control), prazosin 10^sup -7^ M, yohimbine 10^sup -7^ M, or propranolol 10^sup -5^ M, before performing the norepinephrine cumulative dose-response study from an elevated tension. Other rings were rubbed to remove the endothelium or N^sup W^-nitro-L-arginine methyl ester (L-NAME) 10^sup -4^ M was added before preconstricting them to determine whether the relaxation was due to release of nitric oxide by the endothelium. Maximum contractile and relaxant responses to the relevant antagonists were expressed as a percentage of the control maximum response.
The contractile response was expressed as developed tension (mg/mg tissue). The relaxation response was expressed as the percentage relaxation of the preconstricted tension induced by U46619. The effect of age and hypoxic pulmonary hypertension on norepinephrine-induced responses in the arteries and veins was determined using a general linear model with repeated measures. The effect of removal of the endothelium, the presence of L-NAME, and adrenoceptor blockers were analyzed using analysis of variance and where appropriate, Student's t test with Bonferroni's correction, comparing lest to control rings in each animal at the concentrations producing maximal response. Additional details on the methods and the results for potassium chloride are provided in an online supplement.
RESULTS
Responses to Norepinephrine in Normal Animals
The pulmonary arterial contractile response to norepinephrine showed a dose-dependent increase in tone in all the fetal animals, which was significantly greater than at all other ages (Table 1 and Figure 1). At 3 and 14 days of age, only 28% and 71% of rings, respectively, contracted to norepinephrine, and when a contractile response was seen in these and in the rings from adult animals, there was a dose-dependent increase in tone up to 10 µM (Figure 1). The norepinephrine concentration producing half-maximal contraction (EC^sub 50^) was unaffected by age (Table 1).
In contrast, the thromboxane analog U46619 produced a strong contractile response at all ages, the maximum tension generated being 4- to 90-fold greater than the norepinephrine response (Table 1).
A contractile response to norepinephrine was seen in the pulmonary veins in all age groups, which was maximal at 1 µM (Figure 1). The response was significantly greater in the fetal pulmonary veins compared with the 3 day old, 14 day old, and adult (Figure 1). Overall, as shown in Table 1, there was a twofold to threefold greater maximal contractile response to norepinephrine in the pulmonary veins than in the pulmonary arteries (p = 0.01).
In the femoral arteries, norepinephrine elicited a dose-dependent contractile response up to 10 µM (Figure 1), which was 15-fold to 40-fold greater than the pulmonary arterial response at all ages (p
A dose-dependent relaxant response to norepinephrine was present in all pulmonary arteries and veins except in the fetal pulmonary arteries, where no relaxant response was seen in 66% of vessels. For the pulmonary arteries, norepinephrine maximum relaxation responses were similar at 3 and 14 days old and in the adult, and all were significantly greater than the fetal relaxation responses (Figure 2). In contrast, a dose-dependent relaxation response was seen in the fetal pulmonary veins, and the magnitude of the response did not change significantly with age (Figure 2 and Table 2).
In the femoral artery, there was no relaxant response to norepinephrine in the fetal vessels, and a relaxant response was only seen at a norepinephrine concentration of 0.1 mM in vessels from the 3- and 14-day-old animals. The response was twofold to threefold less than that seen in the pulmonary arteries and veins (p
Effect of age on adrenoceptor subtypes. The [alpha]^sub 1^-adrenoceptor antagonist prazosin reduced the maximum pulmonary arterial norepinephrine contractile response to a much greater degree in vessels from the fetal pigs (98 ± 5%) than in vessels from 14-day-old (46 ± 4%) and adult animals (49 ± 9%) (p = 0.01; Table 3). In contrast, the [alpha]^sub 2^-adrenoceptor antagonist yohimbine significantly reduced the maximum pulmonary arterial norepinephrine contractile response in the 14-day (91 ± 8%) and adult (88 ± 6%) animals but did not change the contractile response of the 3-day or fetal pigs (p
A similar pattern of contractile and relaxant responses was seen in the pulmonary veins (Tables 3 and 4). Prazosin again had a greater inhibitory effect on norepinephrine-mediated contraction in the fetal veins as compared with its effect on veins from older animals (p = 0.001). In contrast, yohimbine reduced the norepinephrine-stimulated maximum contraction in the pulmonary veins by 85 ± 5% in the 14-day and 87 ± 9% in the adult animals but did not affect the responses of the fetal or 3-day-old vessels (p
The femoral arterial norepinephrine-stimulated contractile response in the fetal, 3-day-old, and 14-day-old animals was predominantly [alpha]^sub 1^-adrenoceptor mediated with a small contribution from the [alpha]^sub 2^-adrenoceptor (Table 3). Yohimbine had a significantly greater inhibitory effect on the norepinephrine-induced maximum contraction of the 14-day-old femoral arteries than on arteries from fetal animals (p = 0.01) (Table 3). The norepinephrine-induced femoral arterial relaxation was absent in the fetal animals and was completely inhibited by yohimbine in the 3- and 14-day-old animals (Table 4), implying that there is also a maturational increase in [alpha]^sub 2^-adrenoceptor-mediated responses in the femoral artery.
The relaxant response of the pulmonary arteries, veins, and femoral arteries was markedly attenuated after the addition of L-NAME and removal of the endothelium, suggesting that the relaxation was largely due to release of nitric oxide from the endothelium (Table 4).
The Effect of Hypoxic Pulmonary Hypertension on the Response to Norepinephrine
Compared with the 3-day-old normoxic control animals, the norepinephrine contractile response of the pulmonary arteries from animals exposed to hypoxia from birth to 3 days of age was significantly increased and approached values seen in the fetal animals (Table 1). In contrast, the contractile response after hypoxic exposure from 3 to 14 days was similar to that seen in the 14-day-old control subjects (Table 1). The pulmonary arterial contractile response to U46619 was unaffected by pulmonary hypertension but remained 4- to 90-fold greater than that seen to norepinephrine (Table 1). Pulmonary hypertension also had no effect on the norepinephrine-induced contractile response of either the pulmonary veins or the femoral arteries in either group of hypoxic animals. The femoral arterial contractile response to norepinephrine remained 30-60 times greater than the pulmonary arterial response (p
Pulmonary hypertension reduced the norepinephrine-induced maximum relaxant response of the pulmonary artery in both groups of hypoxic animals by 60-80% (p
Effect of hypoxia on adrenoceptor subtypes. Exposure to hypoxia from birth resulted in an increased [alpha]^sub 1^-adrenoceptor-mediated contractile response compared with the normal response at 3 days. Prazosin reduced the hypoxic norepinephrine-induced contractile response by 93 ± 5% compared with 68 ± 8% in the 3-day-old control subjects (p = 0.01) Table 3. In contrast, hypoxic exposure from 3-14 days did not significantly alter the aradrenoceptor contribution, but the [alpha]^sub 2^-adrenoceptor contribution to the contractile response was reduced when compared with the 14-day-old normoxic control subjects (p = 0.005) (Table 3).
After exposure to hypoxia from birth to 3 days of age, norepinephrine-induced relaxation was absent in the majority of pulmonary arteries and thus could not be studied. However, after exposure from 3-14 days of age, norepinephrine-mediated relaxation was present but impaired, and the normal development of [alpha]^sub 2^-adrenoceptor dilatation was inhibited in the pulmonary artery (Table 4). The [beta] adrenoceptor contribution to the relaxation, as assessed with propranolol, was similar in the 14-day hypoxic and control animals. The pulmonary arterial norepinephrine-induced relaxation of the 3- to 14-day hypoxic animals was attenuated significantly less by endothelial removal than that of the 14-day normoxic control animals (Table 4). Hypoxic pulmonary hypertension did not alter the effect of prazosin, yohimbine, or propranolol on the pulmonary veins or femoral arteries (Tables 3 and 4).
DISCUSSION
We have demonstrated in this animal model that there are changes in the response of conduit arteries to norepinephrine with age during normal adaptation to extrauterine life. In pulmonary hypertension, these normal changes are compromised. These observations may have implications for the development of persistent pulmonary hypertension of the newborn, although data from animal studies must always be extrapolated to humans with considerable caution. The similarities between the immature human and porcine lung are well documented (7), and the structural findings in the porcine model of neonatal pulmonary hypertension parallel those seen in the infant (8).
Effect of Age on the Response to Norepinephrine
In the vessels from normal animals, we documented an immediate postnatal reduction in the contractile response of pulmonary arteries and veins to norepinephrine and a postnatal increase in [alpha]^sub 2^-adrenoceptor-mediated relaxation in isolated porcine pulmonary arteries, veins, and femoral arteries. At all ages, the contractile response of the systemic arteries to norepinephrine was 15- to 60-fold greater than that of the pulmonary arteries.
The pulmonary arterial contractile response to norepinephrine, even in fetal life and after exposure to chronic hypoxia, was not great, particularly when compared with the response to the thromboxane mimetic U46619, which was 8- to 60-fold greater. These observations are in accord with those of McIntyre and colleagues (11), who also found that eicosanoid receptor stimulation of the pulmonary vascular smooth muscle of the rat with U46619 and prostaglandin F^sub 2[alpha]^ produced a greater maximal tension than aradrenoceptor stimulation. In isolated pulmonary arteries from human adults undergoing thoracic surgery, the maximum tension induced by U46619 and prostaglandin F^sub 2[alpha]^ was eightfold greater than that produced by norepinephrine and phenylephrine (12). Endothelin-1 also produced a 60% greater contractile response than norepinephrine in adult human pulmonary arteries (13). Neild and colleagues (14) examined resistance pulmonary arteries from lung biopsies of children with congenital heart disease and a high pulmonary blood flow and found that norepinephrine caused no constriction in concentrations up to 1 mM. Thus, the evidence for norepinephrine being a potent contractile stimulant in pulmonary arteries, even in pulmonary hypertension, is not strong.
In this study, the contractile response to norepinephrine decreased considerably between late fetal life and 3 days of age in normal pulmonary arteries and veins. Concomitant with this, there was a 12-fold increase in the pulmonary arterial relaxant response, suggesting that this mediator may have a role in the reduction of pulmonary vascular resistance after birth. Dunn and colleagues (15) noted a similar postnatal reduction in norepinephrine-stimulated contraction between the preterm and 1-day-old lamb but did not examine the relaxant response.
The predominant adrenoceptor subtype responsible for norepinephrine-mediated contraction in the pulmonary artery switched from the [alpha]^sub 1^ subtype in the fetus and 3-day-old animals to the [alpha]^sub 2^ subtype at 14 days. Similar changes were found in the pulmonary veins. In adult porcine intrapulmonary arteries (16) and in adult canine pulmonary veins (17), the norepinephrine contractile response was inhibited by both prazosin and yohimbine, suggesting a combined [alpha]^sub 1^ and [alpha]^sub 2^-adrenoceptor effect. Responses in young animals were not examined, and the norepinephrine-induced relaxation response in the porcine pulmonary arteries and veins was largely [beta]-adrenoceptor mediated in our normal 3-day-old animals and was both [beta] and [alpha]^sub 2^-adrenoceptor mediated in the 14-day-old and adult animals, again showing an increase in [alpha]^sub 2^-adrenoceptor activity with age. These observations confirm those of earlier investigators who found [alpha]^sub 2^-adrenoceptor-induced relaxation at approximately 3 months but not at 3 days of age in isolated porcine pulmonary arteries (18).
The small norepinephrine-induced relaxation response in the femoral arteries of our 3- and 14-day-old animals was [alpha]^sub 2^-adrenoceptor mediated. Similarly, in 10- to 200-day-old rats, the femoral artery relaxant response of norepinephrine was attributed to [alpha]^sub 2^-adrenoceptors (19). The [alpha]^sub 2^ contractile effect significantly increased with age, suggesting that there is a delay in the appearance of [alpha]^sub 2^-adrenoceptors in femoral arteries as well as in the pulmonary arteries.
Very little is known about the maturation of [alpha] adrenoceptors in the human lung. The small amount of mature adult human data is consistent with the data from our older pigs. In the adult human lung, the ratio of [alpha]^sub 1^/[beta] binding sites was 1:1 (20); however, [alpha]^sub 2^-adrenoceptors have not been studied in human pulmonary vasculature. In adult human skeletal muscle resistance arteries, norepinephrine produced a contractile response, which was predominantly mediated via [alpha]^sub 1^-adrenoceptors (21). However, the [alpha]^sub 2^-adrenoceptor also mediated a small contractile response (21), which is similar to the adrenoceptor responses seen in our porcine femoral arteries.
In our study, norepinephrine-stimulated pulmonary arterial relaxation was absent in the majority of fetal piglets. After birth, the norepinephrine-induced pulmonary arterial relaxation was largely mediated by nitric oxide release from the endothelium as the response was markedly reduced by removal of the endothelium and by the application of the nitric oxide synthase inhibitor L-NAME. Porcine endothelial nitric oxide synthase activity is extremely low in utero and increases dramatically immediately after birth, peaking at 14 days of age (22). This may help explain the dramatic increase in norepinephrine relaxation seen between birth and 3 days of age, in addition to adrenoceptor changes. The density of [beta] adrenoceptors also increases immediately after birth in newborn pigs (23).
Effect of Hypoxia-induced Pulmonary Hypertension on the Response to Norepinephrine
Exposure to hypoxia from birth for 3 days prevented the normal postnatal decrease in the contractile response of conduit arteries to norepinephrine, with an increased [alpha]^sub 1^-adrenoceptor contribution. The contractile response remained normal in those animals that had been subjected to hypoxic pulmonary hypertension after a period of normal adaptation, but the [alpha]^sub 2^-adrenorelaxation was delayed. In all animals, the contractile response of the femoral arteries remained normal and was consistently 15- to 60-fold greater than that seen in the pulmonary arteries. Sassa and colleagues (24) found that increasing the systemic mean arterial pressure by norepinephrine administration, in addition to high frequency ventilation, was beneficial in infants with persistent pulmonary hypertension of the newborn. Similarly, in anesthetized patients with chronic pulmonary hypertension, norepinephrine increased the systemic to pulmonary arterial pressure ratio without changing cardiac index (25). Thus, norepinephrine may to be a useful agent in the management of systemic hypotension in the presence of pulmonary hypertension, although further studies are required to determine whether the response of small resistance vessels is similar to that of the larger vessels used in this study.
Norepinephrine-induced pulmonary arterial relaxation was reduced in all animals exposed to chronic hypoxia, both from birth and from 3 days of age. Priest and colleagues (26) also noted depressed isoprenaline-stimulated vasorelaxation in chronically hypoxic rats, and Houde and colleagues (27) found that in children with primary or secondary pulmonary hypertension, salbutamol and phentolamine were ineffective in reducing pulmonary arterial pressure. Pulmonary arterial [beta] adrenoceptor relaxation was absent in our piglets exposed to hypoxia from birth for 3 days. Hypoxia from birth also attenuated the normal postnatal increase in pulmonary arterial [beta] adrenoceptor density (23). In children with congenital heart disease, platelet [alpha] adrenoceptor density was increased, and lymphocyte [beta] adrenoreceplor density was attenuated by 27% in patients with left to right shunts associated with pulmonary hypertension (28).
The impaired relaxant responses to noradrenaline in the pulmonary artery described in our study may be due to a combination of altered balance between different adrenoceptor populations and impaired nitric oxide release by the endothelium. In the pulmonary arteries of neonatal piglets, hypoxia-induced pulmonary hypertension is associated with disruptions at several points in the nitric oxide pathway (10, 29), whereas in porcine pulmonary vein (29) and rat aorta (30), the nitric oxide pathway appeared unaffected.
In conclusion, the norepinephrine contractile response was increased, and relaxation was impaired in the pulmonary arteries of the neonatal pulmonary hypertensive animals, findings similar to those seen in normal fetal vessels. The responses of the pulmonary veins and systemic femoral arteries were unaffected by pulmonary hypertension. [alpha]^sub 2^-Adrenoceptor activity increased with age in the pulmonary arteries and veins and in the femoral arteries. Norepinephrine-induced contraction was greater in the systemic arteries than pulmonary arteries in both normal and pulmonary hypertensive animals. These findings suggest that use of norepinephrine to manage systemic hypotension in infants and children should not significantly compromise the pulmonary vasculature.
References
1. Salvi SS. [alpha]1-Adrenergic hypothesis for pulmonary hypertension. Chest 1999;115:1708-1719.
2. Antezana AM, Kacimi R, LeTrong JL, Marchal M, Abousahl I, Dudray C, Richalet JP. Adrenergic status of humans during prolonged exposure to the altitude of 6,542 m. J Appl Physiol 1994;76:1055-1059.
3. Graham RM, Perez DM, Hwa J, Piascik MT. [alpha]1-Adrenergic sub-types: molecular structure, function and signalling. Circ Res 1996;78:737-749.
4. Dempsey EC, McMurtry IF, O'Brien RF. Protein kinase C activation allows pulmonary artery smooth muscle cells to proliferate to hypoxia. Am J Physiol 1991;260:L136-L145.
5. Jianming X, Quanfu X, Lirong W. Effect of hypoxia on the pulmonary [beta]- and [alpha]1-adrenoreceptors in rats. Chin Med Sci J 1991;6:217-222.
6. Ognibene FP. Hemodynamic support during sepsis. Clin Chest Med 1996; 17:279-287.
7. Haworth SG, Hislop AA. Adaptation of the pulmonary circulation to extra-uterine life in the pig and its relevance to the human infant. Cardiovasc Res 1981;15:108-119.
8. Haworth SG, Hislop AA. Effect of hypoxia on adaptation of the pulmonary circulation to extra-uterine life in the pig. Cardiovasc Res 1982; 16:293-303.
9. Schindler M, Hislop A, Haworth SG. The effect of norepinephrine on porcine pulmonary and systemic vasculature during pulmonary hypertension [abstract]. Pediatr Crit Care Med 2003;4:A148.
10. Tulloh RM, Hislop AA, Boels PJ, Deutsch J, Haworth SG. Chronic hypoxia inhibits postnatal maturation of porcine intrapulmonary artery relaxation. Am J Physiol 1997;272:H2436-H2445.
11. McIntyre RC Jr, Agrafojo J Banerjee A, Fullerton DA. Pulmonary vascular smooth muscle contraction. J Surg Res 1996;61:170-174.
12. Sjoberg T, Steen S. The strong contractile effect of the thromboxane receptor agonist U46619 in isolated human pulmonary arteries and its competitive antagonism by BM-13.505. Acta Physiol Scand 1989;136: 161-165.
13. Cases E, Vila JM, Medina P, Aldasora M, Segarra G, Lluch S. Increased responsiveness of human pulmonary arteries in patients with positive bronchodilator response. Br J Pharmacol 1996;119:1337-1340.
14. Neild TO, McLean JR, Mce RB. An in vitro study of the pharmacological and electrophysiological properties and the adrenergic innervation of small pulmonary arteries from children with pulmonary hypertension. Res Commun Chem Pathol Pharmacol 1986;53:265-268.
15. Dunn JA, Lorch V, Sinha SN. Responses of small intrapulmonary arteries to vasoactive compounds in the fetal and neonatal lamb: norepinephrine, epinephrine, serotonin, and potassium chloride. Pediatr Res 1989;25:360-363.
16. Tulloh RM, Dyamenhalli U, Stuart-Smith K, Haworth SG. Adrenoceptor-stimulated endothelium-dependent relaxation in porcine intrapulmonary arteries. Pulm Pharmacol 1994;7:299-303.
17. Ohlstein EH, Horohonich S, Shebuski RJ, Ruffolo RR Jr. Localisation and characterisation of alpha-2 adrenoceptors in the isolated canine pulmonary vein. J Pharmacol Exp Ther 1989;248:233-239.
18. Wilson LE, Levy M, Stuart-Smith K, Haworth SG. Postnatal adrenoceptor maturation in porcine intrapulmonary arteries. Pediatr Res 1993;34:591-595.
19. Nishina H, Ozaki T, Hanson MA, Poston L. Mechanisms of noradrenaline-induced vasorelaxation in isolated femoral arteries of the neonatal rat. Br J Pharmacol 1999;127:809-812.
20. Kondratenko TY, Zacharova IV, Kuzina NV, Katukov Vyu, Severin ES, Kornilova ZCh, Perelman MI. Alterations in human lung adrenergic receptors in cancer. Biochem Mol Biol Int 1993;29:123-130.
21. Jarajapu YP, Coats P, McGrath JC, MacDonald A, Hillier C. Increased alpha (1)- and alpha (2)-adrenoceptor-mediated contractile response of human skeletal muscle resistance arteries in chronic limb ischemia. Cardiovasc Res 2001;49:218-225.
22. Arrigoni FI, Hislop AA, Pollock JS, Haworth SG, Mitchell JA. Birth up-regulates nitric oxide synthase activity in the porcine lung. Life Sci 2002;70:1609-1620.
23. Hislop AA, Mak, JC Kelly D, Reader JA, Barnes PJ, Haworth SG. Postnatal changes in [beta]-adrenoceptors in the lung and the effect of hypoxia induced pulmonary hypertension of the newborn. Br J Pharmacol 2002;135:1415-1424.
24. Sassa S, Kribs A, Vierzig A, Roth B. A staged protocol for the treatment of persistent pulmonary hypertension of the newborn. Klin Padiatr 1997;209:301-307.
25. Kwak YL, Lee CS, Park YH, Hong YM. The effect of phenylephrine and norepinephrine in patients with chronic pulmonary hypertension. Anaesthesia 2002;57:9-14.
26. Priest RM, Robertson TP, Leach RM, Ward JP. Membrane dependent and independent vasodilation in small pulmonary arteries from chronically hypoxic rats. J Pharmacol Exp Ther 1998;285:975-982.
27. Houde C, Bohn DJ, Freedom RM, Rabinovitch M. Profile of paediatric patients with pulmonary hypertension judged by responsiveness to vasodilators. Br Heart J 1993;70:461-468.
28. Dzimiri N, Galal O, Moorji A, Bakr S, Abbag F, Fadley F, Almotrefi AA. Regulation of sympathetic activity in children with various congenital heart diseases. Pediatr Res 1995;38:55-60.
29. Berkenbosch JW, Baribeau J, Perreault T. Decreased synthesis and vasodilatation to nitric oxide in piglets with hypoxia-induced pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol 2000;278:L276-L283.
30. Shaul PW, Wells LB, Horning KM. Acute and prolonged hypoxia attenuate endothelial nitric oxide production in rat pulmonary arteries by different mechanisms. J Cardiovasc Pharmacol 1993;22:819-827.
Margrid B. Schindler, Alison A. Hislop, and Sheila G. Haworth
Vascular Biology and Pharmacology Unit, Institute of Child Health, London, United Kingdom
(Received in original form November 14, 2003; accepted in final form June 3, 2004)
Supported by the British Heart Foundation.
Correspondence and requests for reprints should be addressed to Sheila G. Haworth, M.D., Vascular Biology and Pharmacology Unit, Institute of Child Health, 30 Guilford Street, London WC1N 1EH, UK. E-mail: s.haworth@ich.ucl.ac.uk
This article has an online supplement, which is accessible from this issue's table of contents online at www.atsjournals.org
Am J Respir Crit Care Med Vol 170. pp 641-646, 2004
Originally Published in Press as DOI: 10.1164/rccm.200311-1551OC on June 7, 2004
Internet address: www.atsjournals.org
Conflict of Interest Statement: M.B.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this article; A.A.H. does not have a financial relationship with a commercial entity that has an interest in the subject of this article; S.G.H. does not have a financial relationship with a commercial entity that has an interest in the subject of this article.
Copyright American Thoracic Society Sep 15, 2004
Provided by ProQuest Information and Learning Company. All rights Reserved