Maintenance of an adequate BP, specifically mean arterial pressure (MAP), is essential for adequate tissue perfusion. When the MAP falls below the autoregulatory range of an organ, blood flow decreases in an almost linear fashion. Decreased blood flow results in tissue ischemia and organ failure. In patients with narrowing of their renal, coronary, or cerebral arteries, and in patients with long-standing hypertension, the fall in organ blood flow will occur at a higher BP. Furthermore, different vascular beds will lose autoregulation at different BP values. The autoregulatory threshold for the mammalian kidney is about 80 mm Hg, while that for the brain is approximately 50 mm Hg. An important goal in the management of critically ill patients is therefore to maintain the MAP above the autoregulatory threshold of the kidney, namely, 80 mm Hg. A higher threshold should be targeted in patients with a history of hypertension and in patients with atherosclerotic vascular disease. In patients who have experienced acute cerebrovascular insults, cerebral autoregulation may be lost, and in such circumstances blood flow is pressure-dependent. (1) In such patients, increasing the MAP beyond the cerebral autoregulatory range may improve tissue perfusion and decrease neuronal loss. (2,3)
Aggressive volume resuscitation is considered to be the best initial therapy for the management of patients with hypotension. Volume resuscitation is initiated with fluid boluses of 500 mL, titrated to BP (ie, MAP), heart rate, urine output, and respiratory status. In patients with the systemic inflammatory response syndrome due to sepsis or other causes, hypotension may persist despite vigorous volume expansion. These patients require treatment with a vasopressor agent. Traditionally, dopamine has been regarded as the pressor of choice as it was believed that this agent would maintain renal, cerebral, coronary, and splanchnic blood flow. Furthermore, it was taught that norepinephrine was to be avoided at all costs as this agent caused severe vasoconstriction. However, some data have suggested that both of these widely held "truths" are incorrect. The "reno-protective" effects of dopamine have been debunked, and this agent may paradoxically impair splanchnic mucosal blood flow. (4-7) At the same time, the deleterious effects of norepinephrine have not been confirmed, and indeed it has been demonstrated that this agent increases organ and tissue blood flow in patients in various disease states.
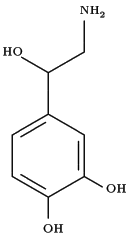
Although norepinephrine has been used in an animal model of ischemia-induced renal failure, intense vasoconstriction occurs only with infusion of the drug directly into the renal artery, and not via the systemic route at clinically relevant doses. (8-10) The dose of the drug used in animal models of norepinephrine-induced acute renal failure was two to three times that used in appropriate animal studies and was well beyond the mean dose usually administered in clinical practice. Indeed, as demonstrated by Albanese and colleagues in this issue of CHEST (see page 534), at clinically relevant doses (ie, renal dose norepinephrine) norepinephrine may improve renal function in patients with pathologic vasodilatation and maintain renal function in volume-replete patients who have normal systemic vascular resistance. Norepinephrine has been demonstrated to increase the expression of a cyclooxygenase (COX)-2 isoform in the kidney, and increased production of COX-2-derived prostaglandins (PGs) [ie, PG[E.sub.2] and PC[I.sub.2]] attenuates the renal vasoconstriction induced by uorepinephrine. (11-14) Furthermore, COX2-derived PGs may cause greater afferent arteriolar dilatation, thereby maintaining glomerular filtration. (13-15) In addition, an increase in systemic BP may lead to renal vasodilation by decreasing renal sympathetic tone through a baroreceptor feedback mechanism. (10)
Albanese and coworkers demonstrated that norepinephrine at a mean ([+ or -] SD) dose of up to 1.3 [+ or -] 0.3 [micro]g/kg/min restored the MAP and reestablished urine output in oligurie patients with septic shock. This finding has been observed by other investigators, (16-18) and was confirmed in experimental models of endotoxemia in which norepinephrine restored renal blood flow and renal function. (19-21) It should be appreciated that due to decreased adrenergic receptor density and receptor uncoupling in patients with sepsis, doses of up to 2.0 [micro]g/kg/min may be required to achieve an adequate MAP. (22) While the benefit of norepinephrine in patients with septic shock has been established, (23) the safety of this vasopressor in other clinical scenarios has been questioned. However, the study by Albanese and colleagues has demonstrated that in volume-replete patients with head injuries norepinephrine (in a doses of up to 0.5 [micro]g/kg/min) will reliably increase the MAP (and cerebral perfusion pressure) without compromising renal function. This observation has been confirmed by Morimatsu et al, (24) who demonstrated that norepinephrine maintained renal function in hypotensive patients after cardiac surgery.
Volume resuscitation remains the cornerstone of treatment for the hypotensive patient. In the hypovolemic patient, therapy with norepinephrine may seriously compromise renal function and should therefore be avoided. However, in the volume-replete patient, norepinephrine is the vasopressor of choice. Norepinephrine in clinically relevant doses is a friend of the kidney and not a foe! (25)
REFERENCES
(1) Lang EW, Lagopoulos J, Griffith J, et al. Cerebral vasomotor reactivity testing in head injury: the link between pressure aim flow. J Neurol Neurosurg Psychiatry 2003; 74:1953-1059
(2) Rordorf C, Koroshetz WJ, Ezzeddine MA, et al. A pilot study of drug induced hypertension for treatment of acute stroke. Neurology 2001; 56:1210-1213
(3) Marik PE, Varon J, Trask T. Management of head trauma. Chest 2002; 122:699-711
(4) Kellum JA, Decker JM. Use of dopamine in acute renal failure: a meta-analysis. Crit Care Med 2001; 29:1526-1531
(5) Marik PE. Low-dose dopamine: a systematic review. Intensive Care Med 2002; 28:877-883
(6) Segal JM, Phang PT, Walley KR. Low-dose dopamine hastens onset of gut ischemia in a porcine model of hemorrhagic shock. J Appl Physiol 1992; 73:1159-1164
(7) Marik PE, Mohedin M. The contrasting effects of dopamine and norepinephrine on systemic and splanchnic oxygen utilization in hyperdynamic sepsis. JAMA 1994; 272:1354-1357
(8) Cronin RE, Erickson AM, de Torrente A, et al. Norepinephrine-induced acute renal failure: a reversible ischemic model of acute renal failure. Kidney Int 1978; 14:187-199
(9) Cronin RE, de Torrente A, Miller PD, et al. Pathogenic mechanisms in early norepinephrine-induced acute renal failure: functional and histological correlates of protection. Kidney Int 1978; 14:115-125
(10) Anderson WP, Korner PI, Selig SE. Mechanisms involved in the renal responses to intravenous and renal artery infusions of noradrenaline in conscious dogs. J Physiol 1981; 321:21-30
(11) Llinas MT, Lopez R, Rodriguez F, et al. Role of COX-2derived metabolites in regulation of the renal hemodynamic response to norepinephrine. Am J Physiol 2001; 281:F975-F982
(12) Chatziantoniou C, Arendshorst WJ. Prostaglandin interactions with angiotensin, norepinephrine, and thromboxane in rat renal vasculature. Am J Physiol 1992; 262:F68-F76
(13) Imig JD, Deichmann PC. Afferent arteriolar responses to ANG 11 involve activation of PLA2 and modulation by lipoxygenase and P-450 pathways. Am J Physiol 1997; 273: F274 -F282
(14) Pelayo JC. Renal adrenergic effector mechanisms: glomerular sites for prostaglandin interaction. Am J Physiol 1988; 254: F184-F190
(15) Inscho EW, Carmines PK, Navar LG. Prostaglandin influences on afferent arteriolar responses to vasoconstriclor agonists. Am J Physiol 1990; 259:F157-F163
(16) Desjars P. Pinaud M, Bugnon D, et al. Norepinephrine therapy has no deleterious renal effects in human septic shock. Crit Care Med 1989; 17:426-429
(17) Martin C, Papazian L, Perrin C, et al. Norepinephrine or dopamine for the treatment of hyperdynamic septic shock? Chest 1993; 103:1826-1831
(18) Ledoux D, Astiz M, Carpati CM, et al. Effects of perfusion pressure on tissue perfusion in septic shock. Crit Care Med 2000; 28:2729-2732
(19) Di Giantomasso D, Morimatsu H, May CN, et al. Intrarenal blood flow distribution in hyperdynamic septic shock: effect of norepinephrine. Crit Care Med 2003; 31:2509-2513
(20) Zhang H, Smail N, Cabral A, et al. Effects of norepinephrine on regional blood flow and oxygen extraction capabilities during endotoxic shock. Am J Respir Crit Care Med 1997; 155:537-544
(21) Treggiari MM, Romand JA, Burgener D, et al. Effect of increasing norepinephrine dosage on regional blood flow in a porcine model of endotoxin shock. Crit Care Med 2002: 30:1334 -1339
(22) Boillot A, Massol J, Maupoil V, et al. Myocardial and vascular adrenergic alterations in a rat model of endotoxin shock: reversal by an anti-tumor necrosis factor-alpha monoclonal antibody. Crit Care Med 1997; 25:504-511
(23) Martin C, Viviand X, Leone M, et al. Effect of norepinephdoe on the outcome of septic shock. Crit Care Med 2000; 28:2758-2765
(24) Morimatsu H, Uchino S, Chung J, et al. Norepinephrine for hypotensive vasodilatation after cardiac surgery: impact on renal function. Intensive Care Med 2003; 29:1106-1112
(25) Bellomo R, Di Giantomasso D. Noradrenaline and the kidney: friends or foes? Crit Care 2001:5:293-298
Paul E. Marik, MD, MBBCh, FCCP Pittsburgh, PA
Dr. Marik is affiliated with the Department of Critical Care Medicine, University of Pittsburgh Medical Center. Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Paul Marik, MD, MBBCh, FCCP, Professor of Critical Care and Medicine, Department of Critical Care, University of Pittsburgh, 640A Scaife Hall, 3550 Terrace St, Pittsburgh, PA, 15261; e-mail: maripe@ccm.upmc.edu
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group