In this issue, Boyle et all demonstrate that commercially available antibodies against tyrosinase and glycoprotein 100 (gp100) can serve as excellent immunocytochemical tools for the diagnosis of melanoma in its different variants. Using an antigen retrieval technique and antibodies T311 and HMB-45, they found corresponding immunoreactivities in all of their tested samples of melanoma, which included melanotic (6 cases), amelanotic (4 cases), and desmoplastic (5 cases) variants. They also found positivity for gp100 in 1 of 10 cases of schwannoma and positivity for tyrosinase in 1 of 10 cases of schwannoma and 4 of 8 cases of neurofibroma. These latter findings are not unexpected since, like melanocytes, these tumors contain cells of neural crest origin and thus are potentially capable of random derepression of markers of the melanocytic phenotype. The detection of gp100 antigen in desmoplastic melanomas is however surprising because this melanoma type, although positive for S100, is generally negative for HMB-45 when tested with standard immunocytochemistry techniques.2 The absence of staining observed in properly matched controls and in unrelated tumors indeed confirms the high specificity of these antibodies. Thus, based on the data presented, an appropriate conclusion would be that tyrosinase and gp100 may eventually serve as powerful (superior) immunocytochemical markers in the diagnosis of amelanotic and desmoplastic melanomas, provided that proper fixation and antigen retrieval techniques are applied.
Tyrosinase and gp100 are melanogenesis-related proteins (MRPs) that represent recent diagnostic and therapeutic additions to the pathology arsenal.3,4 Melanogenesis-related proteins are involved in the regulation of melanogenesis, the main function of the melanocyte.3-5 The structure, function, and molecular biology of these proteins have been extensively investigated by experts in the fields of pigment cell biology and human genetics, and their main characteristics are summarized in the Tables To provide better insight into MRPs and the melanogenic pathway, I will review current concepts in this area briefly and address the implications pertinent to diagnostic pathology.
MELANOGENESIS
It has been historically accepted that melanin synthesis starts with the hydroxylation of L-tyrosine to L-dihydroxyphenylalanine (L-DOPA). This hydroxylation is the limiting step of the pathway catalyzed by tyrosinase (Enzyme Commission of the International Union of Biochemistry designation EC 1.14.18.1); this step is followed by a series of oxidation and reduction reactions to yield the pigment melanin.5 L-DOPA, the product of L-tyrosine hydroxylation, serves as a precursor of catecholamines in addition to serving as a precursor of the eumelanin and pheomelanin pigments. Depending on an individual's genotype and the cellular environment, melanogenesis generates the black pigment eumelanin (eumelanogenesis), the reddish to yellow pigment pheomelanin (pheomelanogenesis), or a mixture that contains both components.5,6 The step common to the eumelanogenic and pheomelanogenic pathways is the oxidation of DOPA to dopaquinone.6 Eumelanogenesis proceeds from the transformation of dopaquinone to leukodopachrome, followed by oxidoreduction reactions catalyzed by post-DOPA oxidase regulators.7 Pheomelanin synthesis begins with the conjugation of dopaquinone to cysteine or glutathione to yield cysteinyldopa and glutathionyldopa, which are progressively transformed through a series of chemical reactions into the pheomelanin product.6 Melanogenesis intermediate products can also escape the melanocyte and enter the extracellular environment and systemic circulation; there they may serve as serum markers for melanogenic activity, for melanotic melanoma progression, or for melanoma recurrence.3,4
MELANOGENESIS-RELATED PROTEINS
The structural proteins involved in the formation of melanosomes together with the enzymes involved in the transformation of L-tyrosine to melanin are collectively called MRPs. Among the MRPs, those currently considered as better targets for use in diagnostic pathology are described subsequently, and their functions and chromosomal locations are summarized in the Table.
Tyrosinase
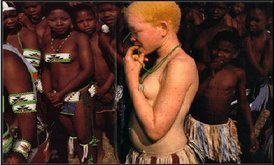
Tyrosinase is encoded by a gene at the c-locus that maps to chromosome 11q14-q21 in humans and chromosome 7 in mice.5 The tyrosinase gene contains 5 exons that after transcription generate several alternatively spliced products, of which only one expresses tyrosinase activity.5 It has been suggested that alternatively spliced tyrosinase messenger RNA (mRNA) species could possibly serve as receptors for L-tyrosine and LDOPA and, therefore, participate in the regulation of melanocytes function.8 The tyrosinase gene and protein are predominantly expressed in cells of melanocytic lineage.5 Mutation in the tyrosinase gene leading to defective (catalytically inactive) tyrosinase or a lack of this protein results in type 1 oculocutaneous albinism (OCA1) (see the Albinism Database9).
Newly synthesized tyrosinase has a molecular weight (MW) of 58 kD. Tyrosinase contains a cytoplasmic (C) terminal, a transmembrane segment, and an N terminal domain. The latter comprises the signal peptide, a cysteine-rich region, an epidermal growth factor-like domain, and 2 copper-binding domains.5 The N terminal signal peptide is critical for intracellular trafficking and processing, whereas the transmembrane region and cytoplasmic tail are necessary for targeting the enzyme to the melanosome.5,10 Glycosylation processes taking place in the Golgi complex increase the tyrosinase size to 65 to 72 kD.5,10 Proteolytic cleavage of the transmembrane portion of the newly synthesized enzyme generates 2 soluble molecular forms, 1 unmodified with a 53-kD MW, and 1 glycosylated tyrosinase with a 65-kD MW, and probably active in the melanosome. Tyrosinase forms of reportedly higher MWs may represent either dimers or tight complexes with other melanogenic proteins or differential processing of the protein.5,8 Catalytically active tyrosinase participates in 3 distinct reactions in the melanogenic pathway: hydroxylation of monophenol (L-tyrosine), dehydrogenation of catechol (L-DOPA), and dehydrogenation of dihydroxyindole (DHI); L-DOPA serves as cofactor in the first of these 3 reactions.5-7 In addition to direct involvement in the chemistry of the pathway, tyrosinase also acts as in situ regulator of the local availability of these biologically active molecules, conferring hormonelike properties to L-tyrosine and L-DOPA.8,11
Tyrosinase is also classified as a major histocompatibility complex (MHC) class I- and II-restricted tumor antigen and thus represents a potential target for the response of T lymphocytes against melanoma cells.12,13 In this context, tyrosinase expression in relation to specific human haplotypes could be used to guide immunotherapeutic approaches.3,4
HMB-45/gp100 Protein
The HMB-45/gp100 protein, a product of the SILV gene locus, is a membrane-bound melanosomal protein that acts as an enzymatic regulator of melanogenesis. The human SILV gene maps to chromosome 12q12-q13 and is homologous to the silver locus in mice; it consists of 11 exons and 10 introns spanning 9.1 kilobase (kb).5,14 Translation of the alternatively spliced SILV mRNA generates potentially malignant epithelial lesion 17 (PMEL17) and gp100 proteins. PMEL17 is a 668-amino acid protein with a potential signal peptide and a single transmembrane domain near the C terminal.5,14 The gp100 protein is a 661-amino acid protein with an approximately 100kD MW; gp100 differs from PMEL17 by the presence of one substitution (P274L) and deletion of a heptapeptide (588VGILLT594) located before the transmembrane domain.3,14 Both glycoproteins, PMEL17 and gp100, are recognized by the HMB-45 monoclonal antibody and are associated with the melanosomal membrane; they also share the ExxPLL motif (proposed as a melanosomal targeting signal) and cysteine- and histidine-rich regions.5,10 The functional role of gp100 and PMEL17 is still unclear, although these proteins may act as a scaffold in melanosomes, serving as a matrix for deposition of melanin; as stabilizers of melanin intermediates; or as catalysts for the polymerization of 5,6-dihydroxyindole-2-carboxylic acid (DHICA) to melanin.5,14 The gp100 and PMEL17 mRNAs are expressed in many tissues; expression of the corresponding proteins is however restricted to normal and malignant melanocytes, indicating tight translational regulation.5,14 Of potential therapeutic significance is the antigenic property of gp100 and PMEL17: these proteins are recognized by T lymphocytes.3,4,12,13
Tyrosinase-Related Proteins
Two additional tyrosinase-related proteins (TRPs) stimulate the eumelanin synthetic rate; they are TRP-1 (gp75, Melan-A or -B locu protein) and TRP-2 (a homolog of the slaty locus in mice). These proteins are cysteine rich and membrane bound, with 2 copper-binding sites, and they have approximately 40% amino acid homology with tyrosinase.5 The gene for TRP-1 is 15 to 18 kb long, contains 8 exons separated by 7 introns, and is located on chromosome 9.5 In the mouse, TRP-1 acts as a DHICA oxidase, generating indole-5,6-quinonecarboxylic acid, a reaction that may not be catalyzed by TRP-1 in humans., TRP-1 activity appears to be important for eumelanogenesis but not for pheomelanogenesis. The gene for TRP-2 contains 8 exons and is located on chromosome 13.5 TRP-2 acts as dopachrome tautomerase (EC 5.3.2.3), catalyzing the transformation of dopachrome to DHICA.5 It is noteworthy that TRPs contain sequences homologous to epidermal growth factor and that they can form multimeric complexes of 200 to 700 kD.5 These properties suggest an additional role for TRPs as regulators of melanocyte function, in addition to their mechanistic action as enzymes.8,11 During differentiation of neural crest cells toward the melanocytic lineage or during hair cycle melanoblastic differentiation to fully pigmented melanocytes, the expression of TRPs precedes that of tyrosinase.5,15 This sequence suggests a probable broader diagnostic utility for TRP-1 and -2 than for tyrosinase.
COMMENT
The paper by Boyle et all provides an additional argument for the use of melanogenic enzymes as legitimate diagnostic tools (with high specificity and sensitivity) for the diagnosis of amelanotic melanomas of even the desmoplastic type. Since tyrosinase, TRP-1, TRP-2, gp100, and melanosome-specific MART-1 are also classified as MHC class I-restricted tumor antigens (or MHC class I- and II-restricted tumor antigens in the case of tyrosinase), the usefulness of their detection may well extend beyond diagnosis and into the realms of therapy. This application would involve the generation of specific peptides to activate a T lymphocyte response against melanoma cells. Such a T-cell immune response may however be highly variable because peptides derived from MRPs can be recognized by T cells in association with specific haplotypes including human leukocyte antigen (HLA)-A2, HLA-A24, HLA-1344, HLA-A1, HLADR4, and HLA-DR15.3,4,12,13 Detection of MRPs can undoubtedly provide useful information for the classification of such an undifferentiated tumor as melanoma. Moreover, characterization of the expression of MRPs in relation to specific human haplotypes could also become a potential guide for immunotherapy.
References
1. Boyle JL, Haupt HM, Stern JB, Multhaupt HAB. Tyrosinase expression in malignant melanoma, desmoplastic melanoma, and peripheral nerve tumors: an immunohistochemical study. Arch Pathol Lab Med. 2002;126:816-822.
2. Carlson JA, Dickersin GR, Sober Aj, Barnhill RL. Desmoplastic neurotropic melanoma: a clini
copathologic analysis of 28 cases. Cancer. 1995;7: 478-494.
3. Slominski A, Carlson A, Wortsman J, Mihm M. The role of molecular biology in diagnostic pathology of melanoma. Methods Mol Med. 2001;61: 123-163.
4. Slominski A, Wortsman J, Carlson A, Matsuoka LY, Balch CM, Mihm M. Malignant melanoma: an update. Arch Pathol Lab Med. 2001;125:12951306.
5. Nordlund J), Boissy RE, Hearing VJ, King L, Ortonne JP, eds. The Pigmentary System: Physiology and Pathophysiology. New York, NY: Oxford University Press; 1998.
6. Prota G, ed. Melanins and Melanogenesis. New York, NY: Academic Press; 1992.
7. Pawelek J. After dopachrome? Pigment Cell Res. 1991;4:53-62.
8. Slominski A, Paus R. Towards defining receptors for L-tyrosine and L-DOPA. Mol Cell Endocrinol. 1994;99:C7-Cl 1.
9. Albinism Database [database online]. Twin Cities, Minn: International Albinism Center, University of Minnesota; 2002. Available at: http:// www.cbc.umn.edu/tad. Accessed February 2002.
10. jimbow K, Park JS, Kato F, et al. Assembly, target-signaling and the intracellular transport of tyrosinase gene family proteins in the initial stages of melanosome biogenesis. Pigment Cell Res. 2000;13: 222-229.
11. Slominski A, Paus R, Schanderdorf D. Melanocytes as sensory and regulatory cells in the epidermis. j Theor Biol. 1993;164:103-120.
12. Sakai C, Kawakami Y, Law LW, Furumura M, Hearing VJ. Melanosomal proteins as melanomaspecific immune targets. Melanoma Res. 1997;7: 83-95.
13. Smith C, Cerundolo V. Immunotherapy of melanoma. Immunology. 2001;104:1-7.
14. Solano F, Martinez-Esparza M, Jimenez-Cervantes C, et al. New insights on the structure of the mouse silver locus and on the function of silver protein. Pigment Cell Res. 2000;13(suppl 8):118-124.
15. Tobin DJ, Slominski A, Botchkarev V, Paus R. The fate of hair follicle melanocytes during the hair growth cycle. J Invest Dermatol Symp Proc. 1999;4: 323-332.
Andrzej Slominski, MD, PhD
Accepted for publication March 6, 2002.
From the Department of Pathology, University of Tennessee Health Science Center, Memphis, Tenn.
Reprints: Andrzej Slominski, MD, PhD, Department of Pathology, 576 BMH, University of Tennessee Health Science Center, 899 Madison Ave, Memphis, TN 38163 (e-mail: aslominski@utmem.edu).
Copyright College of American Pathologists Jul 2002
Provided by ProQuest Information and Learning Company. All rights Reserved