New data have become available since the publication in 1990 of my article, "Controversies in the Management of Hypertension."[1] These new data have helped clarify the approach to the management of hypertension, a disease that accounts for more visits to physicians than any other chronic illness. The fifth Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure (JNC V)[2] has published a report updating the results of the clinical trials and suggesting a somewhat different approach to management of hypertension than had been suggested in the 1988 JNC report,[3] and studies have expanded the indications for treatment of less severe degrees of hypertension.[4]
In parts I and II of this article, I discuss some ongoing controversies regarding the importance of systolic blood pressure, "white coat" hypertension, the choice of initial therapy, whether or not calcium channel blockers should continue to be used in treatment, some newer therapies and recent data on treatment results.
Importance of Systolic Blood Pressure
For years, physicians were taught that an elevated diastolic blood pressure was of greater significance than an increased systolic pressure in determining the patient's risk of cardiovascular disease. It was accepted by many physicians that a normal systolic blood pressure could be represented by 100 mm Hg plus age (i.e., a systolic pressure of 170 mm Hg in a person 70 years of age would be considered to be within normal limits).
Recent data, however, have confirmed what many investigators had suggested for years--that an elevated systolic blood pressure has as great as or greater importance than the diastolic pressure in estimating cardiovascular risk. These conclusions are based on a follow-up study of more than 300,000 men in the Multiple Risk Factor Intervention Trial (MRFIT),[5] as well as data from the Framingham Heart Study.[6]
As can be seen in Figure 1, a systolic blood pressure of 140 to 149 mm Hg confers a greater risk for cardiovascular events than a diastolic pressure of 90 to 94 mm Hg; a systolic pressure of 150 to 159 mm Hg confers a greater risk than a diastolic pressure of 95 to 100 mm Hg. Even borderline isolated systolic hypertension, defined as 140 to 159/less than 90 mm Hg, increases the risk at any age, not only in the elderly (Table 1).[6]
[TABULAR DATA OMITTED]
Recognizing the importance of these data, the JNC V redefined levels of hypertension to include systolic pressure in its new definitions. Hypertension is now defined on the basis of both elevated diastolic pressures of 90 mm Hg or above and systolic pressures of 140 mm Hg or above (Table 2).[2] Levels of severity are now defined in stages rather than as mild, moderate or severe. Although defining blood pressures of 130 to 139/85 to 89 mm Hg as "high normal" in the new classification might concern some persons and lead to unnecessary anxiety in patients, this new definition at a lower level of systolic pressure was put forth to suggest the importance of follow-up, especially in patients with other risk factors for heart disease (e.g., smokers and patients with hyperlipidemia, obesity and diabetes).
[TABULAR DATA 2 OMITTED]
At present, little evidence substantiates the concept that there is a level below which the risk of coronary heart disease events begins to increase. Unless blood pressure is lowered acutely in some patients with heart disease, there is little danger in reducing blood pressure from levels of 170 to 180 mm Hg systolic and 100 to 110 mm Hg diastolic, to, for example, 120 to 125 mm Hg systolic and about 80 mm Hg diastolic, provided the patient remains asymptomatic.
'White Coat' Hypertension
The issue of "white coat" hypertension also continues to be controversial. There is little doubt that certain patients experience elevated blood pressure in a physician's office, while their blood pressure at home or at work is considerably lower. Several investigators suggest that 24-hour blood pressure readings will distinguish those patients with "true" hypertension from patients with white coat hypertension, and that as many as 20 percent of patients with elevated pressure in the office but normal pressure at home will undergo unnecessary treatment.[7] It should be noted, however, that the blood pressure data on which estimates of cardiovascular risk are based are casual blood pressure readings taken in a clinic or office and that the data on benefit are also based on casual or office blood pressures.[8] In the clinical trials, for example, blood pressures were taken only three to four times a year in a clinic or office. Patients with lower pressures had fewer cardiovascular events.[9]
At present, data in the literature are conflicting on the importance of white coat hypertension. Some studies have suggested that patients with this syndrome (i.e., normal pressures at home and elevated pressures in the office) have physiologic changes indicative of hypertension, such as an increase in peripheral resistance and early diastolic dysfunction.[10] In addition, certain metabolic changes that are frequently seen in hypertensive patients are already present, such as increased insulin resistance and elevated lipid levels.
Based on available data, I believe that office blood pressure readings should still be considered the appropriate basis for estimating prognosis or determining effects of treatment. If some patients insist on knowing their blood pressures between visits, experience side effects from treatment or appear to be unusually resistant to therapy, the use of a home blood pressure machine over time is preferred over one 24- or 48-hour recording; not only does this method provide more ongoing data, it is considerably less expensive than ambulatory blood pressure monitoring.[8]
Benefits of Therapy--New Trials
In the past six years, several long-term treatment trials have provided additional data regarding benefits of treatment for hypertension. Studies have confirmed that effective treatment of hypertension with diuretics, either as monotherapy or in combination with a beta blocker, methyldopa (Aldomet), reserpine or clonidine (Catapres) or, in some instances, beta blockers as monotherapy, decreases the incidence of progression to severe disease and helps prevent left ventricular hypertrophy and congestive heart failure.[11]
In the clinical trials, only 95 of 13,389 patients in the treated groups progressed to severe hypertension, with diastohlic pressures above 110 mm Hg and systolic pressures above 200 mm Hg, compared with 1,493 of 13,342 patients in the control or placebo groups (Table 3).[12-17] In addition, only 140 of 6,150 subjects in the treated groups developed left ventricular hypertrophy, compared with 216 of 6,098 in the control or placebo groups. Only 112 of 6,914 subjects in the treated groups developed congestive heart failure, compared with 240 of 6,923 in the control groups (Table 4).[12-15,18-25] These data provide excellent examples of secondary prevention of left ventricular hypertrophy and congestive heart failure through early treatment of hypertension.
[TABULAR DATA 3 OMITTED]
The clinical trials in patients 65 years of age and older demonstrated a more significant decrease in strokes and stroke deaths (25 to 47 percent) and overall cardiovascular mortality (17 to 40 percent) than trials in younger subjects. Thus, speculation that the treatment of hypertension with diuretics and/or beta blockers does not reduce coronary heart disease events has been refuted by good scientific data. None of these long-term studies employed angiotensin-converting enzyme (ACE) inhibitors or calcium channel blockers, since these drugs were not available when the trials began.
Several trials are presently under way, to test the hypothesis that the newer drugs will result in as great a decrease in morbidity and mortality as the older agents.
Why JNC V Suggests Diuretics or Beta Blockers as Preferred Initial Therapy
The results of both the newer and older clinical trials formed the basis for the recommendation of the JNC V that diuretics and beta blockers be considered as preferred initial therapy.[2] Other drugs were suggested as alternative therapies. This decision was made not because ACE inhibitors and calcium channel blockers do not effectively lower blood pressure but because of the lack of data on morbidity and mortality outcome with the latter drugs.
Importance of Adverse Metabolic Effects of Diuretics and Beta Blockers
EFFECTS ON LIPIDS
A careful review of additional studies regarding the potentially adverse effects of diuretics and/or beta blockers on lipids and glucose metabolism indicate that, although there may be a 5 to 7 percent short-term increase in total cholesterol levels with the use of high-dose diuretics, this effect is no longer evident in most patients after one year.[27-30] None of the longer-term trials report a more than minimal increase m cholesterol levels; most report a decrease.
Two recent double-blind, placebo-controlled studies, the Treatment of Mild Hypertension Study (TOMHS),[4] 4.4 years of follow-up, and the Veterans Affairs trial,[31] 2.0 years of follow-up, which compared different classes of drugs (beta blockers, ACE inhibitors, diuretics, alpha blockers, centrally acting agents and calcium channel blockers), have also reported that the use of diuretics does not increase lipid levels.
Follow-up studies from the Hypertension Detection and Follow-up Program[9] show that patients with hyperlipidemia who are treated with diuretics experienced a decrease and not an increase in cholesterol levels at the end of the five-year study In addition, new data from the SHEP study (Table 5),[19] which used diuretics as initial therapy and added beta blockers if necessary, demonstrate that strokes and coronary heart disease events are decreased to an equal degree in subjects with low, medium and high cholesterol levels.
[TABULAR DATA 5 OMITTED]
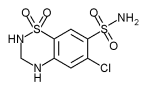
Thus, although there may be a concern about the potential adverse effect of diuretics on lipid metabolism, it appears to be a relatively short-term effect of little clinical significance. In addition, many of the older trials used higher diuretic dosages than the dosages recommended by the JNC V. This committee suggests, for example, that diuretic dosage be started at 12.5 to 25 mg of hydrochlorothiazide (Esidrix, Hydrodiuril, Oretic), chlorthalidone (Thalitone, Hygroton) or their equivalent, and that dosages be increased only to a maximum of 50 mg. At these lower dosages, the effects on lipid metabolism will be even less pronounced. From my experience, I prefer to increase the dosage to only 25 mg and then add a low dosage of a second drug (such as a beta blocker or an ACE inhibitor), rather than increase the diuretic dosage to the maximum recommended level.
While most of the beta blockers (without intrinsic sympathomimetic activity, thus with less effect on heart rate) elevate triglycerides and lower high-density lipoprotein (HDL) levels, these effects may also be of limited clinical importance. Recurrent infarctions and mortality are reduced when beta blockers are used.[32]
EFFECTS ON GLUCOSE METABOLISM
In the past five to six years, additional data have been published on the effect of diuretics and beta blockers on glucose metabolism. These data indicate that insulin resistance is increased in many hypertensive patients when compared with normotensive persons, even before therapy is given. Diuretics may increase insulin resistance still further.[33] Several investigators have suggested that diuretics not be used in patients with overt diabetes or a family history of diabetes, or those who are markedly obese; in these patients, insulin resistance may be increased to a greater degree.
However, a review of the diuretic-based clinical trials, including recent trials in the elderly,[17,19,20] and placebo-controlled studies comparing diuretics with other agents, revealed little evidence of an increase in serum glucose levels or new-onset diabetes or hyperglycemia greater than about 1 percent[34] (Table 6).[4,5,9,15,16,19,21,31,35,] In addition, a case-control study of more than 11,000 hypertensive patients treated with various antihypertensive drugs reported that the number of patients who became hyperglycemic and required antidiabetic therapy was similar with diuretics, beta-adrenergic inhibitors, calcium channel blockers, ACE inhibitors and alpha blockers.[36] Although there are some problems with data from any case-control study, these findings appear consistent with other observations. Recent unpublished but reported data from the SHEP study also show that the reduction in overall mortality from coronary heart disease and cerebrovascular disease in diabetic subjects treated with low-dose diuretics is as great or greater as that in nondiabetic patients.
[TABULAR DATA 6 OMITTED]
Thus, the earlier concerns about the long-term clinical effects of diuretics on glucose metabolism[37] may have been overemphasized. A recent study[38] suggests that diuretic-mediated insulin resistance and cholesterol level increases persist for as long as two years after the institution of diuretic therapy. But this aspect of the study included only 10 patients and, although statistical significance between diuretic and nondiuretic treatment groups was noted at one year, the difference was not significant at the end of two years.
Based on the available evidence on morbidity and mortality, physicians should probably not be concerned about using diuretics, especially in small dosages, in hypertensive patients with hyperlipidemia or diabetes. Chemical parameters should be monitored several times during the first year of treatment to detect the few people in whom changes might develop.
JNC V also considered possible adverse effects of beta-adrenergic inhibitors on glucose
metabolism. These agents may decrease insulin release, mask some of the symptoms of hypoglycemia, such as tachycardia, and delay recovery from hypoglycemia. They should therefore be used with care in patients with type 1, insulin-dependent, diabetes but can be used, if necessary, in patients with type II, non-insulin-dependent, diabetes or in patients with ischemic heart disease to lower blood pressure. In the MRC study in the elderly,[17] beta-blocker therapy did not prove as effective in reducing coronary heart disease events as diuretic therapy, but an earlier MRC study in younger patients[16] demonstrated that beta blockers were more effective in reducing coronary heart disease events.
After considering potential problems and the overall results of treatment with these two classes of drugs, the JNC V suggested that diuretics and beta blockers be preferred initial therapy--primarily because they are the only classes of drugs that have been tested in hypertensive patients and proved to reduce morbidity and mortality. Diuretics appear to be even more effective in reducing cardiovascular events than beta blockers. It should be noted that the use of beta blockers has been shown to reduce subsequent coronary heart disease morbidity and mortality in patients with ischemic heart disease.[32]
Figure I adapted from Kannel WB, Neaton JD, Wentworth D, Thomas HE, Stamler J, Hulley SB, et al. Overall and coronary heart disease mortality rates in relation to major risk factors in 325,348 men screened for the MRFIT. Multiple Risk Factor Intervention Trial. Am Heart J 1986;11 2(4):825-36.
REFERENCES
[1.] Moser M. Controversies in the management of hypertension. Am Fam Physician 1990;41:1449 [2.] The fifth report of the joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V). Arch Intern Med 1993;153:154-83. [3.] The 1988 report of the joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC IV). Arch Intern Med 1988;148:1023-38. [4.] Neaton JD, Grimm RH Jr, Prineas RJ, Stamler J, Grandits GA, Elmer PJ, et al. Treatment of Mild Hypertension Study. Final results. JAMA 1993;270: 713-24. [5.] Rutan GH, Kuller LH, Neaton JD, Wentworth DN, McDonald RH, Smith WM. Mortality associated with diastolic hypertension and isolated systolic hypertension among men screened for the Multiple Risk Factor Intervention Trial. Circulation 1988;77:504-14. [6.] Sagie A, Larson MG, Levy D. The natural history of borderline isolated systolic hypertension. N Engl J Med 1993;329:1912-7. [7.] Pickering TG, James GD, Boddie C, Harshfield GA, Blank S, Laragh JH. How common is white coat hypertension? JAMA 1988;259:225-8. [8.] Moser M. Can the cost of care be contained and quality of care maintained in the management of hypertension? Arch Intern Med 1994;154:1665-72. [9.] Five-year findings of the Hypertension Detection and Follow-up Program. 1. Reduction in mortality of persons with high blood pressure, including mild hypertension. Hypertension Detection and Follow-up Program Cooperative Group. JAMA 1979;242:2562-71. [10.] Julius S, Mejia A, Jones K, Krause L, Schork N, van de Ven C, et al. "White coat' versus "sustained' borderline hypertension in Tecumseh, Michigan. Hypertension 1990,16:617-23. [11.] Moser M, Hebert P. Prevention of disease progression, left ventricular hypertrophy and congestive heart failure in the hypertension treatment trials. J Am Coll Cardiol (In press). [12.] U.S. Public Health Service Hospitals Cooperative Study Group. Treatment of mild hypertension: results of a ten-year intervention trial. Circ Res 1977;40(Supple 1) :98-1'05. [13.] Veterans Administration Cooperative Study Group on Antihypertensive Agents. Effects of treatment on morbidity in hypertension: results in patients with diastolic blood pressure averaging 115 through 129 mm Hg. JAMA 1967;202:1028-34. [14.] The Australian Therapeutic Trial in Mild Hypertension. Lancet 1980;1:1261-7. [15.] Oslo Study. Treatment of mild hypertension. A five-year controlled drug trial. Am J Med 1980;69:725-32. [16.] MRC trial of treatment of mild hypertension: principal results. Medical Research Council Working Party. Br Med J [Clin Res] 1985;291:97-104. [17.] Medical Research Council Trial of treatment of hypertension in older adults: principal results. BMJ 1992;304:405-12. [18.] Veterans Administration Cooperative Study Group on Antihypertensive Agents, II: results of patients with diastolic blood pressure averaging 90 through 114 mm Hg. JAMA 1970;213:1143-51. [19.] The Systolic Hypertension in the Elderly Program Cooperative Research Group. Implications of the Systolic Hypertension in the Elderly Program. Hypertension 1993;21:335-43. [20.] Dahlof B, Lindhom LH, Hansson L, Schersten B, Ekbom T, Wester PO. Morbidity and mortality in the Swedish Trial Old Patients with Hypertension (STOP-hypertension). Lancet 1991;338:1281-5. [21.] Mortality and morbidity results from the European Working Party on High Blood Pressure in the Elderly. European Working Party on High Blood Pressure in the Elderly. Lancet 1985;1:1349-54. [22.] Coope J, Warrender TS. Randomized trial of treatment of hypertension in elderly patients in primary care. Br Med J 1986;293:1145-51. [23.] Effect of antihypertensive treatment on stroke recurrence. Hypertension-Stroke Cooperative Study Group. JAMA 1974;229:409-18. [24.] Wolff FW, Lindeman RD. Effects of treatment in hypertension: results of a controlled study. J Chronic Dis 1966;19:227-40. [25.] Carter AB. Hypotensive therapy in stroke surviviors. Lancet 1970;1:485-9. [26.] Hebert PR, Moser M, Mayer J, Glynn RJ, Hennekens CH. Recent evidence on drug therapy of mild to moderate hypertension and decreased risk of coronary heart disease. Arch Intern Med 1993;153:578-81. [27.] Moser M. Current hypertension management: separating fact from fiction. Cleve Clin J Med 1993;60:27-37. [28.] McInnes GT, Yeo WW, Ramsay LE, Moser M. Cardiotoxicity and diuretics: much speculation--little substance [Editorial]. J Hypertens 1992;10:317-35 [Published erratum appears in J Hypertens 1992; 10:following H24]. [29.] Freis E. Efficacy and safety of diuretics in treating hypertension. Ann Intern Med 1995;122:993-6. [30.] Moser M. Lipid abnormalities and diuretics. Am Fam Physician 1989;40(4):213-20. [31.] Materson BJ, Reda DJ, Cushman WC, Massie BM, Freis ED, Kochar MS, et al. Single-drug therapy for hypertension in men. A comparison of six antihypertensive agents with placebo. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents. N Engl J Med 1993;328;914-21. [32.] Yusuf S, Peto R, Lewis J, Collins R, Sleight P. Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis 1985;27:335-71. [33.] Pollare T, Lithell H, Berne C. A comparison of the effects of hydrochlorothiazide and captopril on glucose and lipid metabolism in patients with hypertension. N Engl J Med 1989;321:868-73. [34.] Moser M. Hypertension. In: Rakel R, ed. Conn's Current therapy. Philadelphia: Saunders, 1995:263-80. [35.] Wilhelmsen L, Berglund G, Elmfeldt D, et al. Beta blockers versus diuretics in hypertensive men. More results from the HAPPHY Trial. J Hypertens 1987;5:561-72. [36.] Gurwitz JH, Bohn RL, Glynn RJ, Monane M, Mogun H, Avom J. Antihypertensive drug therapy and the initiation of treatment for diabetes mellitus. Ann Intern Med 1993;118:273-8. [37.] Houston MC. New insights and new approaches for the treatment of essential hypertension: selection of therapy based on coronary heart disease risk factor analysis, hemodynamic profiles, quality of life, and subsets of hypertension. Am Heart J 1989;117:911-51. [38.] Lind L, Pollare T, Berne C, Lithell H. Long-term metabolic effects of antihypertensive drugs. Am Heart J 1994;128(6 Pt 1):1177-83.
This is Part I of a two-part article on management of hypertension. Part II will appear in the next issue.
MARVIN MOSER, M.D. is clinical professor of medicine at Yale University School of Medicine, New Haven, Conn., and senior medical consultant to the National High Blood Pressure Education Program of the National Heart, Lung, and Blood Institute. He was, chairman of the first Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure and a member of the JNC in 1980, 1988 and 1993. While maintaining an active practice for more than 40 years, Dr. Moser has done extensive research in the field of hypertension and written more than 350 scientific papers, 23 book chapters and four medical texts.
Address correspondence to Marvin Moser, M.D.., 13 Murray Hill Rd., Scarsdale, NY 10583.
COPYRIGHT 1996 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group