NEW ORLEANS -- The best contraceptive choices for women on antiepileptic medications are probably a progesterone-eluting intrauterine device or intramuscular medroxyprogesterone, with the higher doses of oral contraceptives running in second place, Anne Davis, M.D., said at the annual meeting of the American Epilepsy Society.
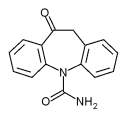
Some antiepileptic drugs--carbamazepine, oxcarbazepine, phenytoin, barbiturates (phenobarbital, mephobarbital and primidone), and topiramate--enhance the P450 cytochrome enzyme system. "This decline potentially decreases the effectiveness of hormonal methods of contraception," said Dr. Davis of Columbia University, New York.
The intrauterine device (IUD) and the depot medroxyprogesterone acetate (DMPA) (Depo-Provera) injection are not as prone to these drug interactions. The progesterone-eluting IUD thickens cervical mucus, impairs sperm movement, suppresses endometrial development, and has a slight anovulatory effect. DMPA suppresses ovulation and its progesterone content protects its effect from alterations in the enzyme system, Dr. Davis said.
In addition, the high progesterone content might have antiseizure properties. "This is a little bit of a teaser, something that's out there in the literature. Progesterone decreased seizure frequency in animal models, and DMPA decreased seizure frequency in women with intractable epilepsy. It's a tantalizing thing, but there's too little information out there to make any conclusions."
The second choice for women on the CYP450-en-hancing drugs would be higher dose oral contraceptives. "It's a little misleading to actually call some oral contraceptives 'high dose,' because everything these days is really low dose," she said. "What we're really talking about is differentiating between medium dose, low dose, and very low dose."
Experts have said that oral contraceptives containing 50 mcg estrogen are probably the most effective for these women, "But there are no real data to back that up," Dr. Davis said. The contraceptive patch and vaginal ring are comparable in estrogen dose with the 50-mcg pill.
The lower-dose pills are much more prone to failure in these women, as are progesterone-only pills. Neither the six-rod implant currently available nor the soon-to-be-approved single rod implant (Implanon) are good choices for this population, as they are both progesterone-only methods.
Some women may want to consider a barrier method, since this alleviates the concern of failure due to drug interaction. However, the failure rates of barrier methods are so much higher than those of hormonal methods that the chance of pregnancy is vastly increased, even taking into consideration drug interaction failures.
Even women taking medications that don't increase contraceptive failure may have special contraceptive considerations, Dr. Davis said. Numerous studies point to valproate's teratogenicity. Women on this drug who want to conceive may consider switching to another effective drug. If pregnancy is not in the cards for them, sterilization may be a viable alternative.
Women with catamenial epilepsy should use a form of birth control that reliably suppresses ovulation. DMPA is a good choice for this population. "Unlike the amenorrhea produced by the progesterone IUD, where they are still ovulating, the DPMA shot reliably suppresses ovulation," Dr. Davis said. "This is an important consideration for seizure frequency that's responsive to fluctuations in the menstrual cycle."
BY MICHELE G. SULLIVAN
Mid-Atlantic Bureau
COPYRIGHT 2005 International Medical News Group
COPYRIGHT 2005 Gale Group