Predicted developments
Establishment of prescribing guidelines, based on clinical studies, for drugs that are subject to substantial polymorphic metabolism
Prescribing advice will relate dose to genotype and will highlight the possibility of drug interactions when multiple drugs are prescribed concomitantly
Establishment and recording of individual patient genotypes--that is, "personal pharmacogenetic profiles"
Pharmacogenetics testing will substantially reduce the need for hospitalisation, and its associated costs, because of adverse drug reactions
Development of new drugs for patients with specific genotypes--that is, "drug stratification"
Individual variation in response to drugs is a substantial clinical problem. Such variation ranges from failure to respond to a drug to adverse drug reactions and drug-drug interactions when several drugs are taken concomitantly. The clinical consequences range from patient discomfort through serious clinical illness to the occasional fatality. One UK study has suggested that about 1 in 15 hospital admissions are due to adverse drug reactions,[1] and a recent US study estimated that 106 000 patients die and 2.2 million are injured each year by adverse reactions to prescribed drugs.[2]
It is now clear that much individuality in drug response is inherited: this genetically determined variability in drug response defines the research area known as pharmacogenetics.[3] This article discusses the potential of pharmacogenetic testing to improve both the efficacy and safety of drug prescribing.
Methods
We compiled the article from the published literature, information presented at scientific meetings, our own published research work, and information gained from working with the pharmaceutical industry on drugs in development.
The human genome and polymorphism
Pharmacogenetic research has gained enormous momentum, with recent advances in molecular genetics and genome sequencing. This is due to the emergence of technologies that permit rapid screening for specific polymorphisms, as well as our recently gained knowledge of the genetic sequences of target genes such as those coding for enzymes, ion channels, and other types of receptors involved in drug response.[4]
Research in pharmacogenetics is currently developing in two main directions: firstly, identifying specific genes and gene products associated with various diseases, which may act as targets for new drugs, and, secondly, identifying genes and allelic variants of genes that affect our response to current drugs.
Identifying novel targets for new drugs
Increasing numbers of research programmes are developing from the human
genome project, including genome-wide screens to identify single nucleotide polymorphisms--that is, differences between individuals of a single base pair in their DNA. These can be used to map and identify specific genes associated with various diseases such as diabetes, cancer, and arthritis. Many of the proteins encoded by these genes are expected to become targets for new drugs. The fact that these genes were identified by polymorphism analysis indicates that drugs directed at such targets may have different effects in different patients and that some drugs will be most effective in patients with specific gene variants. This leads to the concept of drug stratification or individualised drug treatment, in which the choice of drug is influenced by a patient's genetic status.
This type of genomic analysis will generate an enormous amount of information on human polymorphism, and several hundred thousand single nucleotide polymorphisms will probably be identified in the next few years. However, a greater challenge will be determining the function of each polymorphic gene or, to be more exact, of the gene product and its variant forms. In particular, it will be necessary to determine whether a gene product is of pharmacological or toxicological importance and whether individual allelic variants are of therapeutic importance. These are major hurdles, and it will be many years before this aspect of pharmacogenetics is practicable in drug development. However, the future fortunes of many in the global pharmaceutical industry are predicated on such a "genomic" approach to discovering new drugs.
Identifying genetic variants associated with adverse drug reactions
Much closer to clinical application is determining the genetic variations that affect the efficacy of current drugs. Polymorphism in any one of many genes--including those encoding drug receptors, drug transporters, and cell signalling pathways--can be important determinants of clinical response. However, the most immediately exploitable polymorphisms are those in the genes involved in drug metabolism and disposition. Functional polymorphisms in any one of these genes can lead to either a lack of therapeutic effect or an exacerbated clinical response (see box 1). Polymorphisms have now been identified in more than 20 human drug metabolising enzymes, several with substantial ethnic differences in their frequencies, and the phenotypic consequences of some of these are critical determinants of therapeutic outcome (see table). Important examples are polymorphisms in the cytochrome P450 enzymes and in thiopurine methyltransferase.
Box 1: Potential consequences of polymorphic drug metabolism
* Extended pharmacological effect
* Adverse drug reactions
* Lack of prodrug activation
* Drug toxicity
* Increased effective close
* Metabolism by alternative, deleterious pathways
* Exacerbated drug-drug interactions
Cytochrome P450s
The cytochrome P450s are a multigene family of enzymes found predominantly in the liver that are responsible for the metabolic elimination of most of the drugs currently used in medicine.[5] Genetically determined variability in the level of expression or function of these enzymes has a profound effect on drug efficacy. In "poor metabolisers" the genes encoding specific cytochrome P450s often contain inactivating mutations, which result in a complete lack of active enzyme and a severely compromised ability to metabolise drugs. Thus, mutations in the gene encoding cytochrome P450 CYP2C9, which metabolises warfarin, affects patients' response to the drug and their dose requirements.[6] Polymorphism not only affects drug disposition but can also be important in the conversion of prodrugs to their active form. For example, codeine is metabolised to the analgesic morphine by CYP2D6, and the desired analgesic effect is not achieved in CYP2D6 poor metabolisers.
Cytochrome P450 CYP2D6
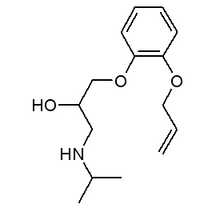
CYP2D6, also known as debrisoquine hydroxylase, is highly polymorphic and is inactive in about 6% of white people. In Britain several million people are thus at risk of compromised metabolism or adverse drug reactions when prescribed drugs that are CYP2D6 substrates. Many such drugs are used for treating psychiatric, neurological, and cardiovascular diseases (see box 2), where the therapeutic window can be narrow and side effects are common.
Box 2: Examples of drugs that are substrates of cytochrome P450 CYP2D6
Drugs for treating psychiatric and neurological disease
Amitriptyline, clomipramine, clozapine, desipraminc, desmethylcitalopram, fluvoxamine, fluoxetine, haloperidol, imipramine, levomepromazine, maprotiline, mianserin, nortriptyline, olanzapine, paroxetine, perphenazine, risperidone, thioridazine, tranylcypromine, venlafaxine, zuclopenthixol
Drugs for treating cardiovascular disease
Alprenolol, amiodarane, flecainide, indoramin, mexiletine, nimodipine, oxprenolol, propranolol, timolol
Another variant results from amplification of the entire CYP2D6 gene, with some individuals inheriting up to 13 copies of the gene, arranged in tandem.[7] This amplification polymorphism results in affected people metabolising drugs that are CYP2D6 substrates so quickly that a therapeutic effect cannot be obtained at conventional doses. For example, it has been estimated that, while a daily dose of 10-20 mg nortriptyline would be sufficient for a patient who is a CYP2D6 poor metaboliser, an "ultra-rapid metaboliser" inheriting multiple copies of the gene could require as much as 500 mg a day.[8]
Clinical problems can also arise from the co-administration of drugs that inhibit or compete for CYP2D6. A drug may interact with and inhibit CYP2D6 to the extent that it is no longer functionally active, resulting in a patient responding like a poor metaboliser even though he or she has an "extensive metaboliser" genotype. Thus, quinidine, a powerful CYP2D6 inhibitor, may exaggerate the effects of other drugs that are prescribed concomitantly or may prevent the metabolic activation of drugs such as codeine by CYP2D6.
Thiopurine methyltransferase
Another clinically important polymorphism occurs in the enzyme thiopurine methyltransferase (TPMT),[9] which is responsible for the metabolism of the antitumour agents 6-mercaptopurine and 6-thioguanine. Genetic polymorphism at this gene locus is associated with difficulty in achieving an effective dose of these drugs in children with childhood leukaemia.[10] Children with inherited TPMT deficiency exhibit severe haematopoietic toxicity when exposed to drugs such as 6-mercaptopurine, whereas those with a high activity form of the enzyme require high doses of the drug to achieve any clinical benefit. The TPMT polymorphism is relatively rare, with only about 1% of the white population being homozygous for it, but, since these individuals show exaggerated toxic responses to normal doses of thiopurine, TPMT phenotype may be an important factor in the successful treatment of childhood leukaemia. Some centres already provide a diagnostic phenotyping service to guide the clinical use of 6-mercaptopurine.
The current situation
Pharmacogenetic testing is currently used in only a limited number of teaching hospitals and specialist academic centres. It is currently most advanced in Scandinavian countries. The most widely accepted application of pharmacogenetic testing is the use of CYP2D6 genotyping to aid individual dose selection for drugs used to treat psychiatric illness.
Several independent testing laboratories provide the pharmaceutical industry and medical practice with a high throughput, DNA based, testing service for a range of pharmacogenetic polymorphisms. It is, however, difficult to predict to what extent the pharmaceutical industry will routinely incorporate pharmacogenetic testing into prescribing schedules for drugs that are subject to polymorphic metabolism. This will depend to some extent on the attitude taken by drug licensing authorities.
To test or not to test?
Until recently, the only way to identify a patient with a genetic risk factor for a particular adverse drug reaction was with "phenotyping tests," with the administration of a specific marker drug or test substance. Such procedures were tedious, involving the invasive administration of the test substance and the collection of samples and subsequent biochemical analysis. Modern DNA based tests, which require only a small sample of tissue--blood from a finger prick, cells from a mouth wash, or hair follicle cells--enable the rapid and unequivocal determination of the "pharmacogenetic profile" or genotype of a patient.
The clinical applicability of pharmacogenetic testing depends on the relative importance of each polymorphism in determining therapeutic outcome (figure). Doctors need to be aware of whether a drug they are prescribing is subject to pharmacogenetic variability and know how use this knowledge. In addition, a reliable DNA based testing service needs to be available. For certain pharmacogenetic polymorphisms (such as CYP2D6), we believe that there is now sufficient knowledge about the implications of genetically determined variation to instigate population based pharmacogenetic testing. Details of more than 20 drugs that are known to be CYP2D6 substrates are now provided in both the ABPI Compendium of Data Sheets in Britain and the Physicians Desk Reference in the United States.[11 12] This may allow the choice and doses of specific drugs, particularly those for treating psychiatric disorders, to be used more appropriately. At present, adverse drug reactions occur in a substantial proportion of patients: a recent US study showed that, in patients prescribed psychiatric drugs that are CYP2D6 substrates, adverse drug reactions were observed in every patient with inherited mutations inactivating the CYP2D6 gene.[13]
[Figure ILLUSTRATION OMITTED]
The future
Pharmacogenetic testing may provide the first example of a mechanism whereby DNA based testing can be applied to populations, but we are still a long way from having a pharmacogenetic DNA chip that general practitioners can use to identify all the drugs to which any particular patient is sensitive. However, there is increasing evidence that pharmacogenetics will be extremely important in the health service. One day it may be considered unethical not to carry out such tests routinely to avoid exposing individuals to doses of drugs that could be harmful to them. The ability to identify sensitive individuals, either before drug treatment or after an adverse drug response would also be of economic importance as it would avoid the empiricism associated with matching the most appropriate drug at its optimal dose for each patient. It might also substantially reduce the need for hospitalisation, and its associated costs, because of adverse drug reactions.
Our increasing knowledge of the mechanisms of drug action, the identification of new drug targets and the understanding of genetic factors that determine our response to drugs may allow us to design drugs that are specifically targeted towards particular populations or that avoid genetic variability in therapeutic response. The extent of genetic polymorphism in the human population indicates that pharmacogenetic variability will probably be an issue for most new drugs.
The development of pharmacogenetics provides at least one mechanism for taking prescription away from its current empiricism and progressing towards more "individualised" drug treatment. In view of the momentum that pharmacogenetics is developing, it is essential that the subject is taught as part of the medical student curriculum.
Contributors: CRW wrote the first draft of the article and collated the comments and additions of the other authors. RLS made extensive revisions to the first draft, as did GS, who also produced the boxes and table. All three were responsible for the intellectual content of the article.
Competing interests: CRW and RLS are consultants to the Laboratory of the Government Chemist, which provides the pharmaceutical industry with a testing service for several pharmacogenetic polymorphisms. RLS is currently chairman of Genotype.
[1] The cost of adverse drug reactions [editorial]. Adverse Drug React Toxicol Rev 1997;16:75-8.
[2] Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalised patients: a meta-analysis of prospective studies. JAMA 1998;279:1200-5.
[3] Vogel F. Moderne probleme der Humangenetik. Ergeb Inn Med Kinderheild 1959;12:52-125.
[4] Weber WW. Pharmacogenetics. Oxford: Oxford University Press, 1997.
[5] Wolf CR, Smith G. Pharmacogenetics. Br Med Bull 1999;55:366-86.
[6] Aithal GP, Day CP, Kesteven PJ, Daly AK. Association of polymorphisms in the cytochrome P450 CYP2C9 with warfarin dose requirement and risk of bleeding complications. Lancet 1999;353:717-9.
[7] Johansson I, Lundquist E, Bertilsson L, Dahl ML, Sjoqvist F, Ingelman-Sundberg M. Inherited amplification of an active gene in the cytochrome P450 CYP2D locus as a cause of ultrarapid metabolism of debrisoquine. Proc Natl Acad Sci (USA) 1993;90:11825-9.
[8] Bertilsson L, Dahl ML, Sjoqvist F, Aberg-Wistedt A, Humble M, Johansson I, et al. Molecular basis for rational mega-prescribing in ultrarapid hydroxylators of debrisoquin. Lancet 1993;341:363.
[9] Lennard L, Lilleyman JS, Van Loon J, Weinshilboum RM. Genetic variation in response to 6-mercaptopurine for childhood acute lymphoblastic leukaemia. Lancet 1990;336:225-9.
[10] Krynetski EY, Tai HL, Yates CR, Fessing MY, Loennechen T, Sheutz JD, et al. Genetic polymorphism of thiopurine S-methyltransferase: clinical importance and molecular mechanisms. Pharmacogenetics 1996;6:279-90.
[11] ABPI compendium of data sheets and summaries of product characteristics 1999-2000. London: Datapharm, 1999.
[12] Physicians' Desk Reference 2000. 54th ed. Montvale NJ: Medical Economics, 1999.
[13] Chou WH, Yan F-X, de Leon J, Barnhill J, Rogers T, Cronin M, et al. An extension of a pilot study: impact from the cytochrome P450-2D6 (CYP2D6) polymorphism on outcome and costs in severe mental illness. J Clin Psychopharmacol (in press).
Imperial Cancer Research Fund Molecular Pharmacology Unit, Ninewells Hospital and Medical School, Dundee DD1 9SY C Roland Wolf director
Biomedical Research Centre, Ninewells Hospital and Medical School, Dundee Gillian Smith research associate
Imperial College School of Medicine, Division of Biomedical Sciences, Section of Molecular Toxicology, Sir Alexander Fleming Building, London SW7 2AZ Robert L Smith senior research fellow
Correspondence to: C R Wolf rooney@icrf. icnet.uk
BMJ 2000;320:987-90
COPYRIGHT 2000 British Medical Association
COPYRIGHT 2000 Gale Group