Key points for clinicians
The effective management of comorbidities, including those that are psychologic in nature, is critical to successful tong-term management of chronic pain (C).
Anti-inflammatory medications are the mainstay of treatment for mild to moderate chronic nociceptive pain, with opioids appropriate in patients with moderate to severe chronic nociceptive pain (C).
Adjuvant analgesics, eg, antidepressants, anticonvulsants, topical agents, and opioids are the mainstay of treatment for chronic neuropathic pain (C).
Combination therapy is generally required to achieve adequate analgesia in chronic pain disorders (C).
Because chronic pain is a complex condition with intrinsic sensory, emotional, and behavioral components contributing to its etiology and severity, managing chronic pain disorders can be challenging. Although the psychosocial aspects of chronic pain management are of critical importance to the successful treatment of chronic pain disorders, a detailed review of it is beyond the scope of this article; psychosocial aspects of treatment will be discussed only tangentially. Since pharmacologic therapy currently is the most efficacious means of managing chronic pain disorders, it will be the primary focus of this article.
Chronic pain may have various causes: nociceptive pain, neuropathic pain (NP), or mixed nociceptive/NP-type pain. The underlying mechanisms for each of these types of chronic pain are distinctly different, as are the recommended pharmacologic treatment approaches. Anti-inflammatory agents are the basis of treatment for nociceptive pain, as inflammation caused by noxious thermal or mechanical stimuli is the precipitating cause of the pain. In contrast, anti-inflammatory agents play essentially no role in the management of NP. Instead, adjuvant analgesics, medications that have primary indications other than pain but produce analgesic effects in some conditions, are the drugs most frequently used for treating chronic NP.
There are several goals in the management of chronic pain:
* Prevent symptoms, if possible
* Reduce pain severity or frequency
* Improve physical functioning
* Reduce psychologic distress
* Improve overall quality of life
* Minimize treatment-related adverse effects.
While complete resolution of the patient's pain is the ideal goal, this is rarely achieved, despite comprehensive multidisciplinary pain management. A more realistic goal is to reduce the pain intensity by at least 50%, or more importantly, to improve patient functioning so that the patient may have an acceptable quality of life. Disability, especially when chronic pain exists for more than 6 to 12 months, generally is not completely resolved, (1) particularly if psychosocial aspects are not addressed appropriately. These factors may complicate treatment responses and negatively impact the patient's motivation to adhere to the management plan. Consequently, open communication with the patient is essential, and psychosocial interventions may be required. Whereas the physician alone often can adequately manage acute pain, the management of chronic pain disorders is complex and often is best accomplished using a team approach. (2)
* CHRONIC NOCICEPTIVE PAIN
Most nociceptive pain disorders are temporary conditions that resolve when the cause of the inflammation is removed or otherwise medically treated. In some situations, however, the condition becomes chronic. Diseases in which this occurs include the arthropathies, mechanical low back pain, fibromyalgia, sickle cell disease, and cancer.
Since inflammation plays a major role in the genesis of chronic nociceptive pain, anti-inflammatory agents play an important role in its management. The analgesic ladder, initially developed by the World Health Organization for cancer pain management, describes a stepwise approach that can be applied also to noncancer pain (FIGURE 1). (3) First-line therapies for mild pain include acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs). Although they have no anti-inflammatory properties, opioid analgesics are useful, too, for managing nociceptive pain, primarily moderate-to-severe pain or as second-line agents when pain relief with anti-inflammatory agents is incomplete.
[FIGURE 1 OMITTED]
Acetaminophen in doses up to 4 g per day provides pain relief comparable to that of traditional NSAIDs. Although acetaminophen is safe and widely available at low cost, its use is not without limitations. Acetaminophen should be used with caution in patients with a history of alcohol abuse. Also, long-term use of daily doses above 2 g should be avoided, especially in older patients and those with liver disease. (4,5) Furthermore, daily doses above 1 to 2 grams have been found to prolong the international normalized ratio (INR) in some patients receiving warfarin, which suggests that the INR should be monitored at the initiation of and during sustained therapy with large doses of acetaminophen. (5,6)
Nonsteroidal anti-inflammatory agents include the traditional nonselective NSAIDs (ibuprofen, indomethacin, diclofenac, diflunisal, naproxen, etc), the cyclooxygenase-2 (COX-2) selective inhibitors (celecoxib, rofecoxib, valdecoxib), aspirin, and the nonacetylated salicylates (choline salicylate or magnesium salicylate). Numerous scientific and clinical trials have been conducted to assess the efficacy and safety of one or more COX-2 selective inhibitors with other agents, particularly traditional NSAIDs. These studies generally show that the efficacy of traditional NSAIDs and COX-2 selective inhibitors is similar, (7-12) although an individual patient may respond to (and tolerate) specific agents differently from other patients. For this reason, lack of satisfactory pain relief with one NSAID or COX-2 selective inhibitor does not preclude the possible benefit of treatment with another. The primary reason to use a COX-2 selective inhibitor or a nonacetylated salicylate as opposed to a traditional NSAID is a significantly reduced incidence of gastrointestinal (GI) bleeding with the COX-2 selective inhibitors and nonacetylated salicylates. (7-9,13-15) COX-2 selective inhibitors and nonacetylated salicylates are valuable also in preoperative pain management because of their lack of antiplatelet effects. Concern exists, however, regarding the increased risk of cardiovascular events observed with rofecoxib, especially in doses above 25 mg per day. (16,17)
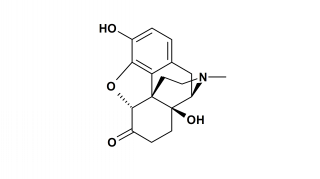
Numerous studies have established the role of opioid analgesics for the management of chronic pain. (18-22) Opioids produce analgesia by binding to specific receptors both within and outside of the central nervous system (CNS). Opioid analgesics are classified as full (mu) agonists, partial agonists, or mixed agonist-antagonists, depending upon the receptors to which they bind and their intrinsic activity at those receptors. Full agonists do not have a ceiling to their analgesic effect, whereas partial agonists and mixed agonist-antagonists do. Patients receiving full opioid agonists (eg, morphine, hydrocodone, hydromorphone, oxycodone, oxymorphone, fentanyl) should not be given a mixed agonist/antagonist (eg, pentazocine, butorphanol, nalbuphine), as this may precipitate a withdrawal syndrome and increase pain.
The oral route of administering opioid analgesics usually is preferred for patients with chronic pain because of convenience, flexibility, relatively steady blood levels and cost-effectiveness. Short-acting agents given "around-the-clock" generally are preferable during titration to prevent pain from recurring in patients with continuous or frequent pain. Patients with severe pain may need rapid titration with a continuous intravenous infusion of morphine. Once the pain is under control, a long-acting opioid may be used. Opioid doses should be adjusted in each patient to obtain the optimal balance between pain relief and side effects. Supplemental use of an immediate-release opioid on a prn basis is appropriate to prevent pain at predictable times during the day or in association with specific activities. In addition, an immediate-release opioid also can be used for some causes of breakthrough pain. The type of breakthrough pain should be identified so that appropriate steps can be taken. (IA) End-of-dose failure is the result of decreased blood levels of analgesic with concomitant increase in pain before the next scheduled dose. If this occurs routinely, consideration should be given to decreasing the interval between doses of continuous-release agents. Increasing the dose of the continuous-release agents is another consideration, but this may cause undesirable effects, such as sedation. (IIIB) Spontaneous pain, common with neuropathic pain, is commonly fleeting and difficult to predict. (IC) Incident pain is usually caused by activity that can be anticipated and pretreated. (IB) In the case of incident pain, a rapid-acting agent is preferred. (22,23) [Evidence levels: Level I: Evidence from at feast one property randomized, controlled trial. Level III: Evidence from respected authorities, based on clinical experience, descriptive studies, or reports of expert committees. Types: A. Good evidence to support the use of a recommendation; clinicians "should do this all the time." B. Moderate evidence to support the use of a recommendation; clinicians "should do this most of the time." C. Poor evidence either to support or to reject the use of a recommendation; clinicians "may or may not follow the recommendation." Available at: http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id= 3365&nbr=2591&string=chronic%20AND%20pain.]
For mild-to-moderate pain requiring an opioid, possible choices include: tramadol or an opioid-acetaminophen combination such as acetaminophen with codeine, hydrocodone, or oxycodone. For moderately severe-to-severe pain, morphine, hydromorphone, hydrocodone, and oxycodone can be used. These drugs should be used cautiously in a fixed combination with acetaminophen or other NSAID to avoid toxicity from acetaminophen or the NSAID. In cases where the pain is constant or breakthrough pain is frequent, sustained-released morphine or oxycodone, a transdermal fentanyl patch, methadone or levorphanol, are possible options. (20,22) Meperidine is not recommended because of its low oral bioavailability and toxicity associated with its metabolite with high doses. Similarly, propoxyphene has few indications because of low analgesic efficacy, a ceiling effect, and a potential for abuse. (20)
Whenever opioid therapy is being considered, the potential for misuse, abuse, and addiction needs to be proactively addressed (see Dr Gallagher's article). Overall, the available literature suggests that iatrogenic addiction is rare in patients receiving opioids for acute pain, as well as in those without a history of substance abuse who receive longer-term opioid therapy for medical indications.
Constipation, sedation, nausea, and vomiting are the most common side effects associated with opioid therapy. Tolerance to these side effects typically occurs 2within a few days to weeks, while constipation frequently persists and should be treated appropriately. Other opioid-related side effects include altered cognitive function, pruritus, and respiratory depression. Although respiratory depression is rare in patients who have been receiving chronic opioid therapy, it is a risk in the treatment of opioid-naive patients with severe pain who require high doses.
Opioid-induced neurotoxicity, characterized by delirium, agitation, myoclonus, or hyperalgesia, which may occur with high-dose or prolonged opioid administration, should be managed with hydration, dose reduction, and opioid rotation. Opioid rotation involves abruptly stopping one opioid and replacing it with an alternative opioid. This is accomplished by initiating treatment with the new opioid at a daily dose 30% to 50% lower than the equianalgesic dose and then slowly increasing the dose until adequate analgesia is achieved. (23,24) Although methadone has become an attractive option for opioid rotation, its long and variable elimination half-life, possibly leading to drug accumulation, and difficulty in establishing equianalgesic doses with other opioids, limit its use to clinicians who understand the pharmacokinetics of methadone and are familiar with published protocols for opioid rotation to methadone. (22,24)
Opioid rotation has also become an accepted strategy for a patient who does not achieve adequate analgesia. The rationale for opioid rotation includes interpatient variability of response, incomplete cross-tolerance, and the interaction between specific opioids and liver metabolism utilizing the cytochrome P-450 system. For example, morphine, codeine, hydrocodone, oxycodone, and methadone are metabolized via the CYP2D6 hepatic enzyme. If a person is a slow metabolizer at the CYP2D6 hepatic enzyme or is taking concomitant medications that also are metabolized through this same pathway (eg, tricyclic antidepressant or selective serotonin reuptake inhibitor [SSRI]), an opioid that is not metabolized through the CYP2D6 hepatic enzyme (eg, fentanyl, oxymorphone) may be a rational choice when considering opioid rotation.
* OSTEOARTHRITIS
Pharmacologic treatment for osteoarthritis (OA) should begin with an analgesic. Guidelines developed by the American College of Rheumatology (ACR), (25) American Pain Society, (26) and American Geriatric Society, (27) all recommend acetaminophen as initial treatment for mild-to-moderate pain. As an alternative to systemic therapy with acetaminophen, topical capsaicin cream, 4 times daily, can be applied for patients with 1 or 2 affected joints. (25)
For those patients who fail to obtain adequate symptomatic relief with acetaminophen or topical analgesic therapy, several alternatives are available. (25) A traditional NSAID alone can be used in patients without a risk for GI bleeding. In those with a risk for GI bleeding, an NSAID in combination with misoprostol or a proton pump inhibitor or a COX-2 selective inhibitor, such as celecoxib, rofecoxib, or valdecoxib, is appropriate. If an adequate response is not achieved, tramadol or another opioid can be used. Tramadol is especially useful in patients who have contraindications to COX-2 selective inhibitors and NSAIDs, including impaired renal function, (25) but tramadol should be avoided in patients with a seizure disorder or in those taking an SSRI. (5) Opioids administered around-the-clock are effective in moderate to severe OA pain. (28-30)
Patients with moderate-to-severe pain due to OA should be treated initially with an intra-articular glucocorticoid or an oral NSAID according to the ACR, (25) while the American Pain Society recommends a COX-2 selective inhibitor. (26) Intra-articular administration of a glucocorticoid should not be performed more than 3 times per year. (5) Viscosupplementation with intra-articular hyaluronic acid is equally effective as oral NSAID therapy, with only minor local reactions. (31,32)
The role of topical agents and intra-articular injection of glucocorticoids and hyaluronic acid is not well studied in OA of the hip. (5,25)
* RHEUMATOID ARTHRITIS
Therapy for rheumatoid arthritis (RA) is much more aggressive than for OA as it is now clear that for there to be an impact on long-term morbidity and mortality, effective treatment of active RA requires early diagnosis and early treatment with disease-modifying antirheumatic drugs (DMARDs). The ACR recommends treatment be initiated with patient education and physical therapy, a DMARD or DMARDs, and possibly a corticosteroid and/or an NSAID or COX-2 selective inhibitor. (33) When oral glucocorticoids are used, prophylaxis with a bisphosphonate, along with calcium supplementation and daily supplemental vitamin D to lower the risk of glucocorticoid-induced osteoporosis, should be considered. [Evidence level: B. There is evidence of types II, III, or IV, and findings are generally consistent. Available at: http://www.guideline.gov/summary/ summary.aspx?ss=15& doc_id=3691&nbr=2917&string=juvenile%20AND%20arthritis.]
If the response to treatment is not adequate after 3 months, therapy should be altered by changing or adding DMARDs, either as monotherapy or in combination. Biologic DMARDs also should be considered either alone or as add-on therapy. Patients who still do not respond adequately despite being on several DMARD regimens should be considered for surgical intervention.
Patients who should be considered for referral to a rheumatologist include those with 3 or more swollen joints, involvement of the metatarsophalangeal and/or metacarpophalangeal joint(s) with a positive squeeze test, and morning stiffness for 30 minutes or more (TABLE 1). In addition, patients who are positive for rheumatoid factor, have an acute phase response, or in whom erosions are evident radiographically should be referred to a rheumatologist regardless of presenting symptoms. It is important to note that NSAID use can mask the symptoms of RA. (34)
It is important to remember that while analgesic and anti-inflammatory medications are important in arthritis pain management, [they] should be used concurrently with nutritional, physical, educational, and cognitive-behavioral interventions, which are briefly discussed below. [Evidence level: A. There is evidence of type I or consistent findings from multiple studies of types II, III, or IV. Available at: http://www.guideline.gov/summary/ summary.aspx?ss=15&doc_id=3691&nbr=2917&string=ju venile%20AND%20arthritis.]
* CHRONIC LOW BACK PAIN
While there is strong evidence supporting the use of pharmacologic agents in the management of acute low back pain, there is significantly less evidence substantiating their use in chronic low back pain. Acetaminophen and NSAIDs may be of short-term benefit, but the evidence supporting their use is largely anecdotal. (35,36) Opioids have been shown to have a modest positive effect on pain and mood but little effect on activity and sleep. (19) Antidepressants also provide only partial pain relief, and their use is limited by side effects. (35) Muscle relaxants, including benzodiazepines and cyclobenzaprine, have been studied poorly in chronic low back pain. While effective in acute, nonspecific low back pain, adverse CNS effects limit their role. (37)
Numerous nonpharmacologic approaches also have been investigated. Among these, exercise, such as strengthening exercises, walking, bicycling, and swimming, appears to be the most helpful. (38,39) Massage, particularly acupuncture massage, may be beneficial especially when combined with exercises and education. (40) Acupuncture alone, however, appears to be ineffective. (41) Behavioral treatment seems to be effective, although the type of patients who benefit most from a specific type of behavioral treatment remains unclear. (42) Transcutaneous electrical nerve stimulation (TENS) (43) and injection therapy (44) have been found to be ineffective.
* CHRONIC NEUROPATHIC PAIN
Neuropathic pain (NP), which results from disease, injury, or dysfunction in the peripheral nervous system or the CNS, is a heterogeneous group of pain disorders. While precise estimates of the prevalence of NP are not available, it is likely that NP is more common than is generally appreciated. In the United States alone, there may be more than 3 million people with painful diabetic neuropathy and as many as 1 million with postherpetic neuralgia. (45) Other examples of common chronic NP disorders seen in primary care include neuropathic low back pain, cancer-related neuropathy, carpal tunnel syndrome, trigeminal neuralgia, postischemic myelopathy, and poststroke pain. (46,47)
Diabetic polyneuropathy and postherpetic neuralgia are the best studied of the NP disorders in terms of management. While the extent to which the results of clinical trials in one NP syndrome applies to other chronic NP syndromes cannot be determined presently, current knowledge about underlying pathophysiology, presenting signs/symptoms, and results of controlled clinical trials suggest that treatments effective in one NP disorder can be expected to be efficacious in other NP conditions. (45)
The management of chronic NP involves treating any underlying condition that may be causing or contributing to the pain. For example, painful peripheral diabetic neuropathy in a patient with diabetes mellitus requires close attention to home glucose monitoring and blood glucose control. Therapy to provide symptomatic relief from pain and disability, as well as to prevent recurrence is essential. In some cases, pain relief might be obtained through direct intervention, such as surgical release of an entrapped nerve or epidural steroids for lumbar radiculopathy. Symptomatic treatment always should be offered in combination with corrective treatment, if appropriate. Since preventive measures are sometimes available, patients who are at known risk of chronic pain should receive preventive treatment and be counseled regarding the possibility of the development of a chronic pain syndrome. Providing antiviral agents for patients with acute herpes zoster, for example, may help to prevent postherpetic neuralgia.
Unfortunately, because of the complex pathophysiology of NP, treatment of patients with chronic NP is rarely effective in completely eliminating the pain. Consequently, appropriate goals of management should be discussed with the patient so that realistic expectations are established and treatment options are prioritized. Here, the goal generally is to improve the patient's quality of life and function.
* SYMPTOMATIC TREATMENT
Since chronic NP is not an inflammatory condition, anti-inflammatory analgesics generally are not helpful. Instead, pharmacologic therapies for chronic NP tend to involve adjuvant agents such as antidepressants, topical analgesics, anticonvulsants, opioids, and other miscellaneous agents (TABLE 2). (45,48,49)
Recently published evidence-based consensus guidelines for the treatment of chronic NP support the use of gabapentin, the lidocaine patch 5%, opioid analgesics, tramadol, and tricyclic antidepressants, as first-line medications for NP. (45) These recommendations are based on positive results of multiple randomized controlled trials. Also, clinical circumstances exist in which each agent can be used in the initial treatment of NP. The guidelines state, however, that opioid analgesics and tricyclic antidepressants generally require greater caution in administration, are less well tolerated, and have less overall ease of use than the other options. Consequently, the initiation of treatment with opioids and tricyclic antidepressants can be expected to occur less frequently.
These evidence-based guidelines also discuss second-line agents that can be considered when patients do not have a satisfactory response to treatment with the 5 first-line medications alone or in combination. These first- and second-line therapies are discussed below with an emphasis on key considerations on their use in the management of chronic NP disorders. It is important to keep in mind that only 3 drugs have been approved by the US Food and Drug Administration for chronic NP: carbamazepine for trigeminal neuralgia and gabapentin and the lidocaine patch 5% for postherpetic neuralgia. A discussion of clinical trials and other evidence is not provided within the context of this article, but the chronic NP disorders for which each drug has been found useful are noted in TABLE 2. Finally, this section will conclude with an overview that puts the key considerations of each drug or drug class into clinical context by providing recommendations regarding the management of several chronic NP disorders. Children and older adults present special challenges to primary care physicians but are not the focus of the following discussion.
* FIRST-LINE MEDICATIONS
Based on the results of multiple randomized controlled clinical trials and the clinical experience of the expert panel, gabapentin, the lidocaine patch 5%, opioids, tramadol, and tricyclic antidepressants are considered first-line medications (TABLE 2). (45)
Gabapentin has been shown to improve sleep, mood, and quality of life in some patients with chronic NP. (45) Gabapentin is less likely to be effective when it is prescribed for questionable neuropathic pain conditions with no objective finding of nerve injury, such as complex regional pain syndrome (CRPS) type 1. [Evidence level: The type of supporting evidence is not specifically stated for each recommendation. The guideline is based on a literature review of the current scientific information and on expert opinion from actively practicing physicians who regularly treat patients with this condition. Available at: http://www.guideline. gov/summary/summary.aspx?ss=15&doc_id=3550&nbr=2776&strin g=gabapentin.] Gabapentin must be used with caution in older patients because of the risk of falls and cognitive impairment. An adequate trial of gabapentin takes 3 to 8 weeks to allow the development of tolerance to adverse effects, plus 1 to 2 weeks at the maximum tolerated dosage. Compared with most of the oral agents used for chronic NP, gabapentin is unique in its overall excellent tolerability, safety, and lack of drug interactions. (45,50,51)
The lidocaine patch 5% has an excellent safety and tolerability profile since systemic absorption is minimal with a dosage schedule of 12 hours on and 12 hours off. (45) Patients with intact skin who have localized or regional pain syndromes (eg, post-herpetic neuralgia) may benefit from commercially available topical therapies (eg, capsaicin cream, lidocaine patch). [Evidence lever: IB. Evidence from at least one property randomized, controlled trial. Moderate evidence to support the use of a recommendation; clinicians "should do this most of the time." Available at: http://www.guideline. gov/summary/summary. aspx?ss=15&doc_id=3365&nbr=2591&string=topical%20AND%2 Olidocaine.] In addition, the lidocaine patch 5% requires no dosage titration; an adequate trial takes 2 weeks. (45)
Opioids are effective in a wide variety of pain disorders and are a good choice in patients who have a concomitant non-NP disorder. Tramadol is especially useful in patients who also suffer from a concomitant non-NP disorder. Tramadol increases the risk of seizures in those predisposed, and for serotonin syndrome when used concomitantly with an SSRI or a monoamine oxidase inhibitor. Dosage adjustment is needed in renal or hepatic disease. (45)
Tricyclic antidepressants are useful in patients with chronic NP, although intentional overdose is a possibility. Since the doses used for pain management are generally lower than those required for depression or a sleep disorder, the use of a tricyclic antidepressant for chronic pain in a patient with comorbid depression or sleep disorder may not completely resolve the comorbid illness. Should this occur, the addition of a different antidepressant, such as an SSRI, may be needed.
Many drawbacks to tricyclic antidepressants exist, and they must be used cautiously in older patients. Nortriptyline and desipramine are better tolerated and equally effective as amitriptyline. Tricyclic antidepressants should not be used in patients with cardiovascular disease, and a screening electrocardiogram is recommended before beginning treatment, especially in patients aged 40 years or older. The onset of pain relief appears to be biphasic and occurs within hours or days, although 6 to 8 weeks generally are needed to achieve the maximal effect. Drug interactions occur with many commonly used drugs. (45,51)
Gabapentin, the lidocaine patch 5%, and opioid analgesics all have fewer drug interactions than tramadol or tricyclic antidepressants.
Following an adequate trial, patients who do not achieve their individualized goals of therapy should be started on a different first-line medication. Should the goals of therapy still not be achieved with the five first-line medications alone or in combination, various second-line medications can be considered.
* SECOND-LINE MEDICATIONS
Several second-line agents are recommended generally based on the positive results of a single randomized controlled trial or inconsistent results of multiple randomized controlled trials. (45) Other anticonvulsants, particularly carbamazepine and lamotrigine, have shown some efficacy in various chronic NP disorders. The benefits of clonazepam, phenytoin, and valproic acid are uncertain. Many of the second-line agents are limited by side effects (TABLE 2). (45,48,50,51)
Various antidepressants other than the tricyclic antidepressants are developing a limited role in the management of chronic NP. The SSRI paroxetine may offer benefit, although its use has been associated with extrapyramidal-like movement disorders. Bupropion, citalopram, mirtazapine, and venlafaxine also show promise and appear to be better tolerated and have fewer side effects than do the tricyclic antidepressants. (45,51,52)
Capsaicin, eutectic mixture of local anesthetics (EMLA) cream, (53) and salicylates (54) are other topical agents that have limited data suggesting some benefit in chronic NP. Of these 3 agents, capsaicin cream appears most promising, (55) although the need for several doses per day and the intense burning and redness at the application site with the high strength needed (7.5%)limit patient acceptance. (51,53)
* COMBINATION THERAPY
Most patients with chronic NP will require more than one drug to achieve adequate pain control. There are no studies that have systematically examined the efficacy of the various possible combinations of the 5 first-line medications compared with monotherapy. (45) Despite this lack of data from controlled clinical trials, the use of combinations of 2 or more of these first-line medications can be recommended when patients have a partial response to 1 as a single agent. A combination also is reasonable at the beginning of treatment to increase the likelihood of a beneficial response or when a medication that requires titration to reach an effective dosage also is being used.
There is, at best, limited data to guide which combinations may work best. Several approaches, not necessarily mutually exclusive, seem reasonable. One approach is to use drugs that have an established clinical benefit for the type of pain. A second approach is to use agents that also are effective in treating existing comorbidities, especially those that may contribute to the pain disorder. The third approach is to use medications that are thought to work via different mechanisms of action, (56,57) as is often done in the management of diabetes mellitus and essential hypertension. Regardless of the approach, side effects, drug interactions, ease of use, and cost must also be considered.
* MANAGEMENT OF SELECTED CHRONIC NEUROPATHIC PAIN DISORDERS
The selection of the medication(s) to manage chronic NP remains relatively challenging for the reasons already discussed. To assist in this process, Galer and Dworkin have made step-wise recommendations for the management of several chronic neuropathic pain disorders (TABLE 3). (48) Also included are recommendations for treatments to avoid because of lack of demonstrated efficacy and/or toxicity.
* NONPHARMACOLOGIC MANAGEMENT
Chronic pain can have significant impact on a patient's quality of life. Conversely, the patient's psychologic outlook, as well as the socioeconomic environment, can have a dramatic impact on the short- and long-term effectiveness of pain management strategies. The assessment of mood, physical disability, pain-coping strategies, and social support are necessary to determine other modalities of treatment that may be needed in conjunction with medication (see Dr Brunton's article).
* BIOFEEDBACK, HYPNOSIS AND COGNITIVE-BEHAVIORAL THERAPIES
Beyond managing psychologic comorbidities that may complicate pain relief, an important management goal is to improve function even in the face of residual pain. Biofeedback, hypnosis, and cognitive-behavioral interventions may be helpful.
Biofeedback training may include specific relaxation strategies, such as progressive muscle relaxation, diaphragmatic breathing or autogenic training by the use of a monitoring instrument that allows the patient to learn to control a physiologic response connected to the pain. (58) Hypnosis uses relaxation combined with imagery to create a state of focused attention. Hypnosis has been shown to be particularly helpful in patients with pain due to cancer.
Cognitive-behavioral therapy seeks to reframe a patient's beliefs that the pain and subsequent disability is out of her/his control. Cognitive-behavioral therapy can reduce pain, increase coping, and reduce behavioral expressions of pain. (59,60) Plans for coping with pain exacerbations should be a part of this therapy to prevent self-defeating behavior during such episodes. [Evidence level: IIIC. Evidence from respected authorities, based on clinical experience, descriptive studies, or reports of expert committees. Poor evidence either to support or to reject the use of a recommendation; clinicians "may or may not follow the recommendation." Available at: http://www.guideline.gov/ summary/summary.aspx?ss=15&doc_id=3 365&nbr=2591&string=chronic%20AND%20pain.] When used in combination with medications, cognitive-behavioral therapy may lead to a reduction in medication use and overall healthcare services, as well as lead to an improvement in functional activities. In some cases, such as high emotional distress, cognitive-behavioral therapy may need to be initiated prior to medication. Consultation with a psychologist or behavioral therapist should be considered to determine if a patient is in need of these additional therapies.
* NUTRITION AND EXERCISE
Obesity is a major risk factor for OA, thus weight reduction is an important component of comprehensive management. In addition, physical inactivity should be discouraged since this leads to muscular atrophy and further joint instability. (5) In fact, strengthening the muscles that support the affected joint(s) through exercise is critical also. Any physical activity program for older patients should include exercises that improve flexibility, strength, and endurance. [Evidence level: IA. Evidence from at feast one property randomized, controlled trial. Good evidence to support the use of a recommendation, clinicians "should do this all the time." Available at: http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id= 3365&nbr=2591&string=chronic%20AND%20pain.] This is best accomplished by the involvement of physical therapy/occupational therapy specialists.
* REFERRAL
In some cases, referral to a pain specialist should be considered. Possible situations include inadequate pain relief after appropriate trials of several combinations of medications, the need for opioid rotation with methadone, or evidence suggesting opioid abuse.
* SUMMARY
The effective management of chronic pain requires a comprehensive treatment plan consisting of pharmacologic and nonpharmacologic approaches that is often provided by a multidisciplinary healthcare team. The effective management of comorbidities, including those that are psychologic in nature, is critical to successful long-term management of chronic pain. Anti-inflammatory medications are the mainstay of treatment for mild-to-moderate chronic nociceptive pain, with opioids appropriate in patients with moderate-to-severe nociceptive pain. In chronic NP, adjuvant medications are used; first-line recommendations in a recently published evidence-based guideline include gabapentin, the lidocaine patch 5%, opioids, tramadol, and tricyclic antidepressants. Combination therapy generally is required to achieve adequate analgesia in chronic pain disorders. Currently, there have been no systematic studies that have evaluated combinations of agents, and as such, no combinations are clearly preferable in the treatment of chronic NP.
REFERENCES
(1.) Wootton RJ. Psychosocial assessment of chronic pain. In: Warfield CA, Bajwa ZH, eds. Principles and Practice of Pain Medicine. 2nd ed. New York, NY: McGraw-Hill; 2004:148-156.
(2.) Marcus DA. Tips for managing chronic pain. Implementing the latest guidelines. Postgrad Med. 2003;113:49-56, 59.
(3.) Anon. Cancer pain relief. 2nd ed. Geneva, Switzerland: World Hearth Organization; 1996.
(4.) Garcia Rodriguez LA, Hernandez-Diaz S. The risk of upper gastrointestinal complications associated with nonsteroidal anti-inflammatory drugs, glucocorticoids, acetaminophen, and combinations of these agents. Arthritis Res. 2001;3:98-101.
(5.) Anon. Acetaminophen. In: McEvoy GK, ed. AHFS Drug Information. 2000 ed. Bethesda, Md: American Society of Health-System Pharmacists; 2000:1937-1945.
(6.) Grainger R, Cicuttini FM. Medical management of osteoarthritis of the knee and hip joints. Med J Aust. 2004;180:232-236.
(7.) Day R, Morrison B, Luza A, et al. A randomized that of the efficacy and tolerability of the COX-2 inhibitor rofecoxib vs ibuprofen in patients with osteoarthritis. Rofecoxib/Ibuprofen Comparator Study Group. Arch Intern Med. 2000;160:1781-1787.
(8.) Bensen WG, Fiechtner 33, McMillen JI, et al. Treatment of osteoarthritis with celecoxib, a cyclooxygenase-2 inhibitor: a randomized controlled trial Mayo Clin Proc. 1999;74:1095-1105.
(9.) Makarowski W, Zhao WW, Bevirt T, Recker DP. Efficacy and safety of the COX-2 specific inhibitor valdecoxib in the management of osteoarthritis of the hip: a randomized, double-blind, placebo-controlled comparison with naproxen. Osteoarthritis Cartilage. 2002;10:290-296.
(10.) Emery P, Zeidler H, Kvien TK, et al. Celecoxib versus diclofenac in long-term management of rheumatoid arthritis: randomised double-blind comparison. Lancet. 1999;354:2106-2111.
(11.) Simon LS, Weaver AL, Graham DY, et al. Anti-inflammatory and upper gastrointestinal effects of celecoxib in rheumatoid arthritis: a randomized controlled trial. JAMA. 1999;282:1921-1928.
(12.) Laine L, Harper S, Simon T, et al. A randomized trial comparing the effect of rofecoxib, a cyclooxygenase 2-specific inhibitor, with that of ibuprofen on the gastroduodenal mucosa of patients with osteoarthritis. Rofecoxib Osteoarthritis Endoscopy Study Group. Gastroenterology. 1999;117:776-783.
(13.) Goldstein J, Eisen G, Bensen W, et al. SUCCESS in Osteoarthritis (OA) Trial: Celecoxib significantly reduces the risk of upper gastrointestinal (UGI) hospitalizations compared to diclofenac and narpoxen in 13,274 randomized patients with OA. Presented at: European League Against Rheumatism 2001 Annual Meeting, June 13-16, 2001, Prague, Czech Republic.
(14.) Silverstein FE, Faich G, Goldstein JL, et al. Gastrointestinal toxicity with celecoxib vs nonsteroidal anti-inflammatory drugs for osteoarthritis and rheumatoid arthritis: the CLASS study: A randomized controlled trial. Celecoxib Long-term Arthritis Safety Study. JAMA. 2000;284:1247-1255.
(15.) Bombardier C, Laine L, Reicin A, et al. Comparison of upper gastrointestinal, toxicity of rofecoxib and naproxen in patients with rheumatoid arthritis. VIGOR Study Group. N Engl J Med. 2000;343:1520-8, 2.
(16.) Ray WA, Stein CM, Daugherty JR, Hall K, Arbogast PG, Griffin MR. COX-2 selective non-steroidal, anti-inflammatory drugs and risk of serious coronary heart disease. Lancet. 2002;360:1071-1073.
(17.) Mamdani M, Rochon PA, Juurlink DN, et al. Observational study of upper gastrointestinal haemorrhage in elderly patients given selective cyclooxygenase-2 inhibitors or conventional non-steroidal, anti-inflammatory drugs. BMJ. 2002;325:624.
(18.) Ballantyne JC, Mao J. Opioid therapy for chronic pain. N Engl J Mad. 2003;349:1943-1953.
(19.) Jamison RN, Raymond SA, Slawsby EA, Nedeljkovic SS, Katz NP. Opioid therapy for chronic noncancer back pain. A randomized prospective study. Spine. 1998;23:2591-2600.
(20.) Savage SR. Opioid use in the management of chronic pain. Med Clin North Am. 1999;83:761-786.
(21.) Chou R, Clark E, Helfand M. Comparative efficacy and safety of long-acting oral opioids for chronic non-cancer pain: a systematic review. J Pain Symptom Manage. 2003;26:1026-1048.
(22.) Bruera E, Kim HN. Cancer pain. JAMA. 2003;290:2476-2479.
(23.) Vielhaber A, Portenoy RK. Advances in cancer pain management. Hematol Oncol Clin North Am. 2002;16:527-541.
(24.) Bruera E, Pereira J, Watanabe S, Belzile M, Kuehn N, Hanson J. Opioid rotation in patients with cancer pain. A retrospective comparison of dose ratios between methadone, hydromorphone, and morphine. Cancer. 1996;78:852-857.
(25.) Anon. Recommendations for the medical, management of osteoarthritis of the hip and knee: 2000 update. American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Arthritis Rheum. 2000;43:1905-1915.
(26.) Anon. Guideline for the Management of Pain in Osteoarthritis, Rheumatoid Arthritis, and Juvenile Chronic Arthritis. Glenview, Ill: American Pain Society; 2002.
(27.) Anon. The management of persistent pain in older persons. J Am Geriatr Soc. 2002;50(suppl. 6):S205-S224.
(28.) Caldwell JR, Rapoport RJ, Davis JC, et al. Efficacy and safety of a once-daily morphine formulation in chronic, moderate-to-severe osteoarthritis pain: results from a randomized, placebo-controlled, double-blind trial and an open-label extension trial. J Pain Symptom Manage. 2002;23:278-291.
(29.) Caldwell JR, Hale ME, Boyd RE, et al. Treatment of osteoarthritis pain with controlled release oxycodone or fixed combination oxycodone plus acetaminophen added to non-steroidal antiinflammatory drugs: a double blind, randomized, multicenter, placebo controlled trial. J Rheumotol. 1999;26:862-869.
(30.) Roth SH, Fleischmann RM, Burch FX, et al. Around-the-clock, controlled-release oxycodone therapy for osteoarthritis-related pain: placebo-controlled trial, and long-term evaluation. Arch Intern Mad. 2000;160:853-860.
(31.) Goorman SD, Watanabe TK, Miller EH, Perry C. Functional outcome in knee osteoarthritis after treatment with hylan G-F 20: a prospective study. Arch Phys Med Rehabil. 2000;81:479-483.
(32.) Adams ME, Atkinson MH, Lussier AJ, et al. The role of viscosupplementation with hylan G-F 20 (Synvisc) in the treatment of osteoarthritis of the knee: a Canadian multicenter trial comparing hylan G-F 20 alone, hylan G-F 20 with non-steroidal anti-inflammatory drugs (NSAIDs) and NSAIDs alone. Osteoarthritis Cartilage. 1995;3:213-225.
(33.) Anon. Guidelines for the management of rheumatoid arthritis: 2002 Update. Arthritis Rheum. 2002;46:328-346.
(34.) Emery P, Breedveld FC, Dougados M, Kalden JR, Schiff MH, Smolen JS. Early referral recommendation for newly diagnosed rheumatoid arthritis: evidence based development of a clinical guide. Ann Rheum Dis. 2002;61:290-297.
(35.) Bogduk N. Management of chronic low back pain. Med J Aust. 2004;180:79-83.
(36.) van Tulder MW, Scholten RJ, Koes BW, Deyo RA. Non-steroidal anti-inflammatory drugs for low back pain. Cochrane Database Syst Rev. 2000;2:CD000396.
(37.) van Tulder MW, Touray T, Furlan AD, Solway S, Bouter LM. Muscle relaxants for non-specific low back pain. Cochrane Database Syst Rev. 2003;2:CD004252.
(38.) Institute for Clinical Systems Improvement. National Guideline Clearinghouse web site. Adult low back pain. Available at: http://www.guidel.ine.gov/summary/ summary.aspx?ss=15&doc_id=4165&nbr=3190&string=chronic%20AND%20Low%20AND %20back%20AND%20pain. Accessed August 7, 2004.
(39.) van Tulder MW, Malmivaara A, Esmail R, Koes BW. Exercise therapy for low back pain. Cochrane Database Syst Rev. 2000;2:CD000335.
(40.) Furlan AD, Brosseau L, Imamura M, Irvin E. Massage for low back pain. Cochrane Database Syst Rev. 2002;2:CD001929.
(41.) Cochrane Database of Systematic Reviews. Cochrane Database web site. Acupuncture for low-back pain. Available at: http://gateway2.ovid.com/ovidweb.cgi. Accessed August 7, 2004.
(42.) van Tulder MW, Ostelo RW, Vlaeyen JW, Linton SJ, Morley SJ, Assendelft WJ. Behavioural treatment for chronic low back pain. Cochrane Database Syst Rev. 2000;2:C0002014.
(43.) Milne S, Welch V, Brosseau L, et al. Transcutaneous electrical, nerve stimulation (TENS) for chronic low back pain. Cochrane Database Syst Rev. 2001;2:CD003008.
(44.) Nelemans PJ, de Bie RA, de Vet HC, Sturmans F. Injection therapy for subacute and chronic benign low back pain. Cochrane Database Syst Rev. 2000;2:CD001824.
(45.) Dworkin RH, Backonja M, Rowbotham MC, et al. Advances in neuropathic pain: diagnosis, mechanisms, and treatment recommendations. Arch Neural 2003;60:1524-1534.
(46.) Bennett GJ. Neuropathic pain: new insights, new interventions. Hasp Pratt (Off Ed). 1998;33:95-104, 107.
(47.) Schifitto G, McDermott MP, McArthur JC, et al. Incidence of and risk factors for HIV-associated distal sensory polyneuropathy. Neurology. 2002;58:1764-1768.
(48.) Galer BS, Dworkin RH. A Clinical Guide to Neuropathic Pain. Minneapolis, Minn: McGraw-Hill; 2000.
(49.) Guay DR. Adjunctive agents in the management of chronic pain. Pharmacotherapy. 2001;21:1070-1081.
(50.) Backonja M. Anticonvulsants for the treatment of neuropathic pain syndromes. Curr Pain Headache Rap. 2003;7:39-42.
(51.) Macres S, Richeimer S, Duran P. Adjuvant analgesics. In: Warfield CA, Bajwa ZH, ads. Principles and Practice of Pain Medicine. 2nd ed. New York, NY: McGraw-Hill, 2004:627-638.
(52.) Reisner L. Antidepressants for chronic neuropathic pain. Curr Pain Headache Rap. 2003;7:24-33.
(53.) Argoff CE. Targeted topical, peripheral analgesics in the management of pain. Curr Pain Headache Rap. 2003;7:34-38.
(54.) Mason L, Moore RA, Edwards JE, McQuay HJ, Derry S, Wiffen PJ. Systematic review of efficacy of topical rubefacients containing solicylates for the treatment of acute and chronic pain. BMJ. 2004;328:995.
(55.) Mason L, Moore RA, Deny S, Edwards JE, McQuay HJ. Systematic review of topical, capsaicin for the treatment of chronic pain. BMJ. 2004;328-991.
(56.) Beydoun A, Backonja MM. Mechanistic stratification of antineuralgic agents. J Pain Symptom Manage. 2003;25(suppl 5):S18-S30.
(57.) Harden N, Cohen M. Unmet needs in the management of neuropathic pain. J Pain Symptom Manage. 2003;25(suppl 5):S12-S17.
(58.) Haythornthwaite JA, Benrud-Larson LM. Psychological assessment and treatment of patients with neuropathic pain. Curr Pain Headache Rep. 2001;5:124-129.
(59.) Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain. 1999;80: 1-13.
(60.) McCracken LM, Turk DC. Behavioral and cognitive-behavioral, treatment for chronic pain: outcome, predictors of outcome, and treatment process. Spine. 2002;27:2564-2573.
Bill McCarberg, MD
Founder, Chronic Pain Management Program, Kaiser Permanente-San Diego; Assistant Clinical Professor (voluntary), University of California, San Diego School of Medicine
COPYRIGHT 2004 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group