The majority of patients who acquire lung cancer will have troublesome symptoms at some time during the course of their disease. Some of the symptoms are common to many types of cancers, while others are more often encountered with lung cancer than other primary sites. The most common symptoms are pain, dyspnea, and cough. This document will address the management of these symptoms, and it will also address the palliation of specific problems that are commonly seen in lung cancer: metastases to the brain, spinal cord, and bones; hemoptysis; tracheoesophageal fistula; and obstruction of the superior vena cava.
Key words: bone metastases; brain metastases; dyspnea; hemoptysis; interventional bronchoscopy; pain management; pleural effusions; spinal cord metastases; superior vena cava syndrome; tracheoesophageal fistula
Abbreviations: AHCPR = Agency for Health Care Policy and Research; APC = argon plasma coagulation; EBB = endobronchial brachytherapy; NSAID = nonsteroidal anti-inflammatory drug; NSCLC = non-small cell lung cancer; PDT = photodynamic therapy; RCT = randomized controlled trial; SCLC = small cell lung cancer; SVC = superior vena cava; TEF = tracheoesophageal fistula; WBRT = whole-brain radiation therapy
**********
Since the vast majority (86%) of patients with lung cancer will die from their disease, it is intuitively obvious that most such patients will have one or more symptoms during the course of their disease. These symptoms produce a clinically significant alteration in quality of life, and--for many of the symptoms and the specific problems that the symptoms represent--a shortening of the quantity of life. Symptoms that may require palliation include those attributable to the primary lung cancer itself (dyspnea, hemoptysis), regional metastases within the thorax (superior vena cava [SVC] syndrome, tracheoesophageal fistula [TEF], pleural effusions), or from metastases to distant sites (brain, spinal cord, bone). Pain is an ever-troublesome symptom for many patients with lung cancer. Clinicians experienced in managing patients with lung cancer must be conversant with the many different ways to palliate the symptoms that may occur with lung cancer.
This section of the evidence-based guidelines is based on an extensive review of the medical literature. The Agency for Health Care Policy and Research (AHCPR) guidelines for the management of cancer pain was used in an abbreviated form for the guidelines regarding management of pain in lung cancer. Randomized controlled trials (RCTs) have generally not been done for most aspects of palliative care in lung cancer specifically, and meta-analyses are not available. Three RCTs were identified that studied surgical resection for brain metastases and whole-brain radiation therapy (WBRT) for brain metastases. One RCT was identified that studied the effect of corticosteroids in bone metastases, spinal cord compression, and brain metastases, respectively. Most reports of the topics considered in this section were case series.
PAIN CONTROL
A comprehensive document for the management of cancer pain was developed and published in 1994 as part of a response to Public Law 101-239 (the Omnibus Reconciliation Act of 1989), under the aegis of the AHCPR. (1) The comments in this section are adapted from that resource, which was written by a multidisciplinary panel of private-sector clinicians and other experts convened by the AHCPR. Explicit, science-based methods and expert clinical judgment were used to develop specific statements. The scope of that effort is beyond what can be discussed in detail in this document, and the reader is referred to that resource for additional information.
The causes of cancer pain include tumor progression and related pathology (eg, nerve damage), surgery, and other procedures used for treatment and diagnosis, toxic side effects of chemotherapy and radiation, infection, and muscle aches when patients limit their physical activity. Approximately 75% of patients with advanced cancer have pain. Failure to relieve pain leads to unnecessary suffering. Decreased activity, anorexia, and sleep deprivation caused by pain can further weaken already debilitated patients.
Effective management of pain from cancer can be achieved in approximately 90% of patients. Proper management of a patient's pain involves more than analgesia, and the program of pain control for any one patient must be individualized. Approaches that may augment analgesia include cognitive/behavioral strategies, physical modalities, palliative radiation and antineoplastic therapies, nerve blocks, and palliative and ablative surgery.
Any analgesic medication program should be kept as simple as possible, both with regard to the frequency and route of administration. Oral medications are preferred, because of convenience and cost-efficacy. If the patient cannot take medications orally, rectal and transdermal routes should be considered because they are relatively noninvasive. IM routes of administration should be avoided because of the associated pain and inconvenience, and also because of unreliable absorption.
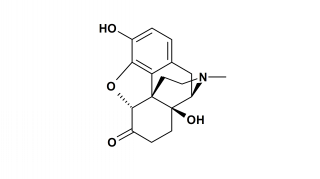
A nonsteroidal anti-inflammatory drug (NSAID) or acetaminophen should be used, unless there is a contraindication to their use. If pain persists or becomes worse, an opioid should be added and not substituted. Using opioids and acetaminophen or NSAIDs often provides more analgesia than can be accomplished by either class of drug alone. Further, the use of acetaminophen or NSAIDs may have a dose-sparing effect for opioids, which can provide the benefit of fewer side effects from the opioids. When pain persists despite this approach, the dose of opioids should be increased or a more potent agent chosen. The World Health Organization ladder has been shown to be an effective method to ensure the rational titration of therapy for cancer pain (Fig 1). (2)
Morphine is the most commonly used opioid for moderate or severe pain. It is available in a wide variety of dosage forms that include immediate and controlled-release preparations. Morphine is relatively inexpensive. Transdermal and rectal routes of administration can be used for most patients who cannot receive medications orally. Morphine, hydrocodone, and oxymorphone suppositories are available. Fentanyl is the opioid most frequently used for transdermal administration. Meperidine should not be administered if it is anticipated that there will be a continuous need for opioid medication. It has a short duration of action, and its metabolite, normeperidine, is toxic and causes CNS stimulation with dysphoria, agitation, and seizures.
Both the cancer patient and family members may shun the use of opioids because of a fear of addiction. Physicians must educate both the patient and the family about pain and how it is to be managed as part of the treatment plan. Effective pain control begins by asking the patient about pain. An easily administered pain rating scale should be used for assessment of pain, both at the time of initial presentation and periodically at regular intervals during the course of the disease. The most common pain scales are numeric (0 to 10 pain intensity), simple descriptive in nature (no pain, mild, moderate, severe), and a visual analog scale.
Analgesic medications should be administered around the clock with extra doses on an as-needed basis, as this approach helps to prevent recurrence of pain. A written pain management plan should be given to the patient with cancer pain. Constipation is a side effect of opioid medications. Constipation should be anticipated, treated prophylactically, and monitored constantly. Mild constipation can be managed by an increase in fiber consumption and a mild laxative such as milk of magnesia. Bulk-forming laxatives such as fiber supplements should be avoided. Unless there are contraindications, cathartic agents should be administered on a regular schedule.
Adjuvant drugs may be used to enhance the efficacy of opioids. Corticosteroids produce effects that include mood elevation, relief of inflammation, and reduction of cerebral or spinal cord edema when there is intracranial metastasis or spinal cord compression. Anticonvulsants such as phenytoin, carbamazepine, and clonazepam are used to manage neuropathic pain. Tricyclic antidepressants are used as an adjuvant to analgesics for the management of neuropathic pain. They augment the effects of opioids and have innate analgesic properties. Their mood-elevating properties may be helpful as an adjuvant to strict analgesics. Other adjunctive pharmacologic approaches include neuroleptics such as the major tranquilizers, hydroxyzine, bisphosphonates, and calcitonin for bone metastases.
There are many different nonpharmacologic methods to manage pain, many of which are very simple, effective, and inexpensive. A list of nonpharmacologic methods to manage pain is outlined in Table 1. For patients with intractable and persistent pain despite use of all modalities that are known and familiar to the practitioner, referral to a clinic that specializes in the management of pain should be considered. Pain-control specialists can help to select additional methods that may improve the overall palliation of pain.
Recommendations for Pain Control
1. All patients and their families must be reassured that pain can be relieved safely and effectively. Level of evidence: good; net benefit: substantial; grade of recommendation: A
2. All patients should be questioned about their pain, and the patient's self-report of pain should be the primary source of assessment. Simple rating scales for pain should be used to assess pain for all patients, and to document the effectiveness of pain management at regular intervals during treatment. Level of evidence: good; net benefit: moderate; grade of recommendation: B
3. For all patients, medications that are used to control pain should be individualized. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
4. For all patients, medication administration should be simple and noninvasive, whenever possible. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
5. For all patients, mild-to-moderate pain should be managed initially with acetaminophen or an NSAID, assuming there are no contraindications to their use. Opioids should be administered when pain is more severe or when it increases. Level of evidence: good; net benefit: substantial; grade of recommendation: A
6. For patients with persisting pain, the dose of opioid or its potency should be increased. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
7. For patients with pain not controlled by pure analgesic medications, adjunctive medications such as tricyclic antidepressants, anticonvulsants, and neuroleptic agents will often augment the effects of pure analgesic medications. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
8. For patients who require medications to control cancer pain, the medications should be administered around the clock with additional as-needed doses. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
9. For any patient, if it is anticipated that there will be a continuous need for opioid medication, meperidine should not be used. It has a short duration of action, and its metabolite, normeperidine, is toxic and causes CNS stimulation with dysphoria, agitation, and seizures. Level of evidence: fair; net benefit: none; grade of recommendation: D
10. For all patients, medications should be administered orally because of convenience and cost-effectiveness. If medications cannot be administered orally, rectal and transdermal routes are preferred because they are relatively noninvasive. Level of evidence: fair; net benefit: small; grade of recommendation: C
11. For all patients, medications should not be administered IM because of pain and inconvenience, and because IM medications are not reliably absorbed. Level of evidence: fair; net benefit: none; grade of recommendation: D
12. For all patients receiving opioids, constipation is common and it should be anticipated, treated prophylactically, and constantly monitored. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
13. All patients should be given a written pain management plan. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
14. All patients should be encouraged to remain active and to care for themselves whenever possible. Prolonged immobilization should be avoided whenever possible. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
15. For patients whose pain is associated with muscle tension and spasm, cutaneous stimulation techniques such as heat and cold applications should be offered for pain relief. Level of evidence: poor; net benefit: small; grade of recommendation: C
16. For all patients, psychosocial methods of care should be introduced early in the management plan, but they should not be regarded as a substitute for analgesia. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
17. For interested patients and family, pastoral care should be encouraged. Level of Evidence: poor; net benefit: moderate; grade of recommendation: C
18. When patients have metastases that have caused pain, palliative radiation therapy should be offered. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
19. For all patients with pain, referral to a specialized pain clinic should be considered. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
PALLIATIVE TREATMENT OF BONE METASTASES
Metastatic lung cancer to bone is a manifestation of stage IV disease, and it is an indication that care for the patient will be palliative in nature. Elimination of pain is the primary goal of treatment options. There are no randomized prospective studies that directly compare radiation to pharmacotherapy for the management of pain due to bony metastasis. If a metastasis occurs in a weight-bearing bone, prophylactic surgical stabilization should be considered before a pathologic fracture occurs.
Pain caused by bone metastases has multiple causes. Periosteal inflammation and elevation is the most common mechanism behind the bone metastasis. Lung cancer metastases to bone are predominately lyric. After controlling pain with pharmacologic methods, treatment should be directed at managing inflammation. External beam radiation should therefore be considered as the initial nonpharmacologic method. This technique uses energy to diminish the local inflammatory response and thereby eliminate the source of the pain. Other nonpharmacologic methods to manage pain from bone metastases include radioactive isotope infusion, supportive measures for pain management, and direct local management (surgery, nerve blocks, etc).
Ninety percent of patients with symptomatic bone metastases obtain some pain relief with a low-dose, brief course of palliative radiation therapy. One half of the responding patients may have complete pain relief. (3) For short-term improvement in bone pain, 8 Gy in a single fraction is as effective as higher doses. (4,5) Although a single dose of radiation may be effective, the duration of pain relief is less than with higher fractionated doses of radiation therapy. Also, if large fields are required, local inflammation and edema may be a problem with a high single dose. A high single dose is more appropriate for small extremity fields, provided internal organs are not included, and for patients whose expected survival is only a few months.
There is a suggestion that different lung cancer cell types that metastasize to the bone may have different responses to radiation therapy. For example, 72% of metastatic adenocarcinoma has been reported to respond as compared to 40% of patients with metastatic squamous cell carcinoma. (6) Most studies do not delineate between cell types but rather separate only small cell lung cancer (SCLC) from non-small cell lung cancer (NSCLC). The reported response to radiation therapy for bony metastases is 75 to 100% for complete to partial relief of pain. (7-11)
A prospective randomized study compared the addition of methylprednisolone with external beam radiation therapy to radiation therapy alone for bone metastases. The group treated with the combination of methylprednisolone and radiation had more rapid and longer duration relief of pain. Stratification was used based on the hydroxyproline/creatinine ratio of [greater than or equal to] 3.6 mg/g). Patients with a higher ratio had more improvement with the combination of external beam radiation and methylprednisolone. (12)
IV radioisotope infusion can also be used to manage pain from bony metastases. Ethylenediamine tetramethylene phosphonic acid is one such agent. Like many of the studies of different methods to treat bone metastases, only a small number of the patients in the reviewed studies had pain due to metastatic lung cancer; this constrains our interpretation of the results. Pain relief was achieved in 83 to 93% of patients treated in this fashion. (13,14) Patients with breast cancer responded better than patients with lung cancer, but bone metastases from lung cancer respond better than other primary sites. (15)
Other radiopharmaceuticals that have been tried for metastatic cancer to bones include strontium-89 chloride. Response rates vary considerably, with some studies identifying little improvement (16) and others demonstrating a 77% response rate. (17) Re-186 hydroxyethylidene diphosphonate has been studied in patients with bony metastases, and was found not to be effective in patients with lung cancer. (18) Significant data and support are limited for these techniques except in case report format.
Adjunctive therapy with disodium pamidronate has demonstrated good therapeutic response by itself, but more importantly when it is used in combination with radiotherapy for bony metastases. Response rates of 92% were seen in a randomized study with external beam radiation and pamidronate, vs radiation alone (83%), pamidronate alone (85%), or pamidronate in combination with chemotherapy (87%). (19) An evidence-based review of the use of this medication provided similar conclusions. (20)
Calcitonin, both porcine and salmon, has been studied in patients with bone pain. Porcine calcitonin was used after failure of radiotherapy and analgesics, with reduction in pain demonstrated in 63% of patients. (21) Salmon calcitonin was studied in different treatment schedules to identify proper dosing regimens for the management of bony pain due to metastatic NSCLC. (22)
Other techniques of pain management that have been tried all have limited evidence-based data and are case series with mixed cancer populations. Percutaneous ethanol injection into metastatic lesions under CT guidance was associated with a reduction in analgesic need in 74% of patients. (23) As cancers are highly vascular, 88% of patients who were treated by embolization of the bone tumor vasculature in a small case series had reduced pain. (24)
Pathologic fractures may occur when lung cancer metastasizes to bones. Fracture of long bones significantly impairs functional status and quality of life. The femur is at special risk because of its role in weight bearing, and surgical intervention may be needed. Other bones that may require palliative surgical intervention include the tibia, hip (proximal femur plus acetabulum), vertebrae, and the humerus.
Prophylactic surgery is recommended for the following situations when long bones are involved: persistent or increasing local pain despite the completion of radiation therapy; a solitary well-defined lytic lesion circumferentially involving > 50% of the cortex; involvement of the proximal femur associated with a fracture of the lesser trochanter; and diffuse involvement of a long bone. (25) Contraindications to surgical treatment of metastatic disease to long bones include a survival expectancy < 4 weeks, and a poor general condition that is an obstacle to a safe operation. (26)
No randomized prospective controlled trials have compared surgery alone, surgery plus radiation therapy, or radiation therapy alone for metastatic longbone disease. All series that have analyzed operative intervention have included metastatic bone disease from multiple primary organ sites, with breast cancer as the most common. Lung cancer usually is the second most common primary site in reported series. A retrospective study of 60 patients compared adjuvant surgery plus radiation therapy (35 sites) to 29 sites that were treated with surgery alone. Univariate analysis revealed that combined therapy (p = 0.02) and prefracture functional status (p = 0.04) were the only predictors of patients achieving a good functional status after surgery. On multivariate analysis, only postoperative radiation therapy was significantly associated with attaining a good level of function after surgery (p = 0.02). (26)
Intramedullary nailing is generally regarded as the preferred operative approach to deal with metastatic long bone disease. An ex vivo biomechanical analysis of the forces required to fracture the humerus after fixation of 50% hemicylindrical cortical central third defects showed that intramedullary nailing was significantly better than dynamic compression plating. (27) In general, endoprostheses and total arthroplasty are required only for intracapsular or very proximal lesions. (28) Operative intervention for metastatic fractures of long bones provides a good functional result in approximately 80 to 85% of patients; a good analgesic effect is accomplished in nearly all patients.
Recommendations for Management of Bone Metastases
20. For patients with bone metastases, external radiation therapy is indicated to control localized pain. Higher fractionated doses of external radiation therapy provide the most predictable and longer lasting pain relief for bone metastases. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
21. For most patients with pain from bone metastases, a single large fraction of external radiation will provide pain relief, but this technique is best reserved for patients with survival expectancy < 3 months and for smaller extremity lesions. Level of evidence: fair; net benefit: small; grade of recommendation: C
22. For patients with bone metastases, systemic corticosteroids (prednisone, 20 to 40 mg/d), when used together with external beam radiation, may augment pain relief. Level of evidence: fair; net benefit: small; grade of recommendation: C
23. In patients who do not respond to external beam radiation for the relief of pain caused by bony metastases, bisphosphonates can be administered alone or as an adjunct to external radiation therapy for bone metastases. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
24. For patients with bone metastases for whom external radiation is not effective, calcitonin may provide pain relief. Level of evidence: poor; net benefit: small; grade of recommendation: C
25. In patients with bone metastases, a variety of radiopharmaceuticals are available to treat pain. They should be considered when analgesics and external radiation therapy fail to control pain. Level of evidence: poor; net benefit: small; grade of recommendation: C
26. In patients with bone metastases, if survival is expected for > 4 weeks and general health status is satisfactory, surgical fixation of a symptomatic or an asymptomatic metastasis to long and/or weight-bearing bones is indicated to minimize the potential for a fracture. Intramedullary nailing is the preferred approach, especially for the femur or the humerus. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
PALLIATIVE TREATMENT OF SPINAL CORD COMPRESSION
Spinal cord compression by epidural tumor is an important complication for many patients with lung cancer, with an estimated frequency of 5% based on autopsy data. (29) Spinal cord compression can be classified anatomically as intramedullary, leptomeningeal, and extradural. No studies focus on functional results of treating intramedullary or leptomeningeal compression of the spinal cord; paraplegia and death occur rapidly in almost all such cases, and treatment is merely supportive. Early detection of epidural metastases with compression of the spinal cord and prompt treatment appear to favorably affect out come. Epidural spinal cord compression is defined as compression of the dural sac and its contents (spinal cord and/or cauda equina) by an extradural tumor mass. The minimum radiologic evidence for cord compression is indentation of the theca at the level of clinical features, which include any or all of the following: pain (local or radicular), weakness, sensory disturbance, and/or evidence of sphincter dysfunction.
There is good evidence to support the use of high-dose dexamethasone (64 mg/d). One welldesigned RCT compared high-dose dexamethasone to no dexamethasone in malignant spinal cord compression treated with radiation therapy alone. (30) Eighty-one percent of patients in the high-dose dexamethasone treatment arm who were ambulatory before treatment remained ambulatory after treatment, compared with 63% in the control arm. In patients who are paretic or paraplegic before treatment, there is a lesser likelihood that gait function will be regained, but the addition of dexamethasone appears to improve the probability of regaining the ability to ambulate. Significant side effects occur in 11% of those who receive high-dose dexamethasone. High-dose dexamethasone is therefore recommended as an adjunct to radiation therapy in retaining or restoring ambulation after treatment, but with a relatively high incidence of serious side effects that must be accepted. There is inconclusive evidence to support the use of moderate-dose dexamethasone (16 mg/d) plus radiation therapy for malignant epidural spinal cord compression. (31) Methylprednisolone has not been compared to dexamethasone in head-to-head studies.
The evidence for radiation therapy with subclinical epidural spinal cord compression is fair, and a combination of high-dose steroids plus radiation should be administered to patients who are not paretic and ambulatory. (32) The dose prescription should be left to the discretion of the prescribing radiation oncologist, as no study has stratified the results by dosing protocol. Most lesions can be managed with nonoperative aggressive treatment aimed at shrinking tumor size and halting growth of the tumor. There is reasonable evidence that there is a difference in relapse rates between those who receive prophylactic radiation and those who do not for patients with asymptomatic epidural spinal cord compression, but the optimal screening process has not been elucidated. (31)
Surgical intervention is limited to specific indications, including spinal instability, progressive neurologic deterioration from bony collapse and compression, intractable pain, and failure of conservative treatment. (32) Laminectomy alone was once the intervention of choice, but it was associated with a high rate of spinal instability and inferior ambulatory outcomes compared with radiation therapy alone. Vertebral body resection with stabilization has the advantage of maintaining the structural integrity of the spine and removing the bulk of bony disease. There is, however, a higher complication rate and perioperative mortality. No study has evaluated these techniques against each other.
Radiation therapy alone should be the first line of treatment for patients who are ambulatory. When there is spinal instability, bony compression, or paraplegia at the time of presentation, surgery should be performed first. In a retrospective analysis of 123 patients treated at a single institution between 1970 and 1996, the major wound complication rate for patients who had radiation before surgical decompression and stabilization was 32%, as compared with 12% for patients whose surgery was done first (p < 0.05). Patients treated initially with surgery had better functional outcomes, with 75% of ambulatory patients remaining ambulatory and continent 30 days after treatment, compared to 50% for those whose surgery followed radiation. (33) The type of surgical decompression depends on the topography of the metastasis: when the anterior or middle column are involved, an anterior decompression should be performed. When the posterior column is involved, a posterior approach may be preferred. A combined approach may be needed when circumferential involvement is present. Reconstruction (cement or prosthesis) is often needed. (34,35) Both surgical and radiation therapy specialties recommend the routine use of surgery for patients with bony compression and for surgical salvage after progression on radiation therapy. (27)
Recommendations for the Palliation of Epidural Spinal Cord Metastases
27. For patients with epidural spinal cord metastases, prompt treatment favorably affects outcome and should be given to all such patients. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
28. For patients who are not paretic and ambulatory, a combination of high-dose steroids plus radiation should be administered. High-dose dexamethasone (64 mg/d) is recommended as an adjunct to radiation therapy in retaining or restoring ambulation after treatment, but with a relatively high incidence of serious side effects that must be accepted. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
29. For patients with asymptomatic epidural spinal cord compression, prophylactic radiation should be prescribed. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
30. For patients with epidural spinal cord compression and spinal instability, progressive neurologic deterioration from bony collapse and compression, intractable pain, and failure of conservative treatment, surgical intervention is indicated. Progression of neurologic deficit while patients are receiving radiation is also an indication for surgical stabilization. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
31. When there is spinal instability, bony compression, or paraplegia at the time of presentation, surgery should be performed first and should then be followed by radiation. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
PALLIATIVE TREATMENT OF BRAIN METASTASES
Brain metastases are more common from lung cancer than from any other primary site. Brain metastases from NSCLC occur in approximately one third of patients, and brain metastases occur in [greater than or equal to] 40% of patients with SCLC. (36,37) If patients with brain metastases are not treated, neurologic deterioration occurs quickly. (38,39) There are four methods currently available to treat patients with metastatic lung cancer to the brain: (1) systemic corticosteroids, used to ameliorate the brain edema that typically accompanies intracranial metastases; (2) WBRT; (3) surgical resection of the metastasis; and (4) stereotactic radiosurgery.
Treatment with systemic glucocorticoids is known to improve neurologic function only for a short time (maximum 1 month). (40) Two thirds of patients will have improvement in their neurologic signs and symptoms with the use of steroids. (41) Dexamethasone is the most commonly used glucocorticoid, because it has minimal mineralocorticoid activity as compared with other steroids. Conventional dosing with dexamethasone for brain tumor edema is [greater than or equal to] 16 mg/d. (42-44) When dexamethasone is administered in these doses for > 1 month, serious side effects are common. (45) Two consecutive, randomized, double-blind, prospective controlled trials of patients with brain metastases and Karnofsky scores [less than or equal to] 80 compared dexamethasone, 8 mg/d, or dexamethasone, 4 mg/d, to dexamethasone, 16 mg/d. (46) Lower doses of dexamethasone were equally effective for improvement in quality of life as compared with patients treated with 16 mg/d, with significantly fewer toxic side effects (cushingoid facies, peripheral edema, steroid-induced myopathy) than in the group receiving 16 mg/d (p < 0.03). One other study (nonrandomized and nonblinded) also reported on the effect of lower doses of dexamethasone; there were similar benefits from lower doses and fewer toxic side effects. (47) In a small pilot study, 12 patients with intracranial metastases were initially administered 24 mg of dexamethasone IV q6h for 48 h, and then randomized to receive either 4 mg of dexamethasone po q6h for approximately 2 weeks during brain irradiation or no further dexamethasone during the radiotherapy. (48) Withholding steroids during the radiotherapy did not result in pronounced deterioration of general performance status or neurologic function at the conclusion of treatment or in reduction in overall survival. A multi-institutional prospective trial is needed to perform adequate statistical evaluation of patients regarding the role of steroid therapy in managing intracranial metastases. Until such a study is done, the consensus of opinion holds that dexamethasone, 16 mg/d, should be administered for 4 weeks, during the time of WBRT, and that it should then be rapidly tapered and discontinued.
Because of the frequency with which brain metastases occur in patients with SCLC, prophylactic WBRT is routinely indicated in patients with limited stage disease who achieve either a complete or a near complete response in the thorax following combined radiation and chemotherapy. When intracranial metastases are known to be present with SCLC, WBRT is again the primary method for palliating symptoms.
Patients with more than one intracranial metastasis from NSCLC are generally treated with WBRT. Median survival with this approach is 3 to 7 months, depending on prognostic factors. (49)
Currently, there are three treatment options available for patients with a known NSCLC and a solitary intracranial metastasis: surgical resection, external beam WBRT, and stereotactic radiosurgery (50) (see also chapter on special treatment issues in this guideline). Most often, some combination of these methods of treatment is preferable. Almost all studies of patients with solitary intracranial metastases that have compared two or more methods of treatment have included patients with tumors from a variety of primary sites, not solely lung cancer. Lung cancer is almost always the most common primary site in these studies; SCLC is usually an exclusion criterion. Whereas data analyses are done on the group as a whole, it is reasonable to apply the conclusions to the subset of NSCLC patients with solitary intracranial metastases.
Two randomized, prospective, controlled trials have demonstrated a better outcome for a combination of WBRT plus surgical resection over WBRT alone. (51,52) Surgery is appropriate for a solitary metastasis in patients with good functional status and a surgically accessible lesion. Median survival for the patients treated with combination therapy was significantly better in both studies as compared with WBRT alone (a third randomized trial failed to show a benefit from surgery, but more patients with active systemic disease were included in this study (53)). In one of the two studies that showed a significant difference in median survival for the combined approach, the differences were most pronounced for patients with stable extracranial disease. (52)
The rationale for adding WBRT to surgical resection in the setting of a solitary brain metastasis is based on the notion that micrometastases cannot reliably be detected with current technology. A randomized, prospective, controlled trial that compared postoperative WBRT plus surgical resection to surgery alone demonstrated that recurrence of tumor anywhere in the brain was less frequent in the WBRT group than in the observation group (18% vs 70%, p < 0.001). (54) The time to any brain recurrence was also significantly longer in the WBRT group. Overall survival was not different between the two groups; thus, postoperative radiotherapy prevented death due to neurologic causes but death due to systemic cancer was more frequent.
There are no significant differences among various conventional radiation therapy fractionation schemes (20 Gy in 5 fractions, 30 Gy in 10 fractions, 40 Gy in 20 fractions). A common dose of radiation therapy administered is 30 Gy given at 3 Gy per fraction in 10 fractions. A more protracted schedule is used for patients who have limited or no evidence of systemic disease or those who have undergone resection of a single brain metastasis, since these patients have the potential for long-term survival or even cure. (55,56) Side effects of WBRT may include measurable deterioration of neuropsychological function.
Stereotactic radiosurgery utilizes a stereotactic fixation system and noncoplanar convergent beams that create a very sharp peripheral dose fall-off along the edge of the target. Thus, the surrounding normal tissues are spared while the radiation kills the tumor cells; accordingly, a single large fraction of ionizing radiation can be administered, making this method of treatment an attractive alternative to treat lesions whether surgically accessible or not. Stereotactic radiosurgery is usually restricted to lesions < 3 cm in diameter.
No randomized prospective trials have compared stereotactic radiosurgery to surgery. Many studies of stereotactic radiosurgery for patients with intracranial metastases have reported similar median survival times to surgery as reported by others. (57-61) A retrospective study has demonstrated equal local tumor control rates and equal neurologic death rates between surgery and stereotactic radiosurgery. (62) A prospective but nonrandomized study of patients with lung cancer (both SCLC and NSCLC) demonstrated significantly longer median survival for stereotactic radiosurgery with or without WBRT over WBRT alone (10.6 months and 9.3 months vs 5.7 months, p < 0.0001). (63) A randomized study of WBRT alone vs WBRT plus stereotactic radiosurgery in patients with two to four intracranial metastases showed significantly improved local control with a trend toward increased survival for WBRT plus stereotactic radiosurgery. (64) Stereotactic radiosurgery can be performed after brain recurrence in patients who previously have had WBRT, surgical excision of a metastasis, or both. Median survival in a case series of patients with lung cancer whose brain metastases were treated with stereotactic radiosurgery alone was 13.9 months, 14.5 months for stereotactic radiosurgery plus WBRT, and 10 months for patients treated with stereotactic radiosurgery for recurrent brain metastases. (65)
Recommendations for Palliative Treatment of Brain Metastases From Lung Cancer
32. Patients with symptomatic brain metastases should be treated with dexamethasone, 16 mg/d, for 4 weeks, during the course of WBRT; dexamethasone should then be rapidly tapered and discontinued. Level of evidence: good; net benefit: moderate; grade of recommendation: B
33. Patients with multiple brain metastases from lung cancer should be treated with WBRT. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
34. For patients with intracranial metastases that are not surgically accessible, or when two to four intracranial metastases are present, or for intracranial recurrence after surgery, stereotactic radiosurgery, accompanied by WBRT, can also be offered. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
PALLIATION OF DYSPNEA AND COUGH
Dyspnea is a subjective experience of difficult, labored, and uncomfortable breathing. Dyspnea is a common symptom of lung cancer, is most prevalent in advanced disease, and may present as "air hunger." Dyspnea and cough are the most commonly reported symptoms in lung cancer, with 15% of patients having dyspnea at diagnosis and 65% at some point during their illness. (66,67) One major cancer center in the United States reported that dyspnea was the fourth most common symptom among patients with cancer who presented to the emergency department. (68) A prospective cohort study of seriously ill, hospitalized adults in five teaching hospitals in the United States reported that among 939 patients with stage III or IV NSCLC, severe dyspnea was recorded in 32%. (69) Patients with lung cancer presenting to emergency departments with dyspnea have a much shorter survival than patients with other malignancies. (68) One study of 120 patients with stage I through IV lung cancer used a questionnaire to evaluate the importance of dyspnea and observed that 87% had dyspnea, and patients with high dyspnea scores had lower quality of life. (70)
The causes of dyspnea in patients with lung cancer can be classified into five broad groups: (1) the result of direct involvement of the respiratory system by lung cancer, (2) the result of indirect respiratory complications caused by lung cancer (postobstructive pneumonia, pleural effusion, etc), (3) the result of specific therapies to treat lung cancer (radiation-induced and chemotherapy-induced lung toxicity, anemia, etc, (4) the result of respiratory complications that occur more frequently in these patients (pulmonary embolism, lung infections, etc), and (5) comorbid conditions (COPD, heart failure, prior lung resection, malnutrition, etc).
Irrespective of the stage of lung cancer, dyspnea usually impacts the patient's physical, social, and psychological well-being. Anxiety, fear of impending death, and pain caused by lung cancer are among the factors that contribute to the subjective symptoms of dyspnea. A prospective study of 100 terminally ill cancer patients (49 patients with lung cancer) observed that dyspnea, measured on visual analog scale, was significantly associated with anxiety (p = 0.001). (71) From the perspectives of the patient and health-care providers, dyspnea can be perceived as panic, chest congestion and tightness, and suffocation. One study of 52 patients with lung cancer noted that both physical and emotional sensations were associated with descriptions of breathlessness, such as the feeling of being unable to get enough breath, or of panic or impending death. (70,72) Increased anxiety has been connected with worse dyspnea in patients with obstructive lung disease, chronic pulmonary disease, and/or cancer. (73-75) One study of 120 patients with stage I through IV lung cancer observed no difference in dyspnea based on cancer stage, cell type, or performance status. However, pain and anxiety scores were higher in patients with high dyspnea scores. (70)
Fatigue is a common symptom among patients with lung cancer, particularly those with advanced disease. One study of 227 cancer patients and 98 control subjects reported that the prevalence of severe fatigue was 15% among patients with recently diagnosed breast cancer, 16% among patients with recently diagnosed prostate cancer, 50% among patients with inoperable NSCLC, and 78% among patients receiving specialist inpatient palliative care. Fatigue was significantly associated with the severity of psychological symptoms (anxiety and depression) and with the severity of pain and dyspnea. (76)
PHARMACOTHERAPY OF DYSPNEA
Pharmacologic treatments for dyspnea caused by lung cancer have included oxygen, bronchodilators, corticosteroids, antibiotics, and opioids. One retrospective study at a medical center specializing in cancer assessed the resource utilization associated with the management of dyspnea caused by lung cancer in 45 patients. The most common therapies administered in the emergency department were oxygen (31%), [[beta].sub.2]-agonists (14%), antibiotics (12%), and opioids (11%). (68)
Bronchodilators
Standard bronchodilators such as [[beta].sub.2]-agonists, anticholinergics, and aerosolized corticosteroids are commonly prescribed to patients with lung cancer who have underlying COPD or asthma. There is no evidence that the presence of lung cancer induces bronchospastic disease. However, the onset of lung cancer in patients with underlying obstructive lung diseases usually aggravates symptoms of preexisting obstructive lung disease. There are not many studies to prove a beneficial effect of bronchodilators in patients with lung cancer. However, a prospective study of 100 terminally ill cancer patients (49 patients with lung cancer) observed that the potentially correctable causes of dyspnea included bronchospasm (in 52%) and hypoxia (in 40%). (71) It is important to ensure that bronchodilator therapy is optimized if the patient has obstructive airways disease.
Corticosteroids
The role for systemic corticosteroids is limited for relieving dyspnea from lung cancer. As is the case with bronchodilator therapy, patients with obstructive airways disease may benefit from treatment with systemic corticosteroids to decrease mucus production and inflammatory changes in the airway mucosa. It is also important to recognize that patients with lung cancer who are actively receiving specific therapy, such as radiotherapy and/or chemotherapy, may have varying degrees of dyspnea. (77) This may reflect pulmonary toxicity to. such therapies. Pulmonary parenchymal toxicity leading to dyspnea may require discontinuation of tumor-specific therapies and administration of systemic corticosteroids.
Oxygen
Supplemental oxygen is perhaps the most commonly prescribed therapy to relieve dyspnea in patients with lung cancer. (68) Significant involvement of the respiratory system by lung cancer or underlying obstructive airways disease usually produces or aggravates dyspnea and hypoxemia. A limited number of studies have shown the beneficial effects of supplemental oxygen therapy. A prospective, double-blind, crossover trial assessed the effects of supplemental oxygen on the intensity of dyspnea in 14 patients with advanced cancer. Patients were randomized to receive either oxygen or air delivered at 5 L/min by mask. Dyspnea was evaluated with a visual analog scale. The results showed that 12 patients consistently preferred oxygen to air, and patients reported little or no benefit from air compared with moderate to much benefit from oxygen. (78)
Irrespective of the oxygenation status, supplemental oxygen therapy should be considered if patients with lung cancer have dyspnea. Multiple blood gas analyses should be avoided to justify oxygen therapy. Percutaneous oximetry should suffice to assess adequate oxygenation.
Analgesics
Dyspnea has been shown to be more severe in patients with severe pain. (70,73) Dyspneic sensation caused or aggravated by cancer-induced pain may respond to nonnarcotic analgesic therapy. However, dyspnea due to pain caused by bony metastases, malignant pleural effusions, or fatigue is unlikely to respond to conventional analgesic therapy. Such circumstances require more aggressive pain control, including palliative radiotherapy for skeletal metastasis. In patients with dyspnea caused by milder pain and discomfort, nonnarcotic analgesics should be tried for a brief period.
Opioid Analgesics
Opioids are frequently used to alleviate dyspnea in patients with advanced lung cancer, advanced obstructive airway disease, and cardiac failure. (79) A wide variety of opioid analgesics have been used to control both dyspnea and pain in patients with cancer of lung and other organs. They include morphine, oxycodone, hydromorphone, and others. Opioids have been used orally, parenterally, and by aerosol. It is unclear if all opioids are equally efficacious in decreasing dyspnea perception in patients with lung cancer. In a study of 104 patients with lung cancer, opioids administered to treat pain did not decrease dyspnea. (70)
An open, uncontrolled study evaluated the role of oral morphine to relieve dyspnea in 15 patients with advanced malignancy receiving standard care and noted that regular, titrated oral morphine may improve dyspnea but can cause significant short-term adverse effects. (79) The relief of dyspnea is usually noted within 24 h and the relief stays at a plateau with continued opioid therapy. (80)
Continuous IV infusion of morphine has been used in patients with terminal lung cancer with severe dyspnea, unrelieved by oxygen, nonnarcotic drugs, or intermittent bolus narcotics. (81) Even when patients achieve good dyspnea relief, the major side effect is sedation. Health-care providers, patients, and family members should be cognizant of the possibility of severe hypoventilation and hypercarbic respiratory failure and death. This side effect also has been described with inhaled morphine. (82)
Other Methods
Nonpharmacologic, noninterventional methods for the control of dyspnea include patient education and intervention by allied health personnel. A multicenter RCT of 119 patients with SCLC or NSCLC or with mesothelioma, who had completed first-line treatment and reported dyspnea, used various strategies. These included breathing control, activity pacing, relaxation techniques, and psychosocial support, in addition to standard management and treatment available for dyspnea. The group assigned to intervention by nurses improved significantly at 8 weeks in breathlessness, performance status, and physical and emotional status compared to the control group. (83,84)
PHARMACOTHERAPY OF COUGH
Cough is a frequent and distressing symptom in patients with lung cancer. Cough can be dry or associated with sputum production. Involvement of any part of the respiratory system can lead to cough. Among the initial symptoms of lung cancer, cough is present in > 65% and productive cough in > 25% of patients. (85) Cough can be the presenting or leading symptom of lung cancer. It is more likely among patients with lung cancer originating in the airways.
All pharmacologic therapies aimed at controlling cough caused by lung cancer are symptomatic. Even if complete cessation of cough is not possible, a significant control of cough may help patients enjoy cough-free periods. In late-stage cancer when no specific therapy can address the cancer itself, control of bothersome cough becomes a problem. The pharmacologic agents available include the following.
Cough Suppressants
Nonopioid cough suppressants may work in a small group of patients with advanced lung cancer. Occasionally, even opioid-resistant cough may respond to agents such as the peripherally acting nonopioid drug benzonatate. (86)
Bronchodilators
Bronchospasm can cause or contribute to cough. If the patient with lung cancer also has underlying bronchospastic obstructive airways disease, then standard bronchodilator therapy may help alleviate the cough.
One study tested the role of inhaled sodium cromoglycate in 20 patients with NSCLC and cough resistant to conventional treatment. The patients were randomized to receive, in a double-blind trial, either inhaled sodium cromoglycate or placebo. The results showed that inhaled sodium cromoglycate reduced cough in all patients with NSCLC. (87)
Opioids
Opioids are the best cough suppressants in patients with lung cancer. Codeine is the most widely used opioid. In advanced stages of lung cancer, standard nonopioid cough suppressants may not control the cough. Intractable or troublesome cough should be treated with opioid agents. Caution should be exercised in prescribing graduated doses of these drugs because of the risk of respiratory suppression and hypoventilation.
A double-blind, RCT regarding the treatment of nonproductive cough was performed in 140 adults with primary lung cancer or metastatic cancer of the lungs. The therapeutic efficacy and the tolerability of a 7-day treatment with levodropropizine drops (75 mg tid) were evaluated in comparison with dihydrocodeine drops (10 mg tid). Efficacy was assessed on the basis of cough severity scores, the number of night awakenings due to cough, and overall estimate of antitussive efficacy. Tolerability was evaluated by laboratory results, vital signs, and any adverse event occurring during the clinical trial, including the presence or absence of somnolence. Subjective cough severity was significantly reduced during treatment with levodropropizine and dihydrocodeine, the antitussive effect and its time profile being similar for both drugs. Also, according to the investigator's evaluation, both levodropropizine and dihydrocodeine treatment produced a significant decrease in cough severity. Concurrently with the relief of cough, the number of night awakenings was decreased significantly by both drugs, with no difference between the two treatments. No change in laboratory test values was considered clinically relevant, and vital signs were not clinically affected. The number of patients reporting adverse events was similar in the levodropropizine group (n = 6) and dihydrocodeine group (n = 4). However, the percentage of patients experiencing somnolence in the group receiving levodropropizine (8%) was significantly lower as compared with that of the dihydrocodeine group (22%). These results confirm the antitussive effectiveness of levodropropizine and suggest a more favorable benefit/risk profile when compared to dihydrocodeine. (88) However, levodropropizine is not available for use in the United States.
Corticosteroids
There are no studies on steroids specifically for cough in lung cancer. If cough is caused by radiation-induced lung problems, then high-dose corticosteroid therapy may relieve a significant degree of cough.
Lidocaine
There are no studies on the role of inhaled lidocaine on cough in patients with lung cancer.
PALLIATION OF DYSPNEA CAUSED BY PLEURAL EFFUSIONS
Malignant pleural effusions occur in 7 to 15% of patients with lung cancer, (89-91) more than half of whom acquire dyspnea. (92) The mechanism of dyspnea with pleural effusions is unclear. Mechanical factors influencing the chest wall, mediastinum, pleural space, and the lung itself all may contribute to the sensation of dyspnea in the patient with a pleural effusion. Several studies have evaluated various aspects of compliance, lung volume, muscle strength, and gas exchange in patients before and after therapeutic aspiration of pleural effusions. (93-98)
When a pleural effusion is identified and suspected as the etiology of dyspnea in a patient with lung cancer, the first requisite is to determine if the effusion is malignant or due to some other cause. The methods for this differentiation have been discussed in another section (see chapter on diagnosis in this guideline).
The major indication for treating a malignant pleural effusion is to relieve dyspnea. Often there are multiple causes of dyspnea in patients with lung cancer, so removal of the pleural fluid may or may not provide adequate relief of dyspnea. Chest radiographs, often including decubitus views, should be assessed to determine if the pleural fluid is free flowing or loculated. Contralateral shift of the mediastinum with large effusions suggests that evacuation of the effusion should provide relief of dyspnea for the patient. The next step is to perform a therapeutic thoracentesis to assess the effects on breathlessness after fluid removal, as well as the rate and degree of reaccumulation of pleural fluid. If the lung is trapped because of parenchymal or pleural disease, there will be minimal relief of dyspnea and the lung will not re-expand. The volume of fluid removed with the initial thoracentesis should be no more than 1 to 1.5 L, stopping earlier should the patient have dyspnea, chest pain, or cough. Removal of larger amounts of pleural fluid may be associated with re-expansion pulmonary edema, particularly if there is coexisting endobronchial obstruction. (99) Although complicated, this technique may minimize the risk of re-expansion pulmonary edema and help assess for the presence of a trapped lung at the time of the diagnostic or therapeutic thoracentesis. (100,101) Pleural pressure monitoring may be a more objective assessment for trapped lung than chest radiograph assessment.
If the initial thoracentesis provides relief of dyspnea and lung re-expansion is seen on postprocedure chest radiography, reaccumulation of fluid can be managed in two basic ways: intermittent therapeutic thoracentesis, or insertion of a chest tube to completely evacuate the pleural fluid, followed by pleurodesis. (99)
Repeated therapeutic thoracentesis is a viable option for patients with poor performance status or with advanced disease. There are no studies that compare repeated thoracentesis to other management approaches. If the malignant pleural effusion continues to accumulate, a more definitive procedure can be considered. Chemical pleurodesis via chest tube or medical thoracoscopy is the most common and effective approach, but pleuroperitoneal shunting, pleural drainage catheters, and systemic therapy are other options.
The overall complete response rate to chemical pleurodesis is 64%. (102) Further analysis according to the type of agent used reveals that fibrosing agents as a group are associated with a 75% complete response rate and that talc, specifically, is associated with a 91% complete response rate. Antineoplastic agents are less often successful, with a reported complete response of 44%. (102) Reported complete response rates to various sclerosing agents are listed in Table 2.
Despite testing a variety of new chemical pleurodesis and intrapleural therapy agents, none appear to have the clinical success rate of talc, nor have most of these agents been tested in a randomized fashion against talc or one of the more commonly used chemical pleurodesis agents. All chemical pleurodesis and intrapleural therapy agents that are available have common as well as their own unique complications and constraints for use, which should be reviewed before a specific agent is chosen.
Pleuroperitoneal shunting is another technique to manage malignant and other intractable pleural effusions. All studies of pleuroperitoneal shunting are case series. Many patients with malignant pleural effusions lack the ability to actively utilize the pumping device, which must be pushed at least 100 times or so daily to overcome the positive peritoneal pressure. (126-130)
Another technique for managing malignant pleural effusions is tunneled long-term catheter drainage of the pleural space. Case series suggest good results for the relief of dyspnea over an extended time in patients with malignant effusions. Although encouraging, many of these studies are retrospective and there has been no comparison to other treatment modalities. (131-133)
The treatment of choice for malignant effusions due to SCLC is systemic chemotherapy. Many patients will respond with resolution of pleural effusions and the associated dyspnea. (134)
BRONCHOSCOPIC METHODS TO PALLIATE DYSPNEA AND COUGH
Introduction
Central airway obstruction refers to significant obstruction of the trachea and main bronchi. Obstruction of lobar bronchi in a patient with limited pulmonary reserve can also lead to considerable respiratory distress. Central airway obstruction in patients with lung cancer can present with life-threatening dyspnea or hemoptysis. Most patients with dyspnea caused by central airway obstruction also complain of cough. The severity of dyspnea is dependent on the extent of luminal involvement of the airway, and the presence or absence of underlying conditions such as COPD, cardiac failure, loss of lung tissue from previous lung surgery, etc.
Extraluminal tumor compression of the major airways, intraluminal tumor growth, or a combination of both can cause central airway obstruction. Perhaps the most important aspect of managing these patients is to first determine the anatomic type of airway involvement. Clinical examination, imaging techniques, and flow-volume curves may provide diagnostic possibilities. However, the single most important diagnostic procedure is bronchoscopy. Bronchoscopy provides visual clues to the nature of the obstructing lesion and the extent of luminal narrowing, and it will determine if an intraluminal or extraluminal process causes the obstruction. It will also help in determining if bronchoscopic therapy is feasible.
Almost all endobronchial therapies are palliative in patients with lung cancer involving the major airways. A small number of patients with in situ lung cancer, who cannot undergo resection because of comorbid conditions, may be cured with endobronchial therapies. The relief of cough is more troublesome because none of the therapies discussed below will totally eradicate the tumor. Thus, even though cough and hemoptysis may be controlled to some extent by these methods, other types of therapy may be required to control cough.
The degree of dyspnea and respiratory distress should dictate the appropriate mode of endobronchial therapy. The currently available methods of bronchoscopic therapy include debulking of intraluminal tumor growth (usually with rigid bronchoscopy), balloon dilatation, laser therapy, electrocautery, cryotherapy, argon plasma coagulation (APC), endobronchial irradiation, or intraluminal stent placement. All of the following therapeutic techniques will provide significant relief of dyspnea and cough in the majority of patients. It should be noted, however, that not all techniques described here will accomplish dyspnea relief quickly (Table 3).
Types of Therapy
Endotracheal Intubation: This should be performed only in a patient who faces impending death because of tracheal obstruction and no bronchoscopic therapy is available. If the obstruction is located in a short segment of trachea and if bronchoscopic examination reveals a lumen, an endotracheal tube (largest diameter feasible) should be inserted so the tip of the tube is beyond the distal aspect of obstruction. Once the airway is secured and oxygenation optimized, then consideration should be given to more definitive therapy. This technique is useful in both luminal and extraluminal obstructions. The risk of bleeding during endotracheal intubation and the difficulty of intubation should be recognized.
Rigid Bronchoscopy: Rigid bronchoscopy is the quickest technique to relieve dyspnea caused by either intraluminal or extraluminal obstruction of major airways. The major advantages include the availability of rigid bronchoscopes of various diameters, ability to maintain an airway, the possibility of delivering oxygen and anesthetic gases, and the ability to employ other therapeutic techniques described below. One retrospective study has evaluated the role of emergency rigid bronchoscopic intervention, including Nd-YAG laser resection or stenting, in patients with acute respiratory failure from malignant central airways obstruction. Airway strictures were caused by primary bronchogenic lung cancer in 14 patients. Urgent bronchoscopic intervention permitted immediate discontinuation of mechanical ventilation in > 52% of these patients (including 19 patients with benign lesions). (136)
The rigid bronchoscope itself can be used as a tumor-debulking instrument, much like coring an apple. In many patients, this alone may suffice to relieve dyspnea. In patients with extraluminal airway obstruction, the rigid bronchoscope is essential to insert silicone stents. A rigid bronchoscope is also helpful in placement of self-expanding metal stents. (137)
Endobronchial Balloon Dilatation: This procedure has a limited role in the treatment of major airway obstruction by malignant tumors. (138) Balloon dilatation, through either the flexible or rigid bronchoscope, is best suited for stenoses that are short in length. (139) Bronchoscopic balloon dilatation may help prepare an obstructed airway for placement of stents.
Laser: Endobronchial laser therapy is useful in relieving obstruction caused by intraluminal lesions. It has no role in treatment of obstruction caused by extraluminal tumors. Either rigid or flexible bronchoscopy can be used for application of laser energy, even though the former accomplishes this more quickly. Currently, various types of lasers are available for treatment of endobronchial tumors. These include Nd-YAG, potassium triphosphate, and C[O.sub.2] laser units. Almost all bronchoscopic laser therapies reported in the literature have employed Nd-YAG laser for therapy of major airway lesions. Immediate relief of airway occlusion and obstructive symptoms can be expected in > 90% of patients. Laser therapy also helps in preparing the airway for insertion of airway stents. Complications from laser therapy include severe hemorrhage, pneumothorax, and pneumomediastinum. (140,141) Disadvantages of laser application are that it requires special training and expensive equipment.
Electrocautery: Electrocautery application through either a rigid or flexible bronchoscope employs alternating electrical current to produce coagulation and vaporization of endobronchial lesions. (142) The rapidity with which the electrocautery technique opens obstructed airway is similar to that achieved with laser therapy. Immediate relief of dyspnea can be achieved with electrocautery in 55 to 75% of patients. (143-147) A prospective study evaluated the impact of bronchoscopic electrosurgery on the need for bronchoscopic Nd-YAG laser in patients with symptomatic airway lesions and observed that of the 47 bronchoscopic electrosurgery procedures, 42 procedures (89%) were successful in alleviating the obstruction, thus eliminating the need for laser. All procedures were performed in the outpatient bronchoscopy suite with the patient under conscious sedation (morphine and midazolam) and topical anesthesia with 2% lidocaine. (148) The advantages of electrocautery include the less expensive equipment (compared to laser) and the ease of use through flexible or rigid bronchoscope. Complications include endobronchial fire, hemorrhage, and inadvertent electrical shock to the operator or patient. Overall, electrocautery seems a good alternative to the more expensive laser therapy.
APC: APC applies a technique to achieve noncontact electrocoagulation of viable tissue. APC utilizes electrically conductive argon plasma as a medium to deliver high-frequency current via a flexible probe to coagulate tissue. APC devitalizes tissue gradually by producing temperatures that coagulate and desiccate tissue. One retrospective study of 60 patients with bronchogenic carcinoma, (43) metastatic tumors of airways, (14) or benign bronchial disease (3) employed APC therapy via flexible bronchoscopy to control hemoptysis, symptomatic airway obstruction, or both obstruction and hemoptysis. Patients with endoluminal airway lesions had an overall decrease in mean obstruction of 18 [+ or -] 22%. All patients with obstructive lesions experienced symptom improvement, and symptom control was maintained during a median follow-up period of 53 days. There were no complications related to APC. The advantages of APC include low cost, noncontact mode of therapy, easy portability of equipment, and ease of use. The noncontact feature of APC allows rapid coagulation with minimal manipulation of and mechanical trauma to the target tissue. The procedure can be performed in an outpatient setting or at the bedside in the ICU. (149)
Cryotherapy: Cryotherapy employs cryoprobes, through either a rigid or flexible bronchoscope, to apply extremely cold temperatures to tumor tissue so that malignant cells are devitalized and killed by repeated cycles of cold application followed by thawing. Nitrous oxide or liquid nitrogen is most commonly used to produce temperatures of -80[degrees]C. (150-152) As is the case with laser and electrocautery, cryotherapy can be used to treat only intraluminal tumors. Subjective improvements have been observed in > 75% of patients with malignant airway lesions. (153,154) The cryotherapy equipment is less expensive and easier to use than laser therapy. Complications are few and minor. Repeat bronchoscopy is needed for continued therapy in many patients. The major disadvantage of treating large tumors in major airways is that cryotherapy requires far more time to relieve obstruction. As a result, cryotherapy is not an ideal therapeutic method to relieve dyspnea caused by major airway lesions.
Stents: Airway prostheses or stents made of metal, silicone, or other materials are available to relieve airway obstruction caused by malignant tumor. (155,156) Stent therapy is applicable to both intraluminal and extraluminal major airway obstructions. Stent therapy is more effective in patients with tracheal or main bronchial diseases than in those with airway diseases that involve lobar and distal bronchi. Either silicone or metallic stents can be used to treat malignant airway lesions. Uncovered metallic stents should not be inserted in patients with malignant airway lesions because the growth of cancer through the wire mesh negates the benefits of stent placement. (137) Even after bronchoscopic debridement of tumor and laser therapy, stent placement should be considered to maintain airway patency. In one study of 22 patients with severe malignant strictures, 34 endobronchial stents were implanted as a temporary measure when patients received irradiation or chemotherapy. Significant improvements of dyspnea and partial oxygen pressure were observed, and in 50% of patients, the stents were removed after successful tumor-specific therapy. (157) In another study, among 34 patients with inoperable malignant airway stenosis, covered metallic stents were implanted on emergent basis in 19 patients (56%) because of life-threatening airway obstruction. Immediate relief of dyspnea was achieved in 82% of the patients, and significant improvements were observed in airway diameter, vital capacity, and peak expiratory flow. (136)
All silicone stents require rigid bronchoscopy for their insertion, manipulation, and removal, (158-160) whereas metal stents can be inserted with the aid of flexible bronchoscopy and/or fluoroscopic guidance. Complications from silicone stents include migration of stent and inspissation of thick mucus within the stent lumen. Metallic stents are more likely to promote growth of granulation tissue.
Brachytherapy: Brachytherapy is employed to deliver radiation therapy from within the airway lumen to treat intraluminal malignant tumors. (161-163) Brachytherapy is aimed at palliating malignant airway lesions in patients who have already received a maximum dose of external beam radiation. Brachytherapy can be used as a stand-alone therapy or as complimentary or combined therapy following external beam radiation therapy, airway debulking (laser, mechanical removal, etc), or after airway stent placement. Even though earlier experience demonstrated that endobronchial brachytherapy (EBB) alone resulted in adequate symptomatic relief in a considerable number of patients,(164-171) current evidence indicates that brachytherapy as a complimentary therapy provides better relief of dyspnea and other symptoms than EBB alone. (168,172-178) Relief from dyspnea can be expected in > 60% of patients and can last for weeks to months. A phase II study involving 30 patients with stage III NSCLC treated with 60 Gy radiation therapy also used EBB and reported palliation rates of 80% for dyspnea and 43% for cough. (179) One prospective study of 342 patients with endobronchial tumors treated by the combination of external beam radiation therapy (30 to 60 Gy) and concomitant EBB during weeks 1, 3, and 5 observed a response rate of 85% for cough and 86% for dyspnea. (178) Major complications of brachytherapy include fistula formation between the airways and other thoracic structures in up to 8% of patients. The risk of massive hemoptysis increases dramatically when a fraction size of 15 Gy is used. (180)
Photodynamic Therapy: Photodynamic therapy (PDT) consists of using tumor-tagging compounds such as hematoporphyrin derivative and Photofrin. When tumor cells thus tagged are exposed to the light of the proper wavelength, chemical reactions cause death of malignant cells through the production of toxic radicals. Patients with small (< 3 [cm.sup.2]) epithelial cell malignancies are most likely to benefit from this therapy. Complete response lasting for > 12 months has been observed in 50% of patients. (181,182) Complications from PDT include phototoxicity, hemoptysis, and obstruction of bronchi by thick necrotic material.
The effectiveness of PDT for symptom palliation and determined survival benefit has been evaluated in patients with advanced inoperable bronchogenic cancer and endobronchial luminal obstruction. Among 100 such patients, 82% had received prior chemotherapy and/or radiotherapy. On an average, endoluminal obstruction diminished from 86 to 18%. This study suggests that PDT is effective in palliation of inoperable advanced lung cancer in a subset of patients. However, the relief from obstruction is slow, (183) and because of this slow response there is no major role for PDT in the treatment of obstructing lesions of major airways.
Surgery: Surgical resection of malignant tracheobronchial tumors should be considered when unusual types of malignant tumors are encountered. The types of tumors that are amenable to resection and anastomosis include carcinoid, cylindroma, and mucoepidermoid tumors. The length of involvement of trachea or major bronchus should be short enough for the surgeon to resect the tumor so that the anastomotic site is free of malignant cells.
Recommendations for Palliation of Cough and Dyspnea
35. In all patients with lung cancer, potentially correctable causes of dyspnea, such as localized obstruction of a major airway, a large pleural effusion, or an exacerbation of coexisting COPD, should be sought initially. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
36. For all lung cancer patients with dyspnea, pharmacologic approaches for the management of dyspnea may include oxygen, bronchodilators, corticosteroids, antibiotics, and opioids. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
37. For all lung cancer patients with dyspnea, nonpharmacologic, noninterventional treatments including patient education and intervention by allied health personnel should be used to help control dyspnea, including breathing control, activity pacing, relaxation techniques, fans, and psychosocial support. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
38. For all patients with lung cancer who continue to have cough, opioids are the best cough suppressants and should be used. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
39. Patients with malignant pleural effusions that cause dyspnea initially should be drained by thoracentesis. Level of evidence: fair; net benefit: substantial; grade of recommendation: C
40. Patients with lung cancer who have poor performance status and limited life expectancy, and with recurring malignant pleural effusions, can be managed with repeated thoracenteses. Level of evidence: fair; net benefit: small; grade of recommendation: C
41. Patients with NSCLC and better performance status and recurrent malignant pleural effusions, and whose lungs re-expand with initial thoracentesis or thoracoscopy, should be followed up by pleurodesis. Level of evidence: good; net benefit: moderate; grade of recommendation: B
42. In patients with SCLC, the treatment of choice for malignant effusions is systemic chemotherapy. Level of evidence: good; net benefit: moderate; grade of recommendation: B
43. For patients with central airway obstruction, bronchoscopy should be done to determine the type of airway obstruction (extraluminal tumor compression of the major airways, intraluminal tumor growth, or both). Level of evidence: fair; net benefit: substantial; grade of recommendation: B
44. In patients with central airway obstruction, rapid relief of dyspnea can be accomplished via bronchoscopy with removal of intraluminal tumor (laser, electrocautery, APC) and/or by inserting a stent. Other methods (cryotherapy, brachytherapy, PDT) are effective but do not relieve dyspnea as quickly. Level of evidence: poor; net benefit: substantial; grade of recommendation: C
PALLIATION OF HEMOPTYSIS
Hemoptysis is the presenting symptom in 7 to 10% of patients with lung cancer. Approximately 20% will have hemoptysis some time during their clinical course, with 3% having terminal massive hemoptysis. (184-187) For patients whose initial presenting symptom is hemoptysis, surgical resection of the bleeding lobe or the entire lung may be appropriate if the cancer is confined to a hemithorax and amenable to surgery with curative intent. Massive hemoptysis, that which most commonly requires intervention, has a broad definition as expectoration of at least 100 to 600 mL of blood in 24 h. Blood clot formation obstructing the airways is suggested as the most common cause of respiratory insufficiency from massive hemoptysis. Massive hemoptysis due to lung cancer has a much poorer prognosis than hemoptysis of other etiologies. The mortality of massive hemoptysis may be as high as 59 to 100% in patients with bronchogenic carcinoma. (188) Surgery, a more definitive therapeutic modality, is not on the algorithm for intervention, as most lung cancer patients with massive hemoptysis have advanced disease and are already nonsurgical candidates.
Because the prognosis for survival is so grim among lung cancer patients who acquire massive hemoptysis, the patient may not want any kind of intervention. If intervention is undertaken, the initial priority in managing massive hemoptysis should be to maintain an adequate airway. (189,190) This usually requires endotracheal intubation, and a single-lumen endotracheal tube is generally more beneficial than a double-lumen endotracheal tube. Selective right or left mainstem intubation can be performed to protect the nonbleeding lung. Double-lumen endotracheal tubes are more difficult to place and position, have smaller lumens, and do not allow a therapeutic bronchoscope to be passed through each side of the tube. This makes it difficult to further control and/or suction the airways. (191)
Bronchoscopy is typically needed to identify the source of bleeding. Endoscopic management of hemoptysis depends on whether the location of bleeding is identified but a specific endoscopic cause for the bleeding is not seen, as opposed to both site and a specific cause of the hemoptysis (eg, bleeding from an endobronchial tumor). When only the location of bleeding is identified but no direct source is found, endobronchial management options begin with tamponade of the segment by continuous suctioning to collapse the segment. (192) Vasoactive drugs such as 1:10,000 epinephrine solution can be instilled, although this is most useful on visualized lesions. (193) Iced saline solution lavage has been proposed as a temporizing technique to control hemoptysis, (194,195) and balloons may be used to tamponade the bleeding site. It is suggested that balloons remain in place for 24 to 48 h to allow tamponade of hemoptysis. (196-199) Use of Nd-YAG photocoagulation is an efficient tool for the management of bleeding endobronchial lesions, with a reported response rate of 60%. (200,201) Electrocautery should produce similar results, but its use to control hemoptysis has thus far been anecdotal. APC provided resolution of hemoptysis in 100% of patients with a 3-month follow-up. (149)
If hemoptysis is determined to arise from an endoscopically visualized lung cancer, bronchial artery embolization may temporize the bleeding. Most reports of bronchial artery embolization are limited by the few cases of lung cancer managed in almost all studies. (202-205)
When bronchoscopy reveals that bleeding is coming from an endoscopically visible, unresectable lung cancer, external beam radiation should be the next consideration. (206) This is true even when other temporizing measures, such as those discussed earlier, have been done. A high-dose initial fraction may provide a more rapid response. Endobronchial radiation has also been reported to be effective for the control of bleeding from visible tumors.
Recommendations for the Palliation of Hemoptysis
45. In managing a patient with massive hemoptysis, the initial priority should be maintaining adequate airway protection. If intubation is required, a standard single-lumen endotracheal tube should be used. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
46. For patients with massive hemoptysis, bronchoscopy is typically needed to identify the source of bleeding. Early bronchoscopy to assess the site of bleeding is recommended. Level of evidence: poor; net benefit: substantial; grade of recommendation: C
47. For patients with massive hemoptysis, endobronchial management options begin with tamponade. Effective adjunctive devices include APC, Nd-YAG laser, and electrocautery. Level of evidence: fair; net benefit: small; grade of recommendation: C
48. For patients with massive hemoptysis due to lung cancer, bronchial artery embolization is a temporizing treatment. Level of evidence: poor; net benefit: small; grade of recommendation: I
49. For patients with massive hemoptysis or persistent large-volume hemoptysis that is determined to arise from an endoscopically visible, unresectable lung cancer, external beam radiation should be considered. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
PALLIATION OF MALIGNANT TEF
TEFs are serious complications of lung and esophageal cancer; TEFs are more common with esophageal cancers than primary lung cancers. Life expectancy with no therapy is estimated at 1 to 7 weeks. Patients have repeated aspiration of food, gastric contents, and saliva. This persistent aspiration leads to patient distress due to coughing and shortness of breath. Patients can acquire recurrent pneumonias with persistent inflammation of the airways. Patients frequently lose weight and become dehydrated be cause they cannot tolerate oral intake. Even with abstinence from eating and drinking, most patients have difficulty with controlling their own secretions.
Curative resection of the involved tracheal-bronchial and/or esophageal segments in face of a malignancy is inappropriate; most such patients are near the end of their lives and palliation should be the primary treatment objective. Esophageal bypass procedures can be considered, but they have very high morbidity and mortality and are inappropriate as palliative tools in advanced lung cancer. The goals of therapy are to restore patency of the trachea, bronchi, and/or esophagus, to prevent spillage of further material into the lung, and ensure that the patient receives nutrition and fluid.
Double stenting of the tracheobronchial tree and the esophagus appears to be the procedure that yields the best overall results for symptomatic relief for patients with this condition. Clinical series have attempted either esophageal or tracheobronchial stenting with mixed results. Most series with higher success rates use a double-stenting technique. (207-209)
The addition of percutaneous enterogastric tube placement can ensure proper nutrition and fluid management for patients with this condition. Patients may be able to eat soft foods once double stenting is performed, but maintaining adequacy of fluid status and nutrition is often difficult.
Recommendations for the Palliative Treatment of Malignant TEF
50. For patients with a malignant TEF or bronchoesophageal fistula, stenting of both the tracheobronchial tree and the esophagus is the procedure that yields the best overall results for symptomatic relief. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
51. For any patient with lung cancer and a TEF, attempts at curative resection of the involved trachea and/or bronchi and/or esophageal segments should not be done. Level of evidence: fair; net benefit: none; grade of recommendation: D
52. For any patient with advanced lung cancer, esophageal bypass procedures have very high morbidity and mortality and should not be done. Level of evidence: fair; net benefit: none; grade of recommendation: D
PALLIATIVE TREATMENT OF SVC OBSTRUCTION
The SVC may become obstructed by lung cancer, either via direct extension or more commonly by regional lymph node metastases. SVC syndrome develops in 10% of patients with a right-sided malignant intrathoracic mass lesion. (210) SVC syndrome includes symptoms that may be severe and debilitating, including congestion of the collateral veins of the neck, anterior chest wall, face, eyelids and right arm. Dyspnea, headache from cerebral venous hypertension, and cyanosis occur less frequently. Typically, lifestyle is significantly impaired with SVC syndrome. Consensus opinion once held that emergency radiation therapy was always necessary to alleviate the symptoms that are secondary to compression of the SVC. However, the need for emergency radiation therapy has been challenged, and many symptomatic patients are better treated by stenting. (211) Intravascular stenting with expandable metallic stents has largely replaced surgical venous bypass to obtain rapid relief of SVC syndrome from malignant obstruction. Balloon angioplasty may be needed initially to enlarge the vascular lumen and allow proper stent placement. When thrombosis occurs as a complication of SVC syndrome, local lytic therapy may be of value to re-establish patency and subsequently to allow insertion of a stent.
There is usually time to obtain a histologic diagnosis, which is important because patients with SCLC are well managed by chemotherapy. (211) Whereas chemotherapy for SCLC may also improve the symptoms associated with SVC syndrome, radiation therapy is usually a part of treating SCLC with SVC obstruction. Patients with SCLC and SVC syndrome undergoing concurrent treatment with chemotherapy and radiation therapy have improved 5-year survival (15 [+ or -] 7%) [mean [+ or -] SD] compared with SCLC patients without SVC syndrome (9 [+ or -] 2%, p = 0.008). (212)
Radiation therapy for SVC syndrome caused by NSCLC is associated with a good symptomatic response in 82% of patients within 1.7 [+ or -] 0.9 weeks (3 days to 4 weeks). (213) In a small series, 10 of 11 patients had complete relief of symptoms within 3 days after stent implantation; they remained symptom free until death in follow-up (17 to 227 days). (214) In a nonrandomized study, expandable metallic stents provided symptom relief (78%) equally often as radiation therapy (80%); mean survival was identical. (215) Patients with intraluminal tumors had a shorter mean survival (45 days) compared with those who had extrinsic compression (199 days). Stent placement was effective in relieving symptoms in patients without a response to radiation therapy. (215)
In another nonrandomized study comparing stent insertion to radiation therapy, faster relief of symptoms and significantly greater improvement in SVC obstruction score were seen with stent insertion (p = 0.0005 and 0.001, respectively). (216) Placement of stents to obtain quick relief of SVC syndrome symptoms does not preclude the use of radiation therapy or chemotherapy. Complications attributable to stent insertion (bleeding due to vascular injury, thrombosis within the stent) may occur in a minority of patients so treated.
Recommendations for Palliation of SVC Obstruction
53. Lung cancer patients with symptomatic SVC obstruction can be treated with radiation therapy, insertion of a stent, or both. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
SUMMARY OF RECOMMENDATIONS
The majority of patients who acquire lung cancer will have troublesome symptoms during the course of their disease. Pain, dyspnea, hemoptysis, and the effects of regional or distant metastases to bones, brain, or spinal cord are common. There are many effective methods available to relieve these symptoms. Familiarity with the palliative approach to care is crucial for a clinician to be competent in caring for patients with lung cancer.
Recommendations for Pain Control
1. All patients and their families must be reassured that pain can be relieved safely and effectively. Level of evidence: good; net benefit: substantial; grade of recommendation: A
2. All patients should be questioned about their pain, and the patient's self-report of pain should be the primary source of assessment. Simple rating scales for pain should be used to assess pain for all patients, and to document the effectiveness of pain management at regular intervals during treatment. Level of evidence: good; net benefit: moderate; grade of recommendation: B
3. For all patients, medications that are used to control pain should be individualized. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
4. For all patients, medication administration should be simple and noninvasive, whenever possible. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
5. For all patients, mild-to-moderate pain should be managed initially with acetaminophen or an NSAID, assuming there are no contraindications to their use. Opioids should be administered when pain is more severe or when it increases. Level of evidence: good; net benefit: substantial; grade of recommendation: A
6. For patients whose pain persists, the dose of opioid or its potency should be increased. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
7. For patients whose pain is not controlled by pure analgesic medications, adjunctive medications such as tricyclic antidepressants, anticonvulsants, and neuroleptic agents will often augment the effects of pure analgesic medications. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
8. For all patients who require medications to control cancer pain, the medications should be administered around the clock with additional as-needed doses. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
9. For any patient, if it is anticipated that there will be a continuous need for opioid medication, meperidine should not be administered. It has a short duration of action, and its metabolite, normeperidine, is toxic and causes CNS stimulation with dysphoria, agitation, and seizures. Level of evidence: fair; net benefit: none; grade of recommendation: D
10. For all patients, medications should be administered orally because of convenience and cost-effectiveness. If medications cannot be taken orally, rectal and transdermal routes are preferred because they are relatively noninvasive. Level of evidence: fair; net benefit: small; grade of recommendation: C
11. For all patients, medications should not be administered IM because of pain and inconvenience, and because IM medications are not reliably absorbed. Level of evidence: fair; net benefit: none; grade of recommendation: D
12. For all patients receiving opioids, constipation is common and it should be anticipated, treated prophylactically, and constantly monitored. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
13. All patients should be given a written pain management plan. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
14. All patients should be encouraged to remain active and to care for themselves whenever possible. Prolonged immobilization should be avoided whenever possible. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
15. For patients whose pain is associated with muscle tension and spasm, cutaneous stimulation techniques, such as heat and cold applications, should be offered for pain relief. Level of evidence: poor; net benefit: small; grade of recommendation: C
16. For all patients, psychosocial methods of care should be introduced early in the management plan, but they should not be regarded as a substitute for analgesia. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
17. For interested patients and family, pastoral care should be encouraged. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
18. When patients have metastases that have caused pain, palliative radiation therapy should be offered. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
19. For all patients with pain, referral to a specialized pain clinic should be considered. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
Recommendations for Management of Bone Metastases
20. For patients with bone metastases, external radiation therapy is indicated to control localized pain. Higher fractionated doses of external radiation therapy provide the most predictable and longer-lasting pain relief for bone metastases. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
21. For most patients with pain from bone metastases, a single large fraction of external radiation will provide pain relief, but this technique is best reserved for patients with survival expectancy < 3 months and for smaller extremity lesions. Level of evidence: fair; net benefit: small; grade of recommendation: C
22. For patients with bone metastases, systemic corticosteroids (prednisone, 20 to 40 mg/d), when used together with external beam radiation, may augment pain relief. Level of evidence: fair; net benefit: small; grade of recommendation: C
23. In patients who do not respond to external beam radiation for the relief of pain caused by bony metastases, bisphosphonates can be administered alone or as an adjunct to external radiation therapy for bone metastases. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
24. For patients with bone metastases for whom external radiation is not effective, calcitonin may provide pain relief. Level of evidence: poor; net benefit: small; grade of recommendation: C
25. In patients with bone metastases, a variety of radiopharmaceuticals are available to treat pain. They should be considered when analgesics and external radiation therapy fail to control pain. Level of evidence: poor; net benefit: small; grade of recommendation: C
26. In patients with bone metastases, if survival is expected for > 4 weeks and general health status is satisfactory, surgical fixation of a symptomatic or an asymptomatic metastasis to long and/or weight-bearing bones is indicated to minimize the potential for a fracture. Intramedullary nailing is the preferred approach, especially for the femur or the humerus. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
Recommendations for the Palliation of Epidural Spinal Cord Metastases
27. For patients with epidural spinal cord metastases, prompt treatment favorably affects outcome and should be administered to all such patients. Level of evidence: fair; net benefit: substantial; grade of recommendation: B
28. For patients who are not paretic and ambulatory, a combination of high-dose steroids plus radiation should be administered. High-dose dexamethasone, 64 mg/d, is recommended as an adjunct to radiation therapy in retaining or restoring ambulation after treatment, but with a relatively high incidence of serious side effects that must be accepted. Level of evidence: air; net benefit: substantial; grade of recommendation: B
29. For patients with asymptomatic epidural spinal cord compression, prophylactic radiation should be prescribed. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
30. For patients with epidural spinal cord compression and spinal instability, progressive neurologic deterioration from bony collapse and compression, intractable pain, and failure of conservative treatment, surgical intervention is indicated. Progression of neurologic deficit while patients are receiving radiation is also an indication for surgical stabilization. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
31. When there is spinal instability, bony compression, or paraplegia at the time of presentation, surgery should be performed first and should then be followed by radiation. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
Recommendations for Palliative Treatment of Brain Metastases From Lung Cancer
32. Patients with symptomatic brain metastases should be treated with dexamethasone, 16 mg/d, for 4 weeks during the course of WBRT; dexamethasone should then be rapidly tapered and discontinued. Level of evidence: good; net benefit: moderate; grade of recommendation: B
33. Patients with multiple brain metastases from lung cancer should be treated with WBRT. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
34. For patients with intracranial metastases that are not surgically accessible, or when two to four intracranial metastases are present, or for intracranial recurrence after surgery, stereotactic radiosurgery, accompanied by WBRT, can also be offered. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
Recommendations for Palliation of Cough and Dyspnea
35. In all patients with lung cancer, potentially correctable causes of dyspnea, such as localized obstruction of a major airway, a large pleural effusion, or an exacerbation of coexisting COPD, should be sought initially. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
36. For all lung cancer patients with dyspnea, pharmacologic approaches for the management of dyspnea may include oxygen, bronchodilators, corticosteroids, antibiotics, and opioids. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
37. For all lung cancer patients with dyspnea, nonpharmacologic, noninterventional treatments, including patient education and intervention by allied health personnel, should be used to help control dyspnea, including breathing control, activity pacing, relaxation techniques, fans, and psychosocial support. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
38. For all patients with lung cancer who continue to have cough, opioids are the best cough suppressants and should be used. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
39. Patients with malignant pleural effusions that cause dyspnea initially should be drained by thoracentesis. Level of evidence: fair; net benefit: substantial; grade of recommendation: C
40. Patients with lung cancer who have poor performance status and limited life expectancy, and with recurring malignant pleural effusions, can be managed with repeated thoracenteses. Level of evidence: fair; net benefit: small; grade of recommendation: C
41. NSCLC patients with better performance status and recurrent malignant pleural effusions, and whose lungs re-expand with initial thoracentesis or thoracoscopy, should be followed up with pleurodesis. Level of evidence: good; net benefit: moderate; grade of recommendation: B
42. In patients with SCLC, the treatment of choice for malignant effusions is systemic chemotherapy. Level of evidence: good; net benefit: moderate; grade of recommendation: B
43. For patients with central airway obstruction, bronchoscopy should be done to determine the type of airway obstruction (extraluminal tumor compression of the major airways, intraluminal tumor growth, or both). Level of evidence: fair; net benefit: substantial; grade of recommendation: B
44. In patients with central airway obstruction, rapid relief of dyspnea can be accomplished via bronchoscopy with removal of intraluminal tumor (laser, electrocautery, APC) and/or by inserting a stent. Other methods (cryotherapy, brachytherapy, PDT) are effective but do not relieve dyspnea as quickly. Level of evidence: poor; net benefit: substantial; grade of recommendation: C
Recommendations for the Palliation of Hemoptysis
45. In managing a patient with massive hemoptysis, the initial priority should be maintaining adequate airway protection. If intubation is required, a standard single-lumen endotracheal tube should be used. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
46. For patients with massive hemoptysis, bronchoscopy is typically needed to identify the source of bleeding. Early bronchoscopy to assess the site of bleeding is recommended. Level of evidence: poor; net benefit: substantial; grade of recommendation: C
47. For patients with massive hemoptysis, endobronchial management options begin with tamponade. Effective adjunctive devices include APC, Nd-YAG laser, and electrocautery. Level of evidence: fair; net benefit: small; grade of recommendation: C
48. For patients with massive hemoptysis due to lung cancer, bronchial artery embolization is a temporizing treatment. Level of evidence: poor; net benefit: small; grade of recommendation: I
49. For patients with massive hemoptysis or persistent large-volume hemoptysis that is determined to arise from an endoscopically visible, unresectable lung cancer, external beam radiation should be considered. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
Recommendations for the Palliative Treatment of Malignant TEF
50. For patients with a malignant TEF or bronchoesophageal fistula, stenting of both the tracheobronchial tree and the esophagus is the procedure that yields the best overall results for symptomatic relief. Level of evidence: poor; net benefit: moderate; grade of recommendation: C
51. For any patient with lung cancer and a TEF, attempts at curative resection of the involved trachea and/or bronchi and/or esophageal segments should not be done. Level of evidence: fair; net benefit: none; grade of recommendation: D
52. For any patient with advanced lung cancer, esophageal bypass procedures have very high morbidity and mortality and should not be done. Level of evidence: fair; net benefit: none; grade of recommendation: D
Recommendations for Palliation of SVC Obstruction
53. Lung cancer patients with symptomatic SVC obstruction can be treated with radiation therapy, insertion of a stent, or both. Level of evidence: fair; net benefit: moderate; grade of recommendation: B
REFERENCES
(1) Jacox A, Carr DB, Payne R, et al. Management of cancer pain: clinical practice guideline No. 9. Rockville, MD: Agency for Health Care Policy and Research, U.S. Department of Health and Human Services, Public Health Service, March 1994; AHCPR Publication No. 94-0592
(2) World Health Organization. Cancer pain relief and palliative care: Report of a WHO expert committee. World Health Organization Technical Report Series, 804. Geneva, Switzerland: World Health Organization, 1990; 1-75
(3) Hoegler D. Radiotherapy for palliation of symptoms in incurable cancer. Curr Probl Cancer 1997; 21:129-183
(4) Medical Research Council Lung Cancer Working Party. Inoperable non-small-cell lung cancer (NSCLC): a Medical Research Council randomized trial of palliative radiotherapy with two fractions or ten fractions. Br J Cancer 1991; 63:265-270
(5) Medical Research Council Lung Cancer Working Party. A Medical Research Council (MRC) randomised trial of palliative radiotherapy with two fractions or a single fraction in patients with inoperable non-small-cell lung cancer (NSCLC) and poor performance status. Br J Cancer 1992; 65:934-941
(6) Murai N, Koga K, Nagamachi S, et al. Radiotherapy in bone metastases, with special reference to its effect on relieving pain. Gan No Rinsho 1989; 35:1149-1152
(7) Hirano T, Baba H, Iwasaki K, et al. Curative local control of malignant tumors in the acetabulum by intraoperative radiotherapy. Arch Orthop Trauma Surg 1994; 113:215-217
(8) Salazar OM, Sandhu T, da Motta NW, et al. Fractionated half-body irradiation (HBI) for the rapid palliation of widespread, symptomatic, metastatic bone disease: a randomized Phase III trial of the International Atomic Energy Agency (IAEA). Int J Radiat Oncol Biol Phys 2001; 50:765-775
(9) Koswig S, Buchali A, Bohmer D, et al. Palliative radiotherapy of bone metastases: a retrospective analysis of 176 patients. Strahlenther Onkol 1999; 175:509-514
(10) Koswig S, Budach V. Remineralization and pain relief in bone metastases after different radiotherapy fractions (10 times 3 Gy vs 1 time 8 Gy): a prospective study. Strahlenther Onkol 1999; 175:500-508
(11) Hayashi S, Hoshi H, Iida T, et al. Multi-fractionated wide-field radiation therapy for palliation of multiple symptomatic bone metastases from solid tumors, Radiat Med 1999; 17:411-416
(12) Teshima T, Inouye T, Ikeda H, et al. Symptomatic relief for patients with osseous metastasis treated with radiation and methylprednisolone: a prospective randomized study. Radiat Med 1996; 14:185-188
(13) Deng H, Luo S, Tan T, et al. 153Sm-EDTMP for moderate and severe bone cancer pain. Hua Xi Yi Ke Da Xue Xue Bao Med Sci 1995; 26:391-394
(14) Jiang CY, Shu BL, Zhang YJ. The value of Sm-153-EDTMP for treatment of metastatic bone pain and improving quality of life. Zhonghua Zhong Liu Za Zhi 1994; 16:118-121
(15) Tian JH, Zhang JM, Hou QT, et al. Multicentre trial on the efficacy and toxicity of single-dose samarium-153-ethylene diamine tetramethylene phosphonate as a palliative treatment for painful skeletal metastases in China. Eur J Nucl Med 1999; 26:2-7
(16) Lee CK, Aeppli DM, Unger J, et al. Strontium-89 chloride (Metastron) for palliative treatment of bony metastases: the University of Minnesota experience. Am J Clin Oncol 1996; 19:102-107
(17) Firusian N. Endo-osseous isotope therapy of malignant skeletal disease. Cancer Res Clin Oncol 1978; 91:143-156
(18) Kucuk NO, Ibis E, Aras G, et al. Palliative analgesic effect of Re-186 HEDP in various cancer patients with bone metastases. Ann Nucl Med 2000; 14:239-245
(19) Shucai Z, Guimei L, Fanbin H. A clinical trial of Bonin in bone metastases of lung cancer. Chin J Clin Oncol 1999; 26:445-447
(20) Bloomfield DJ. Should bisphosphonates be part of the standard therapy of patients with multiple myeloma or bone metastases from other cancers? An evidence-based review. J Clin Oncol 1998; 16:1218-1225
(21) Egawa J, Kawada Y, Abe M, et al. Effect of porcine calcitonin on pain caused by cancer-induced bone destruction. Gan No Rinsho 1984; 30:251-258
(22) Schiraldi GF, Soresi E, Locicero S, et al. Salmon calcitonin in cancer pain: comparison between two different treatment schedules. Int J Clin Pharmacol Ther Toxicol 1987; 25:229-232
(23) Gangi A, Kastler B, Klinkert A, et al. Injection of alcohol into bone metastases under CT guidance. J Comput Assist Tomogr 1994; 18:932-935
(24) Gorich J, Solymosi L, Hasan I, et al. Embolization of bone metastases. Radiologe 1995; 35:55-59
(25) Haentjens P, Casteleyn PP, Opdecam P. Evaluation of impending fractures and indications for prophylactic fixation of metastases in long bones: review of the literature. Acta Orthop Belg 1993; 59(Suppl 1):6-11
(26) Broos P, Reynders P, van den Bogert W, et al. Surgical treatment of metastatic fracture of the femur improvement of quality of life. Acta Orthop Belg 1993; 59(Suppl 1):52-56
(27) Damron TA, Rock MG, Choudhury SN, et al. Biomechanical analysis of prophylactic fixation for middle third humeral impending pathologic fractures. Clin Orthop 1999; 363: 240-248
(28) Fourneau I, Broos P. Pathologic fractures due to metastatic disease: a retrospective study of 160 surgically treated fractures. Acta Chir Belg 1998; 98:255-260
(29) Turner S, Marosszeky B, Timms I, et al. Malignant spinal cord compression: prospective evaluation. Int J Radiat Oncol Biol Phys 1993:26:141-146
(30) Sorenson S, Helweg-Larsen S, et al. Effect of high-dose dexamethasone in carcinomatous metastatic spinal cord compression treated with radiotherapy: a randomised trial. Eur J Cancer 1994; 30A:22-27
(31) Loblaw DA, Laperriere NJ. Emergency treatment of malignant extradural spinal cord compression: an evidence-based guideline. J Clin Oncol 1998; 16:1613-1624
(32) Jenis LG, Dunn EJ, An HS. Metastatic disease of the cervical spine: a review. Clin Orthop 1999; 359:89-103
(33) Ghogawala Z, Mansfield FL, Borges LF. Spinal radiation before surgical compression adversely affects outcomes of surgery for symptomatic metastatic spinal cord compression. Spine 2001; 26:818-824
(34) Chataigner H, Onimus M. Surgery in spinal metastasis without spinal cord compression: indications and strategy related to the risk of recurrence. Eur Spine J 2000; 9:523-527
(35) Sundaresan N, Galicich JH, Bains MS, et al. Vertebral body resection in the treatment of cancer involving the spine. Cancer 1984; 53:1393-1396
(36) Newman SJ, Hansen HH. Proceedings: frequency, diagnosis and treatment of brain metastases in 247 consecutive patients with bronchogenic carcinoma. Cancer 1974; 33:492-496
(37) Hirsch FR, Paulson OB, Hansen HH, et al. Intracranial metastases in small cell carcinoma of the lung: prognostic aspects. Cancer 1983; 51:529-533
(38) Andrews RJ, Gluck DS, Konchingeri RH. Surgical resection of brain metastases from lung cancer. Acta Neurochir (Wien) 1996; 138:382-389
(39) Kelly K, Bunn PA Jr. Is it time to reevaluate our approach to the treatment of brain metastases in patients with non-small cell lung cancer? Lung Cancer 1998; 20:85-91
(40) Cairncross JG, Kim JH, Posner J. Radiation therapy for brain metastases. Ann Neurol 1980; 7:529-541
(41) Coia LR, Aaronson N, Linggood R, et al. A report of the consensus workshop panel on the treatment of brain metastases. Int J Radiat Oncol Biol Phys 1992; 23:223-227
(42) Shapiro WR. Intracranial neoplasms. In: Rosenberg RN, ed. Comprehensive neurology. New York, NY: Raven Press, 1991; 157-200
(43) Weiss HD. Neoplasms. In: Samuel MA, ed. Manual of neurology. 4th ed. Boston, MA: Little, Brown, 1991; 213-239
(44) French LA, Galicich JH. The use of steroids for control of cerebral edema. Clin Neurosurg 1964; 10:212-223
(45) Weissman DE, Dufer D, Vogel V, et al. Corticosteroid toxicity in neuro-oncology patients. J Neurooncol 1987; 5:125-128
(46) Vecht CJ, Hovestadt A, Verbiest HBC, et al. Dose-effect relationship of dexamethasone on Karnofsky performance in metastatic brain tumors: a randomized study of doses of 4, 8, and 16 mg per day. Neurology 1994; 44:675-680
(47) Weissman DE, Janjan NA, Erickson B, et al. Twice-daily tapering dexamethasone treatment during cranial radiation for newly diagnosed brain metastases. J Neurooncol 1991; 11:235-239
(48) Wolfson AH, Snodgrass SM, Schwade JG, et al. The role of steroids in the management of metastatic carcinoma to the brain: a pilot prospective trial. Am J Clin Oncol 1994; 17:234-238
(49) Diener-West M, Dobbins TW, et al. Identification of an optimal subgroup for treatment evaluation of patients with brain metastases using RTOG study 7916. Int J Radiat Oncol Biol Phys 1989; 16:669-673
(50) Rock JP, Haines S, Recht L, et al. Practice parameters for the management of single brain metastasis. Neurosurg Focus 2000; 9:1-9
(51) Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 1990; 322:494-500
(52) Vecht CJ, Haaxma-Reiche H, Noordijk EM, et al. Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery? Ann Neurol 1993; 33:583-590
(53) Mintz AH, Kestle J, Rathbone MP, et al. A randomized trial to assess the efficacy of surgery in addition to radiotherapy in patients with single brain metastasis. Cancer 1996; 78:1470-1476
(54) Patchell RA, Tibbs PA, Regine WF, et al. Postoperative radiotherapy in the treatment of single metastases to the brain: randomized trial. JAMA 1998; 280:1485-1489
(55) Borgelt B, Gelber RD, Kramer S, et al. The palliation of brain metastases: final results of the first two studies by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys 1980; 6:1-9
(56) Kurtz J, Gelber R, Brady LW, et al. The palliation of brain metastases in a favorable patient population: a randomized clinical trial by the Radiation Therapy Ontology Group. Int J Radiat Oncol Biol Phys 1981; 7:891-895
(57) Zouhair A, Tercier PA, Fankhauser H, et al. Stereotactic radiotherapy of brain metastases: experience in Lausanne. Schweiz Med Wochenschr 1997; 40:1652-1656
(58) Shirato H, Takmura A, Tomita M, et al. Stereotactic irradiation without whole-brain irradiation for single brain metastasis. Int J Radiat Oncol Biol Phys 1997; 37:385-391
(59) Flickinger JC, Kondziolka D, Lunsford LD, et al. A multi-institutional experience with stereotactic radiosurgery for solitary brain metastasis. Int J Radiat Oncol Biol Phys 1994; 28:797-802
(60) Adler Jr, Cox RS, Kaplan I, et al. Stereotactic radiosurgical treatment of brain metastases. J Neurosurg 1992; 76:444-449
(61) Alexander E 3rd, Moriarty TM, Davis RB, et al. Stereotactic radiosurgery for the definitive, noninvasive treatment of brain metastases. J Natl Cancer Inst 1995; 8734-8740
(62) Muacevic A, Kreth FW, Horstmann GA, et al. Surgery and radiotherapy compared with gamma knife radiosurgery in the treatment of solitary cerebral metastases of small diameter. J Neurosurg 1999; 91:35-43
(63) Li B, Yu J, Suntharalingam M, et al. Comparison of three treatment options for single brain metastasis from lung cancer. Int J Cancer 2000; 90:37-45
(64) Kondziolka D, Patel A, Lunsford LD, et al. Stereotactic radiosurgery plus whole brain radiotherapy vs radiotherapy alone for patients with multiple, brain metastases. Int J Radiat Oncol Biol Phys 1999; 45:427-434
(65) Hoffman R, Sneed PK, McDermott MW, et al. Radiosurgery for brain metastases from primary lung carcinoma. Cancer J 2001; 7:121-131
(66) Muers MF, Round CE. Palliation of symptoms in non-small cell lung cancer: a study by the Yorkshire Regional Cancer Organisation Thoracic Group. Thorax 1993; 48:339-343
(67) Reuben DB, Mor V. Dyspnea in terminally ill cancer patients. Chest 1986; 89:234-236
(68) Escalante CP, Martin CG, Elting LS, et al. Dyspnea in cancer patients. Etiology, resource utilization, and survival-implications in a managed care world. Cancer 1996; 78: 1314-1319
(69) Claessens MT, Lynn J, Zhong Z, et al. Dying with lung cancer or chronic obstructive pulmonary disease: insights from SUPPORT. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc 2000; 48(5Suppl):S146-S153
(70) Smith EL, Hann DM, Ahles TA, et al. Dyspnea, anxiety, body consciousness, and quality of life in patients with lung cancer. J Pain Symptom Manage 2001; 21:323-329
(71) Dudgeon DJ, Lertzman M. Dyspnea in the advanced cancer patient. J Pain Symptom Manage 1998; 16:212-219
(72) O'Driscoll M, Corner J, Bailey C. The experience of breathlessness in lung cancer. Eur J Cancer Care (Engl) 1999; 8:37-43
(73) Bernhard J, Ganz PA. Psychosocial issues in lung cancer patients: part 1. Chest 1991; 99:216-223
(74) Kellner R, Samet J, Pathak D. Dyspnea, anxiety, and depression in chronic respiratory impairment. Gen Hosp Psychiatry 1992; 14:20-28
(75) Gift AG, Cahill CA. Psychophysiologic aspects of dyspnea in chronic obstructive pulmonary disease: a pilot study. Heart Lung 1990; 19:252-257
(76) Stone P, Richards M, A'Hern R, et al. A study to investigate the prevalence, severity and correlates of fatigue among patients with cancer in comparison with a control group of volunteers without cancer. Ann Oncol 2000; 11:561-567
(77) Abratt RP, Willcox PA. The effect of irradiation on lung function and perfusion in patients with lung cancer. Int J Radiat Oncol Biol Phys 1995; 31:915-919
(78) Bruera E, de Stoutz N, Velasco-Leiva A, et al. Effects of oxygen on dyspnoea in hypoxaemic terminal-cancer patients. Lancet 1993; 342:13-14
(79) Boyd KJ, Kelly M. Oral morphine as symptomatic treatment of dyspnoea in patients with advanced cancer. Palliat Med 1997; 11:277-281
(80) Zeppetella G. Nebulized morphine in the palliation of dyspnoea. Palliat Med 1997; 11:267-275
(81) Cohen MH, Anderson AJ, Krasnow SH, et al. Continuous intravenous infusion of morphine for severe dyspnea. South Med J 1991; 84:229-234
(82) Lang E, Jedeikin R. Acute respiratory depression as a complication of nebulized morphine. Can J Anaesth 1998; 45:60-62
(83) Bredin M, Corner J, Krishnasamy M, et al. Multicentre randomised controlled trial of nursing intervention for breathlessness in patients with lung cancer. BMJ 1999; 318:901-904
(84) Corner J, Plant H, A'Hern R, et al. Non-pharmacological intervention for breathlessness in lung cancer. Palliat Med 1996; 10:299-305
(85) Vaaler AK, Forrester JM, Lesar M, et al. Obstructive atelectasis in patients with small cell lung cancer: incidence and response to treatment. Chest 1997; 111:115-120
(86) Doona M, Walsh D. Benzonatate for opioid-resistant cough in advanced cancer. Palliat Med 1998; 12:55-58
(87) Moroni M, Porta C, Gualtieri G, et al. Inhaled sodium cromoglycate to treat cough in advanced lung cancer patients. Br J Cancer 1996; 74:309-311
(88) Luporini G, Barni S, Marchi E, et al. Efficacy and safety of levodropropizine and dihydrocodeine on nonproductive cough in primary and metastatic lung cancer. Eur Respir J 1998; 12:97-101
(89) Cohen S, Hossain SA. Primary carcinoma of the lung: a review of 417 histologically proved cases. Dis Chest 1966; 49:67-74
(90) Emerson GL, Emerson MS, Sherwood CE. The natural history of carcinoma of the lung. J Thorac Surg 1959; 37:291-304
(91) Johnston WW. The malignant pleural effusion: a review of cytopathologic diagnoses of 584 specimens from 472 consecutive patients. Cancer 1985; 56:905-909
(92) Chernow B, Sahn SA. Carcinomatous involvement of the pleura: an analysis of 96 patients. Am J Med 1977; 63:695-702
(93) Estenne M, Yernault JC, De Troyer A. Mechanism of relief of dyspnea after thoracocentesis in patients with large pleural effusions. Am J Med 1983; 74:813-819
(94) Light RW, Stansbury DW, Brown SE. The relationship between pleural pressures and changes in pulmonary function after therapeutic thoracentesis. Am Rev Respir Dis 1986; 133:658-661
(95) Agusti AG, Cardus J, Roca J, et al. Ventilation-perfusion mismatch in patients with pleural effusion: effects of thoracentesis. Am J Respir Crit Care Med 1997; 156:1205-1209
(96) Karetzky MS, Kothari GA, Fourre JA, et al. Effect of thoracentesis on arterial oxygen tension. Respiration 1978; 36:96-103
(97) Brown NE, Zamel N, Aberman A. Changes in pulmonary mechanics and gas exchange following thoracocentesis. Chest 1978; 74:540-542
(98) Krell WS, Rodarte JR. Effects of acute pleural effusion on respiratory system mechanics in dogs. J Appl Physiol 1985; 59:1458-1463
(99) Management of malignant pleural effusions. Am J Respir Crit Care Med 2000; 162:1987-2001
(100) Light RW, Jenkinson SG, Minh VD, et al. Observations on pleural fluid pressures as fluid is withdrawn during thoracentesis. Am Rev Respir Dis 1980; 121:799-804
(101) Lan RS, Lo SK, Chuang ML, et al. Elastance of the pleural space: a predictor for the outcome of pleurodesis in patients with malignant pleural effusion. Ann Intern Med 1997; 126:768-774
(102) Walker-Renard PB, Vaughan LM, Sahn SA. Chemical pleurodesis for malignant pleural effusions. Ann Intern Med 1994; 120:56-64
(103) Hartman DL, Gaither JM, Kesler KA, et al. Comparison of insufflated talc under thoracoscopic guidance with standard tetracycline and bleomycin pleurodesis for control of malignant pleural effusions. Thorac Cardiovasc Surg 1993; 105: 743-747
(104) Hamed H, Fentiman IS, Chaudary MA, et al. Comparison of intracavitary bleomycin and talc for control of pleural effusions secondary to carcinoma of the breast. Br J Surg 1989; 76:1266-1267
(105) Fentiman IS, Rubens RD, Hayward JL. A comparison of intracavitary talc and tetracycline for the control of pleural effusions secondary to breast cancer. Eur J Cancer Clin Oncol 1986; 22:1079-1081
(106) Todd TR, Delarue NC, Ilves R, et al. Talc poudrage for malignant pleural effusion. Chest 1980; 78:542
(107) Fentiman IS, Rubens RD, Hayward JL. Control of pleural effusions in patients with breast cancer: a randomized trial. Cancer 1983; 52:737-739
(108) Yim AP, Chan AT, Lee TW, et al. Thoracoscopic talc insufflation vs talc slurry for symptomatic malignant pleural effusion. Ann Thorac Surg 1996; 62:1655
(109) Kennedy L, Rusch VW, Strange C, et al. Pleurodesis using talc slurry. Chest 1994; 106:342-346
(110) Patz EF Jr, McAdams HP, Erasmus JJ, et al. Sclerotherapy for malignant pleural effusions: a prospective randomized trial of bleomycin vs doxycycline with small-bore catheter drainage. Chest 1998; 113:1305-1311
(111) Heffner JE, Standerfer RJ, Torstveit J, et al. Clinical efficacy of doxycycline for pleurodesis. Chest 1994; 105:1743-1747
(112) Pulsiripunya C, Youngchaiyud P, Pushpakom R, et al. The efficacy of doxycycline as a pleural sclerosing agent in malignant pleural effusion: a prospective study. Respirology 1996; 1:69-72
(113) Moffett MJ, Ruckdeschel JC. Bleomycin and tetracycline in malignant pleural effusions: a review. Semin Oncol 1992; 19(2Suppl5):59-62
(114) Martinez-Moragon E, Aparicio J, Rogado MC, et al. Pleurodesis in malignant pleural effusions: a randomized study of tetracycline vs bleomycin. Eur Respir J 1997; 10:2380-2383
(115) Zimmer PW, Hill M, Casey K, et al. Prospective randomized trial of talc slurry vs bleomycin in pleurodesis for symptomatic malignant pleural effusions. Chest 1997; 112:430-434
(116) Macaulay VM, O'Byrne KJ, Saunders MP, et al. Phase I study of intrapleural batimastat (BB-94), a matrix metalloproteinase inhibitor, in the treatment of malignant pleural effusions. Clin Cancer Res 1999; 5:513-520
(117) Kelly-Garcia J, Roman-Berumen JF, Ibarra-Perez C. Iodopovidone and bleomycin pleurodesis for effusions due to malignant epithelial neoplasms. Arch Med Res 1997; 28: 583-585
(118) Bjermer L, Gruber A, Sue-Chu M, et al. Effects of intrapleural mitoxantrone and mepacrine on malignant pleural effusion: a randomized study. Eur J Cancer 1995; 31A:2203-2208
(119) Luh KT, Yang PC, Kuo SH, et al. Comparison of OK-432 and mitomycin C pleurodesis for malignant pleural effusion caused by lung cancer: a randomized trial. Cancer 1992; 69:674-679
(120) Figlin R, Mendoza E, Piantadosi S, et al. Intrapleural chemotherapy without pleurodesis for malignant pleural effusions: LCSG Trial 861. Chest 1994; 106(6Suppl):363S-366S
(121) Masuno T, Kishimoto S, Ogura T, et al. A comparative trial of LC9018 plus doxorubicin and doxorubicin alone for the treatment of malignant pleural effusion secondary to lung cancer. Cancer 1991; 68:1495-1500
(122) Ike O, Shimizu V, Hitomi S, et al. Treatment of malignant pleural effusions with doxorubicin hydrochloride-containing poly(L-lactic acid) microspheres. Chest 1991; 99:911-915
(123) Rosso R, Rimoldi R, Salvati F, et al. Intrapleural natural beta interferon in the treatment of malignant pleural effusions. Oncology 1988; 45:253-256
(124) Astoul P, Viallat JR, Laurent JC, et al. Intrapleural recombinant IL-2 in passive immunotherapy for malignant pleural effusion. Chest 1993; 103:209-213
(125) Viallat JR, Boutin C, Rey F, et al. Intrapleural immunotherapy with escalating doses of interleukin-2 in metastatic pleural effusions. Cancer 1993; 71:4067-4076
(126) Ponn RB, Blancaflor J, D'Agostino RS, et al. Pleuroperitoneal shunting for intractable pleural effusions. Ann Thorac Surg 1991; 51:605-609
(127) Pope AR, Joseph JH. Pleuroperitoneal shunt for pneumonectomy cavity malignant effusion. Chest 1989; 96:686-688
(128) Schulze M, Boehle AS, Kurdow R, et al. Effective treatment of malignant pleural effusion by minimal invasive thoracic surgery: thoracoscopic talc pleurodesis and pleuroperitoneal shunts in 101 patients. Ann Thorac Surg 2001; 71:1809-1812
(129) Reich H, Beattie EJ, Harvey JC. Pleuroperitoneal shunt for malignant pleural effusions: a one-year experience. Semin Surg Oncol 1993; 9:160-162
(130) Petrou M, Kaplan D, Goldstraw P. Management of recurrent malignant pleural effusions: the complementary role of talc pleurodesis and pleuroperitoneal shunting. Cancer 1995; 75:801-805
(131) Chen YM, Shih JF, Yang KY, et al. Usefulness of pig-tail catheter for palliative drainage of malignant pleural effusions in cancer patients. Support Care Cancer 2000; 8:423-426
(132) Pien GW, Gant MJ, Washam CL, et al. Use of an implantable pleural catheter for trapped lung syndrome in patients with malignant pleural effusion. Chest 2001; 119:1641-1646
(133) Pollak JS, Burdge CM, Rosenblatt M, et al. Treatment of malignant pleural effusion with tunneled long-term drainage catheters. J Vase Interv Radiol 2001; 12:201-208
(134) Livingston RB, McCracken JD, Trauth CJ, et al. Isolated pleural effusion in small cell lung carcinoma: favorable prognosis. Chest 1982; 81:208-211
(135) Ramser ER, Beamis JF Jr. Laser bronchoscopy, Clin Chest Med 1995; 16:415-426
(136) Colt HG, Harrell JH. Therapeutic rigid bronchoscopy allows level of care changes in patients with acute respiratory failure from central airways obstruction. Chest 1997; 112: 202-206
(137) Miyazawa T, Yamakido M, Ikeda S, et al. Implantation of ultraflex nitinol stents in malignant tracheobronchial stenoses. Chest 2000; 118:959-965
(138) Hautmann H, Gamarra F, Pfeifer KJ, et al. Fiberoptic bronchoscopic balloon dilatation in malignant tracheobronchial disease: indications and results. Chest 2001; 120:43-49
(139) Ball JB, Delaney JC, Evans CC, et al. Endoscopic bougie and balloon dilatation of multiple bronchial stenoses: 10 year follow up. Thorax 1991; 46:933-935
(140) Cavaliere S, Foccoli P, Toninelli C, et al. Nd-YAG laser therapy in lung cancer: an 11-year experience with 2,253 applications in 1,585 patients. J Bronchol 1994; 1:105-111
(141) Cavaliere S, Venuta F, Foccoli P, et al. Endoscopic treatment of malignant airway obstructions in 2,008 patients. Chest 1996; 110:1536-1542
(142) Sheski FD, Mathur PN. Cryotherapy, electrocautery, and brachytherapy. Clin Chest Med 1999; 20:123-138
(143) Homasson JP, Bell NJ. Endobronchial electrocautery. Semin Respir Crit Care Med 1997; 18:535-543
(144) Petrou M, Kaplan D, Goldstraw P. Bronchoscopic diathermy resection and stent insertion: a cost effective treatment for tracheobronchial obstruction. Thorax 1993; 48: 1156-1159
(145) Sutedja G, van Kralingen K, Schramel FM, et al. Fibreoptic bronchoscopic electrosurgery under local anaesthesia for rapid palliation in patients with central airway malignancies.: a preliminary report. Thorax 1994; 49:1243-1246
(146) van Boxem TJ, Venmans BJ, van Mourik JC, et al. Bronchoscopic treatment of intraluminal typical carcinoid: a pilot study. Thorac Cardiovasc Surg 1998; 116:402-406
(147) van Boxem TJ, Venmans BJ, Schramel FM, et al. Radiographically occult lung cancer treated with fibreoptic bronchoscopic electrocautery: a pilot study of a simple and inexpensive technique. Eur Respir J 1998; 11:169-172
(148) Coulter TD, Mehta AC. The heat is on: impact of endobronchial electrosurgery on the need for Nd:YAG laser photoresection. Chest 2000; 118:516-521
(149) Morice RC, Ece T, Ece F, et al. Endobronchial argon plasma coagulation for treatment of hemoptysis and neoplastic airway obstruction. Chest 2001; 119:781-787
(150) Mathur PN, Wolf KM, Busk MF, et al. Fiberoptic bronchoscopic cryotherapy in the management of tracheobronchial obstruction. Chest 1996; 110:718-723
(151) Marasso A, Gallo E, Massaglia GM, et al. Cryosurgery in bronchoscopic treatment of tracheobronchial stenosis: indications, limits, personal experience. Chest 1993; 103:472-474
(152) Rodgers BM, Moazam F, Talbert JL. Endotracheal cryotherapy in the treatment of refractory airway strictures. Ann Thorac Surg 1983; 35:52-57
(153) Maiwand MO, Homasson JP. Cryotherapy for tracheobronchial disorders. Clin Chest Med 1995; 16:427-443
(154) Walsh DA, Maiwand MO, Nath AR, et al. Bronchoscopic cryotherapy for advanced bronchial carcinoma. Thorax 1990; 45:509-513
(155) Bolliger CT, Heitz M, Hauser R, et al. An airway Wallstent for the treatment of tracheobronchial malignancies. Thorax 1996; 51:1127-1129
(156) Monnier P, Mudry A, Stanzel F, et al. The use of the covered Wallstent for the palliative treatment of inoperable tracheobronchial cancers: a prospective, multicenter study. Chest 1996; 110:1161-1168
(157) Witt C, Dinges S, Schmidt B, et al. Temporary tracheobronchial stenting in malignant stenoses. Eur J Cancer 1997; 33:204-208
(158) Dumon JF. A dedicated tracheobronchial stent. Chest 1990; 97:328-332
(159) Homasson JP, Renault P, Angebault M, et al. Bronchoscopic cryotherapy for airway strictures caused by tumors. Chest 1986; 90:159-164
(160) Dumon JF, Cavaliere S, Diaz-Jimenez P, et al. Seven-year experience with the Dumon prosthesis. J Bronchol 1996; 3:6-10
(161) Schray MF, McDougall JC, Martinez A, et al. Management of malignant airway compromise with laser and low dose rate brachytherapy: The Mayo Clinic experience. Chest 1988; 93:264-269
(162) Villanueva AG, Lo TC, Beamis JF Jr. Endobronchial brachytherapy. Clin Chest Med 1995; 16:445-454
(163) Ofiara L, Roman T, Schwartzman K, et al. Local determinants of response to endobronchial high-dose rate brachytherapy in bronchogenic carcinoma. Chest 1997; 112:946-953
(164) Bedwinek J, Petty A, Bruton C, et al. The use of high dose rate endobronchial brachytherapy to palliate symptomatic endobronchial recurrence of previously irradiated bronchogenic carcinoma. Int J Radiat Oncol Biol Phys 1992; 22: 23-30
(165) Gauwitz M, Ellerbroek N, Komaki R, et al. High dose endobronchial irradiation in recurrent bronchogenic carcinoma. Int J Radiat Oncol Biol Phys 1992; 23:397-400
(166) Hernandez P, Gursahaney A Roman T, et al. High dose rate brachytherapy for the local control of endobronchial carcinoma following external irradiation. Thorax 1996; 51:354-358
(167) Micke O, Prott FJ, Schafer U, et al. Endoluminal HDR-brachytherapy as a palliative treatment of patients with the recurrence of a non-small cell bronchial carcinoma after prior radiotherapy. Strahlenther Onkol 1995; 171: 554-559
(168) Nori D, Allison R, Kaplan B, et al. High dose-rate intraluminal irradiation in bronchogenic carcinoma: technique and results. Chest 1993; 104:1006-1011
(169) Pisch J, Villamena PC, Harvey JC, et al. High dose-rate endobronchial irradiation in malignant airway obstruction. Chest 1993; 104:721-725
(170) Seagren SL, Harrell JH, Horn RA. High dose rate intraluminal irradiation in recurrent endobronchial carcinoma. Chest 1985; 88:810-814
(171) Sutedja G, Baris G, Schaake-Koning C, et al. High dose rate brachytherapy in patients with local recurrences after radiotherapy of non-small cell lung cancer. Int J Radiat Oncol Biol Phys 1992; 24:551-553
(172) Langendijk H, de Jong J, Tjwa M, et al. External irradiation vs external irradiation plus endobronchial brachytherapy in inoperable non-small cell lung cancer: a prospective randomized study. Radiother Oncol 2001; 58:257-268
(173) Burt PA, O'Driscoll BR, Notley HM, et al. Intraluminal irradiation for the palliation of lung cancer with high dose rate micro-Selectron. Thorax 1990; 45:765-768
(174) Chang LF, Horvath J, Peyton w, et al. High dose rate afterloading intraluminal brachytherapy in malignant airway obstruction of lung cancer. Int J Radiat Oncol Biol Phys 1994; 28:589-596
(175) Gollins SW, Burt PA, Barber PV, et al. High dose rate intraluminal radiotherapy for carcinoma of the bronchus: outcome of treatment of 406 patients. Radiother Oncol 1994; 33:31-40
(176) Huber RM, Fischer R, Hautmann H. Palliative endobronchial brachytherapy for central lung tumors: a prospective, randomized comparison of two fractionation schedules. Chest 1995; 107:463-470
(177) Mehta MP, Shahabi S, Jarjour NN, et al. Endobronchial irradiation for malignant airway obstruction. Int J Radiat Oncol Biol Phys 1989; 17:847-851
(178) Speiser BL, Spratling L. Remote afterloading brachytherapy for the local control of endobronchial carcinoma. Int J Radiat Oncol Biol Phys 193; 25:579-587
(179) Anacak Y, Mogulkoc N, Ozkok S, et al. High dose rate endobronchial brachytherapy in combination with external beam radiotherapy for stage III non-small cell lung cancer. Lung Cancer 2001; 34:253-259
(180) Langendijk JA, Tjwa MK, de Jong JM, et al. Massive haemoptysis after radiotherapy in inoperable non-small cell lung carcinoma: is endobronchial brachytherapy really a risk factor? Radiother Oncol 1998; 49:175-183
(181) Edell ES, Cortese DA. Bronchoscopic phototherapy with hematoporphyrin derivative for treatment of localized bronchogenic carcinoma: a 5-year experience. Mayo Clin Proc 1987; 62:8-14
(182) Cortese DA, Edell ES, Kinsey JH. Photodynamic therapy for early stage squamous cell carcinoma of the lung. Mayo Clin Proc 1997; 72:595-602
(183) Moghissi K, Dixon K, Stringer M, et al. The place of bronchoscopic photodynamic therapy in advanced unresectable lung cancer: experience of 100 cases. Eur J Cardiothorac Surg 1999; 15:1-6
(184) Miller RR, McGregor DH. Hemorrhage from carcinoma of the lung. Cancer 1980; 46:200-205
(185) Chute CG, Greenberg ER, Baron J, et al. Presenting conditions of 1539 population-based lung cancer patients by cell type and stage in New Hampshire and Vermont. Cancer 1985; 56:2107-2111
(186) Hyde L, Hyde CI. Clinical manifestations of lung cancer. Chest 1974; 65:299-306
(187) Grippi MA. Clinical aspects of lung cancer. Semin Roentgenol 1990; 25:12-24
(188) Corey R, Hla KM. Major and massive hemoptysis: reassessment of conservative management. Am J Med Sci 1987; 294:301-309
(189) Cahill BC, Ingbar DH. Massive hemoptysis: assessment and management. Clin Chest Med 1994; 15:147-167
(190) Jean-Baptiste E. Clinical assessment and management of massive hemoptysis. Crit Care Med 2000; 28:1642-1647
(191) Strange C. Double-lumen endotracheal tubes. Clin Chest Med 1991; 12:497-506
(192) Zavala DC. Pulmonary hemorrhage in fiberoptic transbronchial biopsy. Chest 1976; 70:584-588
(193) Worth H, Breuer HWM, Charchut S, et al. Endobronchial vs intravenous application of glypressin for the therapy and prevention of lung bleeding during bronchoscopy. Am Rev Respir Dis 1987; 135(4 part 2):A108
(194) Sahebjami H. Iced saline lavage during bronchoscopy. Chest 1976; 69:131-13
(195) Conlan AA, Hurwitz SS. Management of massive haemoptysis with the rigid bronchoscope and cold saline lavage. Thorax 1980; 35:901-90
(196) Hiebert CA. Balloon catheter control of life-threatening hemoptysis. Chest 1974; 66:308-30
(197) Gottlieb LS, Hillberg R. Endobronchial tamponade therapy for intractable hemoptysis. Chest 1975; 67:482-483
(198) Saw EC, Gottlieb LS, Yokahama T, et al. Flexible fiberoptic bronchoscopy and endobronchial tamponade in the management of hemoptysis. Chest 1976; 70:589-51
(199) Swersky RB, Chang JB, Wisoff BG, et al. Endobronchial balloon tamponade of hemoptysis in patients with cystic fibrosis. Ann Thorac Surg 1979; 27:262-264
(200) Hetzel MR, Smith SG. Endoscopic palliation of tracheobronchial malignancies. Thorax 1991; 46:325-333
(201) Jain PR, Dedhia HV, Lapp NL, et al. Nd-YAG laser followed by radiation for treatment of malignant airway lesions. Lasers Surg Med 1985; 5:47-53
(202) Mal H, Rullon I, Mellot F, et al. Immediate and long-term results of bronchial artery embolization for life-threatening hemoptysis. Chest 1999; 115:996-1001
(203) White RI Jr. Bronchial artery embolotherapy for control of acute hemoptysis: analysis of outcome. Chest 1999; 115: 912-915
(204) Osaki S, Nakanishi Y, Wataya H, et al. Prognosis of bronchial artery embolization in the management of hemoptysis. Respiration 2000; 67:412-416
(205) Knott-Craig CJ, Oostuizen JG, Rossouw G, et al. Management and prognosis of massive hemoptysis: recent experience with 120 patients. Thorac Cardiovasc Surg 1993; 105:394-397
(206) Hoegler D. Radiotherapy for palliation of symptoms in incurable cancer. Curr Probl Cancer 1997; 21:129-183
(207) Freitag L, Tekolf E, Steveling H, et al. Management of malignant esophago-tracheal fistulas with airway stenting and double stenting. Chest 1996; 110:1155-1160
(208) Colt HG, Meric B, Dumon JF. Double stents for carcinoma of the esophagus invading the tracheo-bronchial tree. Gastrointest Endosc 1992; 38:485-489
(209) Alexiou C, Neuhaus H, Kan RJ, et al. Treatment of esophagorespiratory fistula by insertion of an esophageal Montgomery and tracheal dynamic stent after failure of conventional endoprosthesis. ORL J Otorhinolaryngol Relat Spec 1998; 60:51-54
(210) Baker GL, Barnes HJ. Superior vena cava syndrome: etiology, diagnosis, and treatment. Am J Crit Care 1992; 1:54-64
(211) Muers MF. Lung cancer: quality of life and symptom control. Eur Respir J 2001; 6:305-329
(212) Wurschmidt F, Bunemann H, Heilmann HP. Small cell lung cancer with and without superior vena cava syndrome: a multivariate analysis of prognostic factors in 408 cases. Int J Radiat Oncol Biol Phys 1995; 33:77-82
(213) Kawanami S, Imada H, Terashima H, et al. Radiotherapy of superior vena cava syndrome. Jpn J Lung Cancer 1996; 36:745-752
(214) Sasano S, Onuki T, Mae M, et al. Wallstent endovascular prosthesis for the treatment of superior vena cava syndrome. Jpn Thorac Cardiovasc Surg 2001; 49:165-170
(215) Tanigawa N, Sawada S, Mishima K, et al. Clinical outcome of stenting in superior vena cava syndrome associated with malignant tumors: comparison with conventional treatment. Acta Radiol 1998; 39:669-674
(216) Nicholson AA, Ettles DF, Arnold A, et al. Treatment of malignant superior vena cava obstruction: metal stents or radiation therapy. J Vasc Interv Radiol 1997; 8:781-788
* From the Division of Pulmonary, Critical Care, Allergy, Immunology, and Sleep Disorders Medicine (Drs. Kvale and Simoff), Henry Ford Health System, Detroit, MI; and Division of Thoracic Medicine (Dr. Prakash), Mayo Clinic, Rochester, MN.
Correspondence to: Paul A. Kvale, MD, FCCP, Division of Pulmonary, Critical Care, Allergy, Immunology, and Sleep Disorders Medicine, Henry Ford Health System, 2799 West Grand Blvd, Detroit, MI 48202; e-mail: pkvale1@hfhs.org
COPYRIGHT 2003 American College of Chest Physicians
COPYRIGHT 2003 Gale Group