Paclitaxel is one of the most extensively used anticancer agents, however, its use is often limited by severe hypersensitivity reactions, including respiratory distress, bronchospasm, and hypotension, which can occur despite premedication with dexamethasone and histamine H^sub 1^ and H^sub 2^ antagonists. The present study was designed to determine the mechanisms of paclitaxel hypersensitivity. In rats, paclitaxel (15 mg/kg, intravenously) caused a marked increase in pulmonary vascular permeability and edema. Pa^sub o^sub 2^^ decreased, whereas Pa^sub co^^sub 2^ increased, transiently after paclitaxel injection. The paclitaxel-induced pulmonary vascular hyperpermeability was blocked by dexamethasone but not by histamine H^sub 1^ or H^sub 2^ antagonists. Paclitaxel increased the vascular permeability in lungs of mast cell-deficient rats Ws/Ws^sup -/-^ to almost the similar extent as that elicited in wild-type rats. On the other hand, the paclitaxel-induced pulmonary vascular hyperpermeability was reversed by sensory denervation with capsaicin or pretreatment with LY303870 and SR48968, NK^sub 1^ and NK^sub 2^ antagonists, respectively. Consistent with these findings, a marked elevation of sensory neuropeptides such as substance P, neurokinin A, and calcitonin gene-related peptide was observed in rat bronchoalveolar lavage fluid after paclitaxel injection. These findings suggest that sensory nerves rather than mast cells are implicated in the etiology of paclitaxel hypersensitivity.
Keywords: paclitaxel; hypersensitivity; sensory nerve
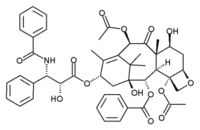
Paclitaxel is a unique anticancer agent with tubulin-stabilizing action and widely used for several malignancies, including those of ovary, breast, non-small lung cells, and stomach. However, its use is often limited because of the occurrence of severe adverse events. Hypersensitivity reactions (HSR) characterized by erythematous rashes, respiratory distress, bronchospasm, hypotension, and pulmonary edema are some major side effects that limit the use of chemotherapy (1-4). Although little is known about the etiology of paclitaxel hypersensitivity, the nonionic surfactant Cremophor EL (polyoxyethylated castor oil) included in paclitaxel injection is considered to be one of causes of the HSR (5, 6) because the surfactant has been shown to initiate histamine release from mast cells (7, 8). Moreover, the characteristics of paclitaxel hypersensitivity such as the rapid onset and its symptoms are similar to type I allergic anaphylactic reactions involving mast cell degranulation. Consequently, the combined medication of histamine H^sub 1^ and H^sub 2^ antagonists with glucocorticoids is inevitably performed before paclitaxel chemotherapy to prevent HSR (9-13). Nevertheless, patients are occasionally obliged to discontinue the paclitaxel chemotherapy due to the occurrence of the HSR (14-17). The inability of the conventional premedication to completely block the paclitaxel HSR raises the possibility that other mediators than mast cell histamine is implicated in the HSR.
Unfortunately, hitherto neither have there been direct evidences for an involvement of mast cell histamine in paclitaxel HSR nor have there been any studies on the cellular mechanisms of paclitaxel HSR. This may partly be due to the lack of animal models of HSR to paclitaxel. We found in the present study that a marked extravasation of plasma proteins and edema were elicited in lungs of rats with a concomitant decrease in pulmonary ventilatory function after an intravenous injection of paclitaxel. To determine the role of mast cells in paclitaxel-induced pulmonary dysfunction in rats, the effects of several agents that arc used clinically for the prophylaxis of paclitaxel HSR were investigated. Sensory nerve fibers in the airways are found beneath the epithelium, near smooth muscle cells and submucosal glands, and around arterial vessels (18). In the airways, the release of the tachykinins, substance P, and neurokinin A from sensory nerves causes a rapid increase in microvascular leakage in the airways of patients with asthma (19), bronchoconstriction in human isolated bronchi (20), and infiltration of inflammatory cells in mice lung (21). The possible involvement of sensory nerves in the action of paclitaxel was subsequently discussed.
METHODS
Animals
Male Sprague-Dawley rats and mast cell-deficient rats Ws/Ws^sup -/-^ and their wild type were used in the present study. The experimental procedures were approved by the Committee for the Care and Use of Laboratory Animals at the Faculty of Medicine, Kyushu University.
MATERIALS
Paclitaxel injection was obtained from Bristol-Myers Squibb (Tokyo, Japan). LY303870 and SR48968 were kindly donated by Dr. Kenji Ohmori of Kyowa Hakko Kogyo Co., Ltd. (Shizuoka, Japan). Nafamostat mesilate was kindly donated by Torii Pharmaceutical Co., Ltd. (Tokyo, Japan). All other chemicals were of reagent grade.
Sensory Nerve Denervation
Rats were injected intraperitoneally with a total dose of 25 mg/kg capsaicin (10 injections over a 48-hour period), according to the method of Bret-Dibat and coworkers (22).
Measurement of Extravasation of Plasma Protein in Rat Lungs
The vascular permeability in lungs was evaluated by the Evans blue extravasation method, as described previously (23). Briefly, rats were injected intravenously with paclitaxel in combination with Evans blue (20 mg/kg) under pentobarbital anesthesia. At 10 minutes, lungs were perfused with physiologic saline through the pulmonary artery. A half of the lung tissues were dissected, and Evans blue was extracted into formamide. The remainder was dried in an oven at 60°C.
Measurement of Blood Gasses
Arterial gasses were monitored by using a gas analyzer (i-STAT Co., East Windor, NJ). A cannula (Angiocath, 24G; Deseret Medical Inc., Sandy, UT) was inserted into the femoral artery of anesthetized rats, and blood specimens were taken to monitor Pa^sub O^^sub 2^, Pa^sub CO^^sub 2^, and pH.
Determination of Histamine in Rat Lungs
The lung tissues were dissected and placed on paper filter, and adherent tissues were carefully removed and histamine concentration was determined by high-performance liquid chromatography, as described (24).
Determination of Neuropeptides and Protein in Rat Bronchoalveolar Lavage Fluid
Ten minutes after paclitaxel infusion, bronchoalveolar lavage fluid (BALF) was obtained by injecting 10 ml phosphate buffered-saline into trachea. BALF was centrifuged, and aliquots of supernatant were used for protein assay by the Bradford method. The remainder was used for determination of neuropeptides such as substance P, calcitonin gene-related peptide (CGRP), and neurokinin A. Before the assay for neuropeptides, samples were pretreated by applying to the C^sub 18^ column. The elutes were evaporated to dryness and reconstituted with assay buffer and determined by the enzyme immunoassay kit.
Histologic Examination
Lungs were immersed in 20% formalin-buffered saline and allowed to fix for 3 days. Ten-micrometer-thick sections obtained from the middle lobe of lungs were processed for standard hematoxylin and eosin staining.
Immunohistochemistry
Lung sections were subjected to immunohistochemical stains with monoclonal antibodies raised against substance P and CGRP. Briefly, lung sections were postfixed in 4% paraformaldehyde and incubated with anti-substance P developed in rabbit delipidized (Whole antiserum, Sigma Chemical, St. Louis, MO) or rabbit anti-CGRP (rat) IgG (Yanaihara Institute Inc., Shizuoka, Japan) at 1:2,000 dilutions. Biotin-labeled affinity-isolated goat anti-rabbit immunoglobulin was used as the secondary antibody and visualized by the DAKO LSAB System (DAKO A/S, Glostrup, Denmark).
Statistical Analyses
Data were statistically analyzed by one-way analysis of variance followed by the Bonferroni/Dunnett's test for multiple comparisons or by Student's t test for comparison between two groups (Stat View; Abacus Concepts, Berkeley, CA).
RESULTS
Paclitaxel-induced Vascular Hyperpermeability and Pulmonary Dysfunction in Rats
In rats anesthetized with pentobarbital-Na, intravenous injection of paclitaxel (10-20 mg/kg) caused a dose-dependent extravasation of plasma protein in the lung, as determined by the leakage of protein-conjugated Evans blue dye into pulmonary tissues (Figure 1A). To determine whether the vascular response is associated with paclitaxel itself or Cremophor EL, the effects of paclitaxel and the surfactant on pulmonary vascular permeability were compared. As shown in Figure 1B, Cremophor EL produced far less marked but significant increase in vascular permeability, thereby suggesting that the plasma extravasation after paclitaxel injection is mediated predominantly but not solely by paclitaxel itself. The pulmonary extravasation after paclitaxel injection was accompanied by dyspnea and pulmonary edema, thus the arterial gasses and pH were monitored as the pulmonary function after paclitaxel injection. As shown in Figure 2, the Pa^sub O^^sub 2^ decreased, whereas Pa^sub CO^^sub 2^ increased, transiently after paclitaxel injection (15 mg/kg). Arterial pH decreased slightly and not significantly after paclitaxel injection.
Effects of Clinically used Premedicative Agents on Paclitaxel-induced Pulmonary Vascular Hyperpermeability in Rats
Dexamethasone (1 and 10 mg/kg), when administered twice at 6 hours and 30 minutes before paclitaxel injection, caused a marked and dose-dependent attenuation of the paclitaxel-induced vascular response (Figure 3A). However, a single injection of dexamethasone even at 10 mg/kg (30 minutes before) did not reduce the vascular hyperpermeability induced by paclitaxel (Figure 3B). The paclitaxel-induced histologie changes in pulmonary sections as characterized by edema in perivascular regions were also ameliorated by dexamethasone (Figure 6A). On the other hand, the paclitaxel-induced pulmonary plasma extravasation was not affected by a histamine H^sub 1^ blocker diphenhydramine (10 mg/kg), an H^sub 2^ blocker famotidine (40 mg/kg), or their combination (Figure 4A). To determine whether tryptase, another mast cell ingredient, contributes to the action of paclitaxel, the effect of nafamostat mesilate, a potent inhibitor of mast cell tryptase (25), on the vascular response to paclitaxel was examined. As shown in Figure 4B, nafamostat mesilate at 10 mg/kg, a dose that produces a marked inhibition of radiographic contrast media-induced mast cell-mediated vascular hyperpermeability in rat lungs (25), did not affect the vascular action of paclitaxel.
Lack of Involvement of Mast Cells in Paclitaxel-induced Plasma Extravasation in Rat Lungs
To further confirm that mast cells are not important in the plasma extravasation induced by paclitaxel injection, the effect of paclitaxel on the vascular permeability was examined in mast cell-deficient rats Ws/Ws^sup -/-^. As shown in Figure 5B, the histamine content in lungs of Ws/Ws^sup -/-^ rats was extremely low and was approximately 0.7% of that in wild-type rats. Paclitaxel injection at 15 mg/kg caused a comparable or even more marked increase in vascular permeability in Ws/Ws^sup -/-^ rats than in wildtype rats. These data strongly suggest the lack of involvement of mast cells in paclitaxel-induced plasma extravasation in rats.
Role of Sensory Nerve Peptides in Paclitaxel-induced Pulmonary Dysfunction in Rats
The histopathologic changes in pulmonary sections induced by paclitaxel were reversed by capsaicin pretreatment (Figure 6A). The paclitaxel-induced plasma extravasation in lungs was also diminished by sensory denervation with repealed injection of capsaicin (Figure 7). These observations suggest an involvement of sensory nerves in the action of paclitaxel on pulmonary vessels. This idea was confirmed by the present immunohistochemical data indicating that a number of immunoreactive substances for CGRP and substance P appeared around the wall of pulmonary alveoli of rats injected with paclitaxel (Figure 6B), although there were no such immunoreaetive materials in the alveolar region of intact rats (data not shown).
Elevation of the Levels of Sensory Neuropeptides in BALF after Paclitaxel Injection
To further confirm that paclitaxel stimulates the release of sensory neuropeptides in lungs, the contents of CGRP, substance P, and neurokinin A were determined in BALF after paclitaxel injection. The protein and histamine contents in BALF were also measured. As shown in Figure 8A, the concentrations of protein as well as CGRP, substance P, and neurokinin A but not histamine were markedly elevated by paclitaxel injection (15 mg/kg). It was noteworthy that the extent of the rise in CGRP and substance P correlated well with the extent of protein leakage (Figure 8B): there were significant correlations between the protein content and CGRP level (r = 0.783, p
Involvement of NK^sub 1^ and NK^sub 2^ Receptors in Paclitaxel-induced Plasma Extravasation in Rat Lungs
To determine whether the stimulation of neurokinin receptors is implicated in the paclitaxel-induced pulmonary plasma extravasation, the effects of the selective antagonists for neurokinin NK^sub 1^ and NK^sub 2^ receptors and CGRP receptor on the vascular hyperpermeability induced by paclitaxel injection was studied. As shown in Figure 9, LY303870 (0.1 and 0.5 mg/kg), an NK^sub 1^ antagonist (26), and SR48968 (0.2 and 1 mg/kg), an NK^sub 2^ antagonist (27), produced a significant and concentration-dependent inhibition of the paclitaxel-induced increase in pulmonary vascular permeability in rats. The inhibition was more marked when LY303870 (0.5 mg/kg) and SR48968 (1 mg/kg) were administered in combination. Unlike NK^sub 1^ or NK^sub 2^ antagonists, a CGRP^sub 1^ antagonist peptide CGRP^sub 8-37^ (28) was not effective in reversing the action of paclitaxel (Figure 9B). Therefore, it is suggested that both NK^sub 1^ and NK^sub 2^ receptors are implicated in the paclitaxel-induced pulmonary dysfunction.
DISCUSSION
Paclitaxel was found to cause with high frequency (three of five patients) severe HSR in the Phase I study in the absence of any premedications (1). Wiernik and coworkers (9) also reported in the data in the Phase I study that severe (Grades 3-4) HSR occurred in 4 (30.8%) out of 13 courses of paclitaxel injection without any premedication. They also showed that the incidence was remarkably reduced by the premedication with dexamethasone, diphenhydramine, and cimetidine, in which moderate (Grade 2) HSR appeared in 3 (4.3%) out of 70 courses. Therefore, the treatment with histamine H^sub 1^ and H^sub 2^ antagonists in combination with glucocorticoids is inevitably performed before paclitaxel chemotherapy. Nevertheless, the HSR to paclitaxel has been reported to occur frequently with the incidence of 5 to 14% in patients with ovarian cancer (3, 8, 12). Therefore, it is suggested that chemical mediators other than histamine also contribute to the HSR to paclitaxel. The severe HSR is characterized by respiratory symptoms such as dyspnea, bronchospasm, and chest tightness.
In the present study, paclitaxel produced a marked increase in pulmonary vascular permeability as well as edema in rats. A transient decrease in Pa^sub O^sub 2^^ with a concomitant increase in Pa^sub CO^sub 2^^ was observed soon after injection of paclitaxel, indicating the reversible pulmonary dysfunction. The dose of paclitaxel (15 mg/kg) required to cause pulmonary dysfunction in rats was somewhat higher than the clinical dose of this agent (~ 5 mg/ kg) for the treatment of ovarian cancer. Pulmonary vascular hyperpermeability as well as pulmonary edema were remarkably alleviated by dexamethasone, only when the glucocorlicoid was administered twice at 6 hours and 30 minutes before paclitaxel injection. However, dexamethasone was no longer effective when administered once at 30 minutes before paclitaxel injection. The difference in the premedicative efficacy of dexamethasone depending on the time of dosing was also reported in the clinical setting, in which the incidence of HSR when dexamethasone was injected twice at 12 and 6 hours or once at 30 minutes before paclitaxel injection is 7.5 and 17.3%, respectively (29). In contrast, the paclitaxel-induced pulmonary protein extravasation in rats was not affected by histamine H^sub 1^ or H^sub 2^ blockers, thereby suggesting the lack of involvement of histamine. Nafamostat mesilate, a potent tryptase inhibitor (24), also had no influence on the vascular action of paclitaxel. We have previously reported in rats that nafamostat mesilate at the dose used in the present study dramatically reduced the pulmonary vascular hyperpermeability induced by iodinated radiographie contrast media (25), agents that cause mast cell degranulation (30, 31). Therefore, it is unlikely that the paclitaxel-induced protein extravasation in rats is attributable to mast cell ingredients. The lack of involvement of mast cells was further confirmed by the present findings, indicating that paclitaxel caused the similar vascular hyperpermeability in lungs of mast cell-deficient rats Ws/Ws^sup -/-^.
The capsaicin treatment by the present dosing regimen is reported to markedly reduce the visceral chemosensory function, as determined by the number of writhings after peripheral administration of phenylquinone, although the concentration of substance P in the spinal cord is lowered slightly (by 15%) but significantly in capsaicin-pretreated rats (22). Therefore, it is likely the tachykinins in C-fibers involving the nociception or inflammatory responses arc largely but incompletely reduced in the present capsaicin-pretreated rats. On the other hand, the paclitaxel-induced vascular response was largely reduced by the sensory denervation with repealed injections of capsaicin. The immunoreactive substances for substance P and CGRP appeared in pulmonary alveoli in paclitaxel-injected rats but not in intact animals. Moreover, the concentrations of sensory peptides such as substance P, CGRP, and neurokinin A as well as the protein content were all elevated in BALF after paclitaxel injection. However, there was no change in the histamine level in BALF after paclitaxel injection. It was noteworthy that the extent of the increase in the sensory peptides, particularly substance P and CGRP, was closely related to the elevation of protein content in BALF. On the other hand, the paclitaxel-induced pulmonary plasma extravasation was reversed by an NK^sub 1^ antagonist LY303870 (0.1 and 0.5 mg/kg) and an NK^sub 2^ antagonist SR48968 (0.2 and 1 mg/kg). The inhibition was more marked when both antagonists were treated in combination. It has been reported that the concentration that inhibits 50% values of LY303870 for inhibiting substance P-induced salivary response and decrease in arterial blood pressure in rats are 0.13 and 0.34 mg/kg, respectively (26), whereas the dose of SR48968 that strongly inhibits the contraction of rat urinary bladder induced by an NK^sub 2^ agonist [beta] [Ala^sup 8^] neurokinin A (4-10) is 55 µg/ kg, intravenously) (32). Therefore, the doses of these tachykinin antagonists used in the present study seemed to be enough to block these tachykinin receptors. However, the vascular response to paclitaxel was not blocked by a CGRP^sub 1^ receptor antagonist, CGRP^sub 8-37^. Taken together, it is strongly suggested that paclitaxel stimulates the release of sensory peptides including substance P, CGRP, and neurokinin A, which leads to the enhancement of vascular permeability and edema via stimulation of NK^sub 1^ and NK^sub 2^ receptors. Therefore, we report here for the first time that paclitaxel-induced acute pulmonary dysfunction is due to the neurogenic inflammation. On the other hand, it has been demonstrated that dexamethasone, when administered 4 hours before the onset of reaction, alleviates the neurogenic inflammation provoked in rat paw by an electrical stimulation of the sensory saphenous nerve, in which the paw edema is considered to result from increased microvascular permeability mediated via neurokinin NK^sub 1^ receptors (26). Thus, these data may explain why in the present study, dexamelhasone was effective only when it was administered at 6 hours and 30 minutes before paclitaxel injection.
Neurogenic inflammation is defined as the inflammatory responses mediated by the neuropeptides that are released from capsaicin-sensitive small-diameter sensory neurons (33). Intravenous injection of several tachykinins such as substance P and neurokinin A induces plasma extravasation markedly in the trachea and main bronchi and less prominently in the larynx and intrapulmonary airways of guinea pigs (34). Moreover, a study by Rogers and coworkers (35) on the roles for substance P and neurokinin A in guinea pig airway plasma extravasation has demonstrated that only NK^sub 1^ receptors play a role in producing plasma extravasation in the trachea and large airways, whereas showing significant roles for both NK^sub 1^ and NK^sub 2^ receptors in the extravasation in the lower airways (secondary bronchi and intraparenchymal airways). Marek and coworkers (36) have reported that in rabbit airway the inhalation of toluene diisocyanate causes the airway hyperresponsiveness to acetylcholine in a capsaicin-sensitive manner. They also showed that the responses are mimicked by substance P and neurokinin A and blocked by NK^sub 1^ and NK^sub 2^ antagonists, thereby suggesting that toluene diisocyanate stimulates the release of substance P and neurokinin A from sensory nerves to cause neurogenic airway hyperresponsiveness. Indeed, both of these tachykinin receptors are present in the airway: radiolabeled binding studies have shown in guinea pigs that NK^sub 1^ receptors labeled with [^sup 125^I] Bolton-Hunter-[Sar^sup 9^, Met (O2)^sup 11^] substance P distribute over the bronchial smooth muscle of large and small airways, bronchial epithelium, and pulmonary arterial smooth muscles, whereas NK^sub 2^ binding sites labeled with [^sup 125^I][Lys^sup 5^,Tyr(I^sub 2^)^sup 7^, MeLeu^sup 9^,Nle^sup 10^] neurokinin A-(4-10) are localized in bronchial smooth muscles of mainly large airways but not in other histologie regions (37). CGRP is another neuropeptide that colocalizes with substance P in sensory C-fiber afferents in the airways (38). But, unlike substance P or neurokinin A, CGRP is reported to possess no significant effect on the microvascular permeability (39, 40). Consistent with this finding, CGRP^sub 8-37^ was not effective in suppressing the paclitaxel-induced plasma extravasation in the present study. Because this peptide is a potent vasodilator, the enhanced release of CGRP may be associated with the flare and rush caused by paclitaxel injection.
In conclusion, a rat model of paclitaxel-induced pulmonary dysfunction was established in the present study. The paclitaxel-induced plasma extravasation and edema were reversed by dexamethasone but not by histamine H^sub 1^ or H^sub 2^ antagonists. The mast cell-deficient rats Ws/Ws^sup -/-^ also showed the similar pulmonary response to paclitaxel as compared with the wild-type animals. Therefore, it is unlikely that mast cells are involved in the initiation of paclitaxel-induced pulmonary vascular hyperpermeability. The vascular response to paclitaxel was reduced by sensory denervation with capsaicin or pretreatment with NK^sub 1^ and NK^sub 2^ antagonists. Paclitaxel stimulated the release of sensory peptides such as substance P, CGRP and neurokinin A but not histamine in BALF of rats. These findings suggest that sensory neuropeptides rather than mast cell histamine are closely associated with the paclitaxel-induced pulmonary dysfunction.
Conflict of Interest Statement: Y.I. has no declared conflict of interest; T.S. has no declared conflict of interest; T.H. has no declared conflict of interest; T.G. has no declared conflict of interest; S.T. has no declared conflict of interest; H.Y. has no declared conflict of interest; H.N. has no declared conflict of interest; R.O. has no declared conflict of interest.
References
1. Kris MG, O'Connell JP, Gralla RJ, Wertheim MS, Parente RM, Schiff PB, Young CW. Phase I trial of taxol given as a 3-hour infusion every 21 days. Cancer Treat Rep 1986;70:605-607.
2. Weiss RB, Donehower RC, Wiernik PH, Ohnuma T, Gralla RJ, Trump DL, Baker JR Jr, Van Echo DA, Von Hoff DD, Leyland-Jones B. Hypersensitivity reactions from taxol. J Clin Oncol 1990;8:1263-1268.
3. Cormio G, Di Vagno G, Melilli GA, Cazzolla A, Di Gesu G, Carriero C, Cramarossa D, Loverro G, Selvaggi L. Hypersensitivity reactions in ovarian cancer patients receiving paclitaxel. J Chemother 1999; 11:407-409.
4. Price KS, Castells MC. Taxol reactions. Allergy Asthma Proc 2002;23: 205-208.
5. Gelderblom H, Verweij J, Nooter K, Sparreboom A. Cremophor EL: the drawbacks and advantages of vehicle selection for drug formulation. Eur J Cancer 2001;37:1590-1598.
6. Nuijen B, Bouma M, Schellens JH, Beijnen JH. Progress in the development of alternative pharmaceutical formulations of taxanes. Invest New Drugs 2001;19:143-153.
7. Decorti G, Klugmann FB, Candussio L, Baldini L. Effect of paclitaxel and Cremophor EL on mast cell histaminc secretion and their interaction with adriamycin. Anticancer Res 1996;16:317-320.
8. Lorenz W, Reimann HJ, Schmal A, Dormann P, Schwarz B, Neugebauer E, Docnieke A. Histaminc release in dogs by Cremophor El and its derivatives: oxethylated oleic acid is the most effective constituent. Agents Actions 1997;7:63-67.
9. Wiernik PH, Schwartz EL, Strauman JJ, Dulcher JP, Lipton RB, Paietta E. Phase I clinical and pharmacokinetic study of Taxol. Cancer Res 1987;47:2486-2493.
10. Bitton RJ, Figg WD, Reed E. A preliminary risk-benefit assessment of paclitaxel. Drug Saf 1995;12:196-208.
11. Boehm DK, Maksymiuk AW. Paclilaxcl premedication regimens. J Natl Cancer Inst 1996;88:463-465.
12. Markman M, Kennedy A, Webster K, Peterson G, Kulp B, Belinson J. An effective and more convenient drug regimen for prophylaxis against paclitaxel-associated hypersensitivity reactions. J Cancer Res Clin Oncol 1999;125:427-429.
13. Kwon JS, Elit L, Finn M, Hirte H, Mazurka J, Moens F, Trim K. A comparison of two prophylactic regimens for hypersensitivity reactions to paclitaxel. Gynecol Oncol 2002;84:420-425.
14. Rowinsky EK, Donehower RC. Paclitaxel (Taxol). N Engl J Med 1995; 332:1004-1014.
15. Bookman MA, Kloth DD, Kover PE, Smolinski S, Ozols RF. Short-course intravenous prophylaxis for paclitaxel-related hypersensitivity reactions. Ann Oncol 1997;8:611-614.
16. Olson JK, Sood AK, Sorosky JI, Anderson B, Buller RE. Taxol hypersensitivity: rapid retreatment is sale and cost effective. Gynecol Oncol 1998;68:25-28.
17. Markman M, Kennedy A, Webster K, Kulp B, Peterson G, Belinson J. Paclitaxel-associated hypersensitivity reactions: experience of the gynecologic oncology program of the Cleveland Clinic Cancer Center. J Clin Oncol 2000;18:102-105.
18. Baluk P. Neurogenic inflammation in skin and airways. J Investig Dermatol Symp Proc 1997;2:76-81.
19. Van Ransen ELJ, Hiemstra PS, Rabe KF, Sterk PJ. Assessment of microvascular leakage via sputum induction. Am J Respir Crit Care Med 2002;165:1275-1279.
20. Amadesi S, Moreau J, Tognetto M, Springer J, Trevisani M, Naline E, Advenier C, Fisher A, Vinci D, Mapp C, et al. NK1 receptor stimulation causes contraction and inositol phosphate increase in medium-size human isolated bronchi. Am J Respir Crit Care Med 2001;163:1206-1211.
21. Graham RM, Friedman M, Hoyle GW. Sensory nerves promote ozone-induced lung inflammation in mice. Am J Respir Crit Care Med 2001; 164:307-313.
22. Bret-Dibat JL, Creminon C, Couraud JY, Kelley KW, Dantzer R, Kent S. Systemic capsaicin pretreatment fails to block the decrease in food-motivated behavior induced by lipopolysaccharide and interleukin-1beta. Brain Res Bull 1997;42:443-449.
23. Sendo T, Kataoka Y, Takeda Y, Furuta W, Oishi R. Nitric oxide protects against contrast media-increased pulmonary vascular permeability in rats. Invest Radiol 2000;35:472-478.
24. Itoh Y, Oishi R, Adachi N, Saeki K. A highly sensitive assay for histamine using ion-pair HPLC coupled with postcolumn fluorescent derivatization: its application to biological specimens. J Neurochem 1992;58: 884-889.
25. Sendo T, Itoh Y, Goromaru T, Sumimura T, Saito M, Aki K, Yano T, Oishi R. A potent tryptase inhibitor nafamostat mesilate dramatically suppressed pulmonary dysfunction induced in rats by a radiographic contrast medium. Br J Pharmacol 2003;138:959-967.
26. Cellier E, Fayolle C, Hipskind PA, Iyengar S, Couture R. Peripheral effects of three novel non-peptide tachykinin NK^sub 1^ receptor antagonists in the anaesthetized rat. Eur J Pharmacol 1996;318:377-385.
27. Emonds-Alt X, Vilain P, Goulaouic P, Proietto V, Van Broeck D, Advenier C, Naline E, Neliat G, Le Fur G, Breliere JC. A potent and selective non-peptide antagonist of the neurokinin A (NK^sub 2^) receptor. Life Sci 1992;50:PL101-PL106.
28. Gardiner SM, Compton AM, Kemp PA, Bennett T, Bose C, Foulkes R, Hughes B. Antagonistic effect of human alpha-CGRP^sub 8-37^ on the in vivo regional haemodynamic actions of human alpha-CGRP. Biochem Biophys Res Commun 1990;171:938-943.
29. Kwon JS, Elit L, Finn M, Hirte H, Mazurka J, Moens F, Trim K. A comparison of two prophylactic regimens for hypersensitivity reactions to paclitaxel. Gynecol Oncol 2002;84:420-425.
30. Laroche D, Aimone-Gastin I, Dubois F, Huel H, Gerard P, Vergnaud MC, Mouton-Faivre C, Gueant JL, Laxenaire MC, Bricard H. Mechanisms of severe, immediate reactions to iodinated contrast material. Radiology 1998;209:35-36.
31. Saito M, Itoh Y, Yano T, Sendo T, Goromaru T, Sakai N, Oishi R. Roles of intracelluiar Ca^sup 2+^ and cyclic AMP in mast cell histamine release induced by radiographie contrast media. Naunyn Schmiedeberg's Arch Pharmacol 2003;367:364-371.
32. Maggi CA, Patacchini R, Giuliani S, Giachetti A. In vivo and in vitro pharmacology of SR 48,968, a non-peptide lachykinin NK^sub 2^ receplor antagonist. Eur J Pharmacol 1993;234:83-90.
33. Holzer P. Local effector functions of capsaicin-sensitive sensory nerve endings: involvement of tachykinins, calcitonin gene-related peptide and other neuropeptides. Neuroscience 1988;24:739-768.
34. Martling CR. Sensory nerves containing tachykinins and CGRP in the lower airways: functional implications for bronchoconstriction, vasodilation and protein extravasation. Acta Physiol Scand 1987;563:1-57.
35. Rogers DF, Belvisi MG, Aursudkij B, Evans TW, Barnes PJ. Effects and interactions of sensory neuropeptides on airway microvascular leakage in guinea-pigs. Br J Pharmacol 1988;95:1109-1116.
36. Marek W, Potthast JJ, Marcynski B, Baur X. Role of substance P and neurokinin A in toluene diisocyanate-induced increased airway responsiveness in rabbits. Lung 1996;174:83-97.
37. Stigas J, Burcher E. Autoradiographic localization of tachykinin NK2 and NK1 receptors in the guinea-pig lung, using selective radioligands. Eur J Pharmacol 1996;311:177-186.
38. Lundberg JM, Franco-Cereceda A, Hua XY, Hokfelt T, Fischer JA. Co-existence of substance P and calcitonin gene-related peptide immunoreactivities in sensory nerves in relation to cardiovascular and bronchoconstrictor effects of capsaicin. Eur J Pharmacol 1985;108:315-319.
39. Martling CR. Sensory nerves containing tachykinins and CGRP in the lower airways: functional implications for bronchoconstriction, vasodilation and protein extravasation. Acta Physiol Scand 1987;563:1-57.
40. Rodger IW, Tousignant C, Young D, Savoie C, Chan CC. Neurokinin receptors subserving plasma extravasation in guinea pig airways. Can J Physiol Pharmacol 1995;73:927-931.
Yoshinori Itoh, Toshiaki Sendo, Toshio Hirakawa, Takeshi Goromaru, Shinya Takasaki, Hideaki Yahata, Hitoo Nakano, and Ryozo Oishi
Department of Hospital Pharmacy, Faculty of Medicine; and Department of Obstetrics and Gynecology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan
(Received in original form July 5, 2003; accepted in final form October 8, 2003)
Correspondence and requests for reprints should be addressed to Toshiaki Sendo, Ph.D., Department of Hospital Pharmacy, Faculty of Medicine, Kyushu University, 3-1-1 Maidashi, Higashi-ku, Fukuoka 812-8582, Japan. E-mail: sendou@st.hosp. kyushu-u.ac.ip
Copyright American Thoracic Society Jan 1, 2004
Provided by ProQuest Information and Learning Company. All rights Reserved