Critical illness polyneuropathy (CIP) is most often associated with sepsis or multiorgan dysfunction syndrome. Although the incidence of CIP among all patients in intensive care units is low, only about 2% (1), patients with other primary diagnoses have also had CIP diagnosed. This case study describes the suspected pathophysiology, clinical features, and treatment of CIP.
Case Study
T.R. is a 60-year-old man with marked risk factors for heart disease, including a history of cardiac disease in his maternal relatives, use of tobacco, hypertension, obesity, and non-insulin-dependent diabetes mellitus. He arrived at a local emergency department with unstable angina and an inferior myocardial infarction. He was then transferred to another local hospital, where he had cardiac catheterization. Three-vessel coronary artery disease was diagnosed, and left ventricular ejection fraction was 0.15 to 0.20. While T.R. was being scheduled for coronary artery bypass graft (CABG) surgery, ventricular tachycardia developed and required placement of an intra-aortic balloon pump to improve perfusion and halt ischemia.
T.R. underwent CABG surgery with saphenous vein grafts to the left anterior descending and the posterior descending coronary arteries. A large pericardial effusion and a transmural infarct with necrosis were found. The left ventricle was in danger of rupturing. In addition to the CABG surgery, a patch repair with biological glue and felt was done. Postoperatively, T.R. remained critically ill with multiple complications. On 2 occasions, he had respiratory insufficiency that required prolonged mechanical ventilation and reintubation. Thrombocytopenia associated with anemia developed and required multiple transfusions of blood products. T.R.'s condition remained hemodynamically unstable, and liver dysfunction developed. In addition, he had Staphylococcus epidermidis septicemia due to an infection at the catheter insertion site. Because of the severity of his illness, T.R. was sedated to reduce oxygen consumption and allow him to rest. After 2 weeks, his condition stabilized, and he was weaned off the sedatives. At that point, flaccid tetraparesis was detected.
Findings on Physical Examination
Two weeks after CABG surgery, T.R.'s most important neurological deficits were generalized weakness and restriction of movement manifested as flaccid tetraparesis. T.R. was awake and alert, and he occasionally followed simple commands by flickering his extremities. His spontaneous movement was minimal, and distal sensation was diminished.
An electromyography study was conducted 15 days after the CABG surgery. The right lower extremity showed a marked decrease in the amplitude of the tibial response, although conduction velocity was preserved. Distal latency was prolonged. T.R. had no peroneal response in the right lower extremity from the extensor digitorum brevis muscle and no sural response. Similar nerve conduction responses were noted in the left lower extremity, with the exception of the proximal tibial area, which had increased insertional activity in the tibialis anterior muscle, and the response of the vastus lateralis muscle, which showed possible insertional activity. Increased insertional activity in the extensor hallucis longus muscle also was apparent. Spontaneous activity was noted in the vastus lateralis and tibialis anterior muscles. T.R.'s lumbar paraspinal responses were not studied because his medical condition made turning him inadvisable. The diagnosis based on the electromyographic findings was polyneuropathy with indications of acute denervation at multiple levels.
On postoperative day 46, T.R. was transferred to a larger tertiary care hospital for continued management of the cardiovascular problems and the polyneuropathy. He was examined by a neurologist at the time of admission to evaluate the polyneuropathy. The examination yielded the following findings: T.R. was awake, alert, and oriented; his pupils were midline, equal, round, and reactive to light; his extraocular movements were intact, and he had positive corneal reflexes to threats; cranial nerves V, VII, VIII, IX, and X were intact; and cranial nerve XI was intact on the right side, but there was no movement of cranial nerve XI on the left side. His extremities were flaccid throughout, with 1/5 strength in the right upper and lower extremities and 2/5 strength in the left upper and lower extremities. Sensation was intact to light touch, with facial grimacing to pain, but no withdrawal. He had no deep tendon reflexes. Coordination could not be assessed because of the lack of motor activity. The diagnosis was CIP most likely due to multiorgan failure and sepsis.
Several laboratory tests were done when T.R. was admitted to the larger tertiary care hospital. An analysis of serum electrolytes revealed the following: sodium 159 mmol/L, potassium 3.7 mmol/L, chloride 128 mmol/L, carbon dioxide 23 retool/L, serum urea nitrogen 28.9 mmol/L (81 mg/dL), creatinine 80 [micro]mol/L (0.9 mg/dL), glucose 7.3 mmol/L (132 mg/dL), calcium 1.98 mmol/L (7.9 mg/dL), magnesium 1.15 mmol/L (2.8 mg/dL), and phosphorus 0.81 mmol/L (2.5 mg/dL). The results of a complete blood cell count were as follows: hemoglobin 87 g/L, hematocrit 0.26, white blood cell count 5.0 x [10.sup.9]/L, and platelets 142 x [10.sup.9]/L. The results of coagulation studies were prothrombin time 17 seconds, partial thromboplastin time 37.2 seconds, and international normalized ratio 1.9. Other results of laboratory tests were as follows: digoxin 2.0 nmol/L (1.6 ng/mL), creatine kinase 35 U/L, amylase 43 U/L, lipase 144 U/L, direct bilirubin 17 umol/L (1.0 mg/dL), delta bilirubin 14 [micro]mol/L (0.8 mg/dL), unconjugated bilirubin 10 [micro]mol/L (0.6 mg/dL), conjugated bilirubin 3 [micro]mol/L (0.2 mg/dL), total bilirubin 27 [micro]mol/L (1.6 mg/dL), alkaline phosphatase 275 U/L, aspartate transaminase 84 U/L, and alanine transaminase 38 U/L.
Before his admission to the tertiary care center, T.R. had received a full 14-day course of vancomycin for S epidermidis sepsis and therefore did not require any further antibiotic therapy. His most recent blood cultures had shown no growth. He remained markedly hypotensive, however, requiring a phenylephrine infusion, and was febrile at 38.1[degrees]C. He appeared to be in either septic or cardiogenic shock. An echocardiogram revealed a rupture of the inferior wall of the left ventricle with brisk flow into the rupture. The left atrium was compressed by a pseudoaneurysm, causing the cardiogenic shock. Urgent reoperation was required.
On postoperative day 49, T.R. was taken to the operating room and underwent a second sternotomy with a repair of the left ventricular rupture and pseudoaneurysm with placement of a Dacron polyester fiber patch. He remained in the operating room for 4 hours after the repair and had signs of disseminated intravascular coagulation, for which he was given massive transfusions of blood products. After surgery, he was taken to the cardiothoracic surgical intensive care unit, where he required intravenous pharmacological inotropic and vasopressive support, antiarrhythmic therapy for atrial fibrillation, ventilator support for pulmonary function, total parenteral nutrition for severe malnutrition, and slow continuous ultrafiltration for decreased urine output to manage fluid overload despite a normal creatinine level.
T.R. was successfully extubated on postoperative day 3 (total hospitalization day 52) and was cleared to receive a regular diet, although he did require assistance with feeding because of the persistent tetraparesis. The intravenous pharmacological inotropic and vasopressive support was eventually diminished and discontinued. Liver dysfunction did not worsen. The platelet count returned to normal, but anemia related to fluid shifts persisted. Despite therapy, the atrial fibrillation continued and necessitated anticoagulation with warfarin. The remainder of T.R.'s care was supportive. The neurologists thought that the polyneuropathy would resolve within weeks to months but would require long-term rehabilitation after discharge. T.R. was discharged to a rehabilitation center on day 26 after the second sternotomy and left ventricular pseudoaneurysm repair (total hospitalization day 75). He recovered fully from the polyneuropathy after approximately 7 months of intense rehabilitation at the center and at home.
Discussion
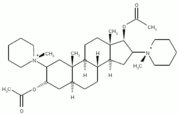
CIP, named by Bolton and colleagues, (1-3) has been recognized and well studied for the past 2 decades. CIP is a self-limiting acute axonal neuropathy that develops during the treatment of severely ill patients. (4) It is often characterized by severe, generalized muscle weakness without bulbar involvement (5) and is often associated with unexplained difficulty in weaning from mechanical ventilation. (3) Although the etiologic factors and exact pathological mechanism of action are not known, (6) sepsis and multiorgan dysfunction syndrome have been most often associated with the development of CIP. (1,4) CIP has been associated with etiologic conditions such as prolonged mechanical ventilation, (7) malnutrition, (3) vitamin deficiencies, (3) immunologic causes, (8) toxin-producing bacteria, (8) coagulopathies, (8) use of aminoglycosides (gentamicin), (4,9) use of neuromuscular blocking agents (pancuronium bromide), (4,9) and hyperosmolality or changes in osmolality. (10)
CIP is the most common neuromuscular condition acquired in the ICU. (11) CIP develops in 50% to 70% of patients who have sepsis lasting longer than 2 weeks. (11) In a prospective study, (3) CIP developed in 70% to 80% of patients who had severe sepsis and multiorgan failure. CIP occurs in 2% of all patients in ICUs. (1) CIP is most likely to develop in severely ill patients who have both systemic inflammatory response syndrome and an elevated score on the Acute Physiology and Chronic Health Evaluation III, a scoring system used to assess mortality risk in ICU patients. (9) The onset of CIP can occur as early as 3 days after the diagnosis of sepsis or systemic inflammatory response syndrome. (4)
The clinical relevance of CIP is related to several factors such as the frequency with which it occurs, (12) prolonging stays in the hospital and ICU, (12,13) increasing duration of mechanical ventilation and risk of ventilator-acquired pneumonia, (13) and necessitating subsequent care and physical rehabilitation. (13) The financial, psychological, and emotional toll on affected patients and their families is considerable. (13)
Pathophysiology
CIP is characterized by an axonal distal degeneration of sensory and motor fibers. (1,8) The pathogenesis of CIP remains unknown, although multiple processes have been considered. In 1996, Bolton (14) proposed that axonal degeneration may be caused by factors attributed to sepsis, such as the presence of tumor necrosis factor, histamines, and arachidonic acid metabolites; the activation of the complement and cell adhesion systems; and the formation of local free radicals. (12) Bolton suggested that the mechanism of action was an alteration in the microcirculation of peripheral nerves. (3) Therefore, the peripheral nervous system is regarded as yet another organ system that succumbs to the adverse effects of sepsis manifesting itself as CIP. (3)
Despite much research (8,11,12,14-16) supporting the idea that sepsis and factors associated with multiorgan failure cause CIP some conflicting findings exist. (6,15) CIP has been observed after respiratory failure, acute episodes of hypotension, and trauma without evidence of sepsis or multiple organ dysfunction syndrome. (3,6,17) Hence, the exact mechanism of action remains undetermined.
Clinical Manifestations
Typical signs and symptoms of CIP that warrant a neurological consultation are unexplained difficulty in weaning from mechanical ventilation (3) and severe generalized muscle weakness. (18) Signs and symptoms may be clinically occult (2) in 50% of cases. (11) Findings on physical assessment include muscular atrophies, severe flaccid tetraparesis, and decreased or absent deep tendon reflexes, (4,12) although deep tendon reflexes may be normal in one third of patients with CIP. (3,4) In fact, deep tendon reflexes may be exaggerated in patients who have a central nervous system lesion coincidental with CIP. (3) Cranial nerves are usually intact. (12) Some researchers (16,18) reported an inconsistency in documented clinical assessment findings with respect to the degree and distribution of muscle atrophy and wasting, changes in deep tendon reflexes, and prevalence of sensory alterations. Abnormalities in laboratory values typically reflect the underlying sepsis or organ failure. (1)
Diagnosis
The most important alternative possibility in the differential diagnosis of CIP is Guillain-Barre syndrome, which is a well-documented complication of severe infection. (1,19) Unremarkable protein levels in cerebrospinal fluid, electrophysiological findings of primary axonal degeneration, and lack of significant inflammatory changes of peripheral nerves differentiate CIP from Guillain-Barre syndrome. (1,15,19)
Difficulty in performing physical assessments of patients affected with CIP may impair diagnosis. (6) Patients who are intubated, sedated, and receiving neuromuscular blocking agents and may have encephalopathy (1,6) require an advanced level of clinical expertise in order to perform the neurological examination. (6) Without this level of expertise, accurate findings may be elusive. CIP may be falsely diagnosed in patients with primary central nervous system lesions, paresis, edema, or atrophy. (6) Last, the nerve conduction studies needed to diagnose CIP may not be readily accessible in many ICUs. (6)
Treatment
Presently, no specific treatment for CIP is available. (1,3) The management of a patient with CIP is focused on treating the underlying critical illness. (1,4) Evidence from a large prospective randomized trial (20) suggests that prevention of CIP and reduction in mortality by 40% are possible with intense insulin therapy in critically ill patients. In addition, preliminary retrospective chart analysis suggested that early administration of intravenous immunoglobulins may prevent or lessen the development of CIP. (21)
Treatment specific to CIP is supportive and should include psychological support for patients and their families, (1,4) pain control if necessary, and frequent neurological assessments. Treatment of the non-neurological signs and symptoms depend on the severity of the illness and must be individualized for each patient. Thorough skin care, prevention of pressure ulcers, aggressive physical therapy including range of motion exercises, and prophylaxis of deep vein thrombosis must be included in the plan of care.
Conclusion
Most authorities concur that a diagnosis of CIP should not precipitate a reduction in treatment intensity, (3) because patients with mild to moderate disease often have a lull recovery. (3,5) Recovery is limited and mortality is higher in patients with more severe polyneuropathy. (22) The prognosis for survivors of CIP ranges from a complete recovery over several months with disappearance of neurophysiological signs to chronic weakness with signs of denervation up to 5 years after discharge from the ICU. (22)
In order to allow the best possible recovery after the sepsis or multiorgan dysfunction syndrome is successfully treated, the signs and symptoms of CIP must be recognized and measures must be taken to prevent any further deterioration of new muscle and joint function. Equally important, healthcare providers should be aware that CIP does not occur solely in patients who have a primary diagnosis of sepsis. It also occurs in patients who have complications after major surgery, such as CABG surgery, as was the situation in this case study.
REFERENCES
(1.) Piper S. Koetter K, Triem J, et al. Critical illness polyneuropathy following cardiac surgery. Scand Cardiovasc J. 1998:32:309-312.
(2.) Bolton C, Laverty D, Brown J, Witt N, Hahn A, Sibbald W. Critically ill polyneuropathy: electrophysiological studies and differentiation from Guillain-Barre syndrome. J Neurol Neurosurg Psychiatry. 1986:49:563-573.
(3.) Hund E. Critical illness polyneuropathy. Curr Opin Neurol. 2001;14:649-653.
(4.) van Mook W, Hulsewe-Evers R. Critical illness polyneuropathy. Curr Opin Crit Care. 2002:8:302-310.
(5.) Zifko U. Long-term outcome of critical illness polyneuropathy. Muscle Nerve Suppl. 2000:9:S49-S52.
(6.) Hund E, Fogel W, Krieger D, DeGeorgia M, Hacke W. Critical illness polyneuropathy: clinical findings and outcomes of a frequent cause of neuromuscular weaning failure. Crit Care Med. 1996;24:1328-1333.
(7.) Hund E, Genzwurker H. Bohrer H, Jakob H, Thiele R, Hacke W. Predominant involvement of motor fibres in patients with critical illness polyneuropathy. Br J Anaesth. 1997:78:274-278.
(8.) Bolton C, Gilbert J. Hahn A, Sibbald W. Polyneuropathy in critically ill patients. J Neurol Neurosurg Psychiatry. 1984:47:1223-1231.
(9.) de Letter M, Schmitz P, Visser L, et al. Risk factors for the development of polyneuropathy and myopathy in critically ill patients. Crit Care Med 2001;29:2281-2286.
(10.) Waldhausen E, Keser G, Schulz B, Lippers P. Weaning failure due to acute neuromuscular disease. Crit Care Med. 1989;17:594-595.
(11.) Bolton C, Young B, Zochodne D. The neurological complications of sepsis. Ann Neurol. 1993;33:94-100.
(12.) Hund E. Neurological complications of sepsis: critical illness polyneuropathy and myopathy. J Neurol. 2001:248:929-934.
(13.) Marinelli W, Leatherman J. Neuromuscular disorders in the intensive care unit. Crit Care Clin. 2002;18:915-929.
(14.) Bolton C. Sepsis and the systemic inflammatory response syndrome: neuromuscular manifestations. Crit Care Med 1996:24:1408-1416.
(15.) Zochodne D, Bolton C, Wells G. et al. Critical illness polyneuropathy: a complication of sepsis and multiple organ failure Brain. 1987:110:819-842.
(16.) Leijten F, Weerd A. Critical illness polyneuropathy: a review of literature, definition and pathophysiology. Clin Neurol Neurosurg, 1994:96:10-19.
(17.) Leijten F, Weerd A, Poortvliet D, De Ridder V. Ulrich C, Harinck-De Weerd J. Critical illness polyneuropathy in multiple organ dysfunction syndrome and weaning from the ventilator. Intensive Care Med. 1996;22:856-861.
(18.) Zifko UA, Zipko HT, Bolton CF. Clinical and electrophysiological findings in critical illness polyneuropathy. J Neurol Sci 1998:159:186-193.
(19.) Op de Coul A, Lambregts P, Koeman J, Van Puygenbroek M, Ter Laak H, Gabreels-Festen A. Neuromuscular complications in patients given Pavulon (pancuronium bromide) during artificial ventilation. Clin Neurol Neurosurg. 1985:87:17-22.
(20.) Van den Berghe G, Wouters P, Weckers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359-1367.
(21.) Mohr M, Englisch L, Roth A, Burchardi H, Zielmann S. Effects of early treatment with immunoglobulin on critical illness polyneuropathy following multiple organ failure and gram-negative sepsis. Intensive Care Med. 1997;23:1144-1149.
(22.) Fletcher S, Kennedy D, Ghosh I, et al. Persistent neuromuscular and neurophysiologic abnormalities in long-term survivors of prolonged critical illness. Crit Care Med. 2003:31:1012-1016.
By April Marissa Keaveney, RN, MSN, CRNP, CCRN. From the School of Nursing University of Pennsylvania Philadelphia, Pa.
COPYRIGHT 2004 American Association of Critical-Care Nurses
COPYRIGHT 2004 Gale Group