INTRODUCTION: The annual incidence of malignant mesothehomas in the United States is 2200 cases per year, of which 70% are linked to asbestos exposure (1). Osteosarcomatous differentiation of this tumor has been reported in 14 cases (2, 3). We report a case of a patient who presented with a large pleural effusion, very densely calcified pleural plaques and an abnormal bone scan.
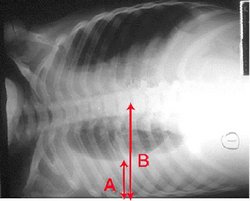
CASE PRESENTATION: The patient was a 79 year old man, non-smoker, who before retiring, had worked in construction and had been employed for 2 years as a shipyard worker unloading bags of asbestos. He had a history of pseudobulbar palsy and of prostate cancer that was treated successfully with surgery alone 2 years before the current illness. On routine blood testing, an elevated alkaline phosphate was noted and a bone scan showed intense uptake along the sternum and the entire adjacent right ribcage, which was interpreted as possible bony metastasis. The patient complained of increasing dyspnea, pleuritic chest pain and cough. Computed tomography of the thorax (figure 3) showed a large right pleural effusion with almost complete collapse and retraction of the right lung. Additionally, there was a 2.5 cm low density soft tissue mass attached to thickened and irregular calcified pleura. Analysis of fluid obtained by thoracocentesis showed an exudate with lymphocytosis and no malignant cells. Microscopic examination from a video-assisted thoracoscopy (VATS) and pleural biopsy showed a malignant tumor composed of spindle and polygonal cells, the latter intimately associated with osteoid (Figure 2). No epithelioid cells were identified. Immunohistochemical study showed strong positive reactions for keratin AE1 and AE3 in the spindle cells; the reaction for calretinin was negative. These findings were consistent with a mesothelioma with osteosarcomatous differentiation. The patient elected for palliative treatment. Three months after his VATS, the patient was admitted for pneumonia and passed away. At autopsy, tumor completely surrounded the tight lung (figure 3) and spread along the major fissure and focally into the superficial lung parenchyma. A Faxitron image (Figure 4) confirmed extensive ossification. Microscopic examination showed the tumor to consist almost entirely of malignant osteoid, with only a few small foci of undifferentiated spindle cell tumor.
[FIGURE OMITTED]
DISCUSSIONS: Four histologic mesothelioma subtypes exist (WHO 2004 classification): epithelioid, sarcomatoid, desmoplastic and biphasic. The sarcomatoid type, seen in 15% of cases, is characterized pathologically by spindle-shaped cells similar to those seen in fibrosarcomas. Rarely, foci of cartilagenous and/or osseous differentiation, as in our case, are seen. The extent of osseous metaplasia here is exceptional. The principal differential diagnostic considerations are primary sarcoma of the pleura and extension of a sarcoma of the rib or a sarcomatoid carcinoma of the lung into the pleural space. Keratin expression on immunohistochemical study will usually be sufficient to exclude the first two of these. However, a small peripheral pulmonary tumor may show an immunohistochemical profile similar to sarcomatoid mesothelioma and also may be difficult to detect by radiologic imaging. Definitive exclusion of such a lung primary may require autopsy examination.
CONCLUSION: Osteosarcomatous differentiation of mesothelioma is rare and the diagnosis can be challenging. While the sarcomatoid type mesothelioma portends a poorer prognosis in general, it is unclear if osteosarcomatous differentiation heralds an even worse outcome.
REFERENCES:
(1) Antman KH. Natural history and epidemiology of malignant mesothelioma. Chest 1993;103(4Suppl):373S-376S
(2) Raizon A, et al Calcification as a sign of sarcomatous degeneration of malignant pleural mesotheliomas: new CT finding. Journal of Coumputed Assisted Tomography. 1996;20:42-44.
(3) Quoix E et al. A left pleural effusion with a calcified tumoral mass and left hemithoracic uptake on bone scan. Lung Cancer 2001;32:203-305.
(4) Pistolesi M, Rusthoven J. Malignant Pleural Mesothelioma: Update, Current Management, and Newer Therapeutic Strategies. Chest 2004;126:1318-1329.
DISCLOSURE: Mariam Louis, None.
Mariam Louis MD * James Gruber MD Richard Fraser MD McGill University, Montreal, PQ, Canada
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group