To the Editor:
We read with great interest the recent case report in CHEST (September 2004) (1) by Norman et al, in which eosinophilic pneumonia preceded the establishment of rheumatoid arthritis (RA). We would like to add some comments to that precious case report. RA, a polarized disease of representative T helper (Th) type 1 cells, is less compatible with the coexistence of allergic disorders with a Th2 cytokine pattern than with other inflammatory diseases. However, previous studies (2,3) have demonstrated the coexistence of Th2 diseases, such as bronchial asthma and atopic dermatitis, and Th1 diseases, such as RA, insulin-dependent diabetes mellitus, and celiac disease. Kero and colleagues (3) have indicated that the presence of Th2 diseases in subjects with Th1 diseases may be related to environmental factors. The most recognized and important effector ceils in Th2 diseases are eosinophils. We are, therefore, interested in the chemoattraetant factors of eosinophils in the patient reported by Norman and colleagues. (1) Immunohistochemical examinations of Th2 cytokines, including interleukin (IL)-4 and IL-5, and chemokines such as eotaxin in lung tissue specimens from the patient would provide further important information.
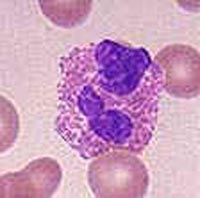
We are also concerned about the character of the arthritis in the patient. There are few case reports (4,5) of eosinophilic synovitis in the literature. If Norman and colleagues (1) collected synovial fluid from the patient, was eosinophilia detected in the fluid samples?
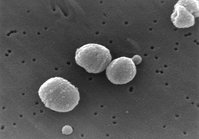
Finally, we think that Figure 2 in the article by Norman et al (1) cannot clearly identify the infiltration of eosinophils. We often stain the bronehoalveolar fluid and lung tissue specimens (Diff-Quik; International Reagents; Kobe, Japan) to determine the differential cell counts. (6,7) Thus, staining of the lung specimens might have yielded a different image.
Ken-ichiro Inoue, MD
Hirohisa Takano, PhD
Rie Yanagisawa, PhD
National Institute for Environmental Studies
Tsukuba, Japan
Toshikazu Yoshikawa, PhD
Kyoto Prefectural University of Medicine
Kyoto, Japan
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: Ken-ichiro Inoue, MD, Inhalation Toxicology Research Team, and Pathophysiology Research Team, National Institute for Environmental Studies, 16-2 Onogawa, Tsukuba, 305-8506, Japan; e-mail: inoue.kenichirou@nies.go.jp
REFERENCES
(1) Norman D, Piecyk M, Roberts DH. Eosinophilic pneumonia as an initial manifestation of rheumatoid arthritis. Chest 2004; 126:993-995
(2) Rudwaleit M, Andermann B, Alten R, et al. Atopic disorders in ankylosing spondylitis and rheumatoid arthritis. Ann Rheum Dis 2002; 61:968-974
(3) Kero J, Gissler M, Hemminki E, et al. Could TH1 and TH2 diseases coexist? Evaluation of asthma incidence in children with coeliac disease, type 1 diabetes, or rheumatoid arthritis: a register study. J Allergy Clin Immunol 2001; 108:781-783
(4) Tauro B. Eosinophilic synovitis: a new entity? J Bone Joint Surg Br 1995; 77:654-656
(5) Atanes A, Fernandez V, Nunez R, et al. Idiopathic eosinophilic synovitis: case report and review of the literature. Scand J Rheumatol 1996; 25:183-185
(6) Inoue K, Takano H, Yanagisawa R, et al. Effect of 15-deoxy-delta 12,14-prostaglandin J2 on acute lung injury indueed by lipopolysaccharide in mice. Eur J Pharmacol 2003; 481:261-269
(7) Takano H, Yoshikawa T, Ichinose T, et al. Diesel exhaust particles enhance antigen-induced airway inflammation and cal cytokine expression in mice. Am J Respir Crit Care Med 1997; 156:36-42
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group