Mrs. Ludlow was an attractive woman in her mid-thirties, but she looked as if she could use a good night's sleep. Her nine-year-old daughter sat at her side. After introducing myself, I led them into my office and asked Mrs. Ludlow if she knew why she needed to see me. "Well, to tell you the truth, no," she said, sighing. "We're here because the Committee on Special Education at our elementary school said they need a report from you." * "Why is your daughter being evaluated?" * "Nicole's a bright kid, but she's missed so much school this year that she's failing third grade. They're trying to decide whether to give her home tutoring, put her in special ed, or make her repeat the year. So they want to find out why she has these attacks. But frankly, Nicole's already been seen by more than a dozen specialists. So far, no one's been able to tell me what's wrong with her."
"We Mrs. Ludlow spoke, her daughter sat stone still on a chair across from her, staring into space.
"Well, I'm a medical geneticist," I explained. "I take care of children with birth defects and inherited diseases. Is there any reason to think Nicole's condition is inherited?"
"Not that I know of."
"Well, if it's all right with you, I'll begin by asking some questions about Nicole's past; then I'll examine her. Then we'll talk about where we go from there. Okay?"
She nodded her head.
"Let's start at the beginning," I said. "How much did Nicole weigh at birth?" As the words were coming out of my mouth, the child began to make a strange mewing noise. It sounded like a cat stuck in a closet. The noise came from somewhere deep inside the girl's throat, not her vocal cords exactly but from somewhere farther down. After finishing my question, I gazed at Nicole, trying to figure out what she was trying to say.
"Quiet," the girl's mother said. "Don't make that noise. That's a bad noise."
Nicole, still staring off into space, immediately became quiet.
"She's usually a nice, sweet kid," said Mrs. Ludlow apologetically. "But she's having one of her attacks. The attacks are the problem."
I stared at the little girl, trying to get her attention. Although she looked fine, she behaved as if she were in a world of her own. Never did she make eye contact with me; not once did she even look my way.
"Has anyone suggested that Nicole might be autistic?" I asked.
"No. She's usually very outgoing. It's only during her attacks that she acts this way. Can autism come and go like this? "
I shook my head. To say this girl had grabbed my attention was an understatement. "How often does this happen?"
"A couple times a year. Actually, it's good you're seeing her today, so you can understand what I'm talking about. When she's her normal self and I try to explain what's wrong with her, people usually think I'm crazy."
"How long does this last?" I asked, though I wasn't sure what "this" actually referred to.
"Can't be sure," the mother replied. "Sometimes it's just a day or two. The longest has been nearly four weeks. And nothing seems to bring them on. They just seem to come and go."
"Are they seizures?" I asked.
"That's what the neurologists have always thought. Over the years, Nicole's been seen by five neurologists. She's been hospitalized three times for overnight brain-wave tests. She's had two CT scans, an MRI, and about a hundred blood tests. Every test has turned out perfectly fine. Every doctor has told me that he could find nothing wrong with my daughter. Some have even accused me of making the whole thing up. But look at her - you can verify I'm not making this up, can't you?"
I said yes, I'd certainly be willing to swear in a court of law that she hadn't invented Nicole's illness. "You seem to know a lot about medicine," I commented. "Do you have a medical background?"
"No," she replied. "But what I've gone through with this kid has been a medical education."
"Has anyone tried to treat these episodes with medication?"
"Sure," she responded without hesitation. "Every neurologist has started Nicole on some form of antiseizure medication. Just last week the doctor we saw put her on Tegretol. None has done a bit of good. Some, if you ask me, have actually made her worse."
"How old was Nicole when the episodes started?" I asked, still groping in the dark.
As Mrs. Ludlow told her daughter's story, the look of exhaustion lifted from her face. She explained that Nicole had been perfectly healthy until she was three and had surgery on an elbow she'd fractured in a fall. "But after the operation, she just never woke up from the anesthesia. It was terrifying - she went into a coma and nobody could bring her out of it. At first they thought she'd suffered brain damage. They did a CT scan, but it was normal. They gave her all kinds of medications, antibiotics, steroids, but Nicole just wouldn't wake up. I was sure she was going to die."
I thought for a minute, trying to understand the relationship between the anesthesia and the onset of the illness. In the back of my mind, a distant bell began to ring. The story was starting to remind me of something. "How long did she stay like that?"
"Two weeks. For two weeks I sat at her bedside, holding her hand, talking to her, trying to wake her up. The doctors kept telling me they couldn't find anything wrong. Then one day she just woke up. She opened her eyes, looked at me and said, `Hi, Mommy,' and that was it."
While her mother was talking, Nicole got up and walked over to my filing cabinet. She placed her face against the cabinet's metal front and stood there, as rigid as a statue. "Is she okay?"
Mrs. Ludlow shrugged. "I guess so. As all right as she ever gets during one of her attacks."
"So after that first episode, was she back to her old self."
"It was as if nothing had happened," she said, "except that the right side of her face drooped. The neurologist told me she had facial palsy and that she might have it for the rest of her life. Of course, he was wrong - the doctors have been wrong about everything about Nicole. The droopiness lasted about a week. But since then it's come back a few times, usually during or right after an attack."
On the pad on my desk, I wrote "Coma after anesthesia" and beneath it "Recurrent facial palsy." The bell inside my head was ringing louder now. "So how many of these attacks has Nicole had?"
Mrs. Ludlow paused and sighed. "Somewhere between 20 and 25."
"Other than the coma and the facial palsy," I continued, "what other problems have occurred during the episodes?"
"Let's see," Mrs. Ludlow said. "Sometimes her speech gets slurred, as if she's had a stroke." The bell in my head was ringing even louder now. I wrote the words "Slurring of speech" on the pad. "And insomnia," she added. "That's the worst part. Nicole can go four or five days in a row without sleeping. And of course I have to stay awake, too, because I'm afraid she might hurt herself."
I wrote "Insomnia" on the next line of the pad. Undoubtedly this was the cause of Mrs. Ludlow's haggard appearance. "Anything else?"
"Yes, she gets bad pains in her neck, her chest, and her belly. Once I thought she was having a heart attack. Another time the doctors in the emergency room wanted to take her appendix out."
As I wrote "Pain" on the pad, I thought I finally knew what was wrong with Nicole. I just needed one more bit of information to confirm my suspicion. "During these attacks, is there anything unusual about Nicole's urine?"
"You're the first person ever to ask, but there is something. When she's sick, Nicole's urine gets very dark. Does that mean anything?"
It sure did. By now the bells in my head were sounding an alarm. I was almost positive that Nicole had a disorder called acute intermittent porphyria, or AIP.
Much as I hate to admit it, my flash of diagnostic insight wasn't the result of my being smarter than the dozen other doctors who'd seen Nicole. I hadn't read more articles, I didn't have better clinical acumen, and I hadn't asked more-probing questions. The explanation for my medical epiphany was simple.
In the weeks prior to the Ludlows' visit, I was at work on a book about historical figures who were afflicted with genetic diseases. Just the month before, I'd finished a chapter on King George III, the English monarch at the time of the American Revolution. Throughout his reign, King George suffered a series of mysterious - and ultimately incapacitating - illnesses. Just like Nicole's, his attacks came and went without warning. His symptoms - nervous trembling, altered consciousness, intractable pain, and terrible insomnia - mystified doctors. In 1966 two British psychiatrists finally proposed a logical explanation for King George's ailment. Based on a study of the records kept by the king's personal physician, they suspected that King George had probably suffered from porphyria.
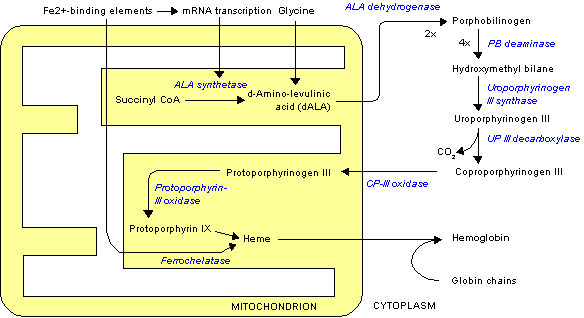
The porphyrias are a group of rare inherited disorders that affect the body's ability to make hemoglobin, the molecule that enables red blood cells to absorb and release oxygen. Heme is the iron-containing portion of hemoglobin, and patients with porphyria don't make one of the several enzymes needed to make normal amounts of it. As a result, many patients with porphyria have two symptoms in common. First, they are anemic because they cannot make enough heme. Second, because heme is not being assembled properly, the precursors of heme build up in the blood. The accumulation of these chemicals, which are toxic to the skin, the liver, and the nervous system, can cause an array of other puzzling symptoms.
The form of porphyria that affected George III, however, does not cause constant symptoms. Under normal circumstances, there is enough enzyme to maintain good health. But during illness or emotional stress, or following exposure to certain drugs or chemicals, patients can experience unexplained aches and bizarre neurological disturbances. And because of the buildup of heme precursors, they excrete abnormally dark urine.
Nicole's first attack had followed exposure to anesthetic agents, some of which are known to exacerbate symptoms. In the following years, she had been treated with the anticonvulsant phenobarbital, which also makes symptoms worse. In fact, the attack that was at that moment gripping Nicole may well have been brought on by treatment with the anticonvulsant drug she'd begun to take the week before.
The more I thought about it, the more convinced I became that Nicole had AIP. Although the condition rarely causes symptoms in young children, the resemblance between her symptoms and King George's was too striking for mere coincidence. To prove the diagnosis, though, I had to complete two tasks. First, since AIP is inherited when a gene is passed from an affected parent to a child, I had to find out which of Nicole's parents also suffered from the disease. And second, I had to prove that Nicole's blood bore evidence of the biochemical abnormality that causes An. I turned my attention to the first of these tasks.
I told Mrs. Ludlow that Nicole's dark urine might be significant and continued with my questioning. "How was your pregnancy with Nicole?"
"Awful," Mrs. Ludlow replied. "I was hospitalized twice. The first time, I was in my sixth week. I began having terrible belly pain. My doctor operated to see what was going on."
"Did he find anything wrong?
"No, that's the strange part: everything was fine. Then about a week later, the pain just went away. Weird."
I was ready to burst. Mrs. Ludlow's unexplained pain was most likely an attack of porphyria. I kept probing. "When was the second hospitalization?"
"A month later. It was terrible. I was vomiting so much I was hospitalized for six weeks for dehydration."
Again, these symptoms were consistent with porphyria. The stress of pregnancy could have triggered the attacks. "Have you ever had any episodes like Nicole's?" I asked. Mrs. Ludlow shook her head.
When I asked about the rest of the family, Mrs. Ludlow said that her husband and his family were in excellent health, but members of her side of the family had had a series of unexplained health problems. "My mother's okay," she said, "but my father's a mess. People think he's a drunk because he has blackouts, but I know he never takes a drink - it makes him sick to his stomach. And then, his older sister has had seizures all her life. . . "
Anything besides seizures?" I asked.
She shook her head. "That sister has a daughter who's okay. . ."
"That would be-your first cousin?"
"Yes, she's okay, but her daughter has some rare disease. I don't know what it's called."
"Porphyria?" I asked, nearly jumping out of my skin.
Mrs. Ludlow's eyes opened wide. "Yes, that's it. How did you know?"
"Mrs. Ludlow, I've been thinking for the past few minutes that porphyria would explain all of Nicole's problems. Since it's an inherited condition, I've been waiting for you to tell me that someone else in your family has it."
She seemed mystified. "But how can my cousin and I both have daughters with it if nobody else in the family has it?" she asked dubiously.
"Well, Nicole and your cousin's daughter aren't the only ones who have it. I'm pretty sure those problems you had during your pregnancy were episodes of porphyria. And your father's blackouts and his inability to tolerate alcohol? Those are probably also caused by porphyria."
"What about my cousin? " Mrs. Ludlow asked. "She's never been sick. . ."
"That's what's strange about this disease," I interrupted. "It varies widely from one person to the next. Some people are sick all the time, others never have a sick day in their lives. I can't explain it better than that."
Mrs. Ludlow considered this. "If she really does have porphyria, and I'm not sure she does, what can we do?"
"Well, we can't cure it, but we can do a lot to help her." I explained that putting Nicole on a high-carbohydrate diet and keeping her off certain medications could prevent the attacks. The first step would be to take Nicole off Tegretol. I also explained that I needed samples of blood and urine from Nicole to confirm the diagnosis. I then asked if Mrs. Ludlow had any more questions.
Just one," she said. "How were you able to make this diagnosis when so many other doctors didn't think of it?"
I just shrugged. What I should have told her was that we doctors are just like everyone else. We go to the movies, watch Tv, read newspapers and novels. If we happen to see a patient who has symptoms of a rare disease that was featured on the previous night's "Movie of the Week," we're more likely to consider that condition when making a diagnosis.
Blood tests ultimately confirmed my diagnosis of acute intermittent porphyria in Nicole Ludlow and her mother. But I didn't make the diagnosis because I'm a brilliant diagnostician or because I'm a sensitive listener. Had I seen Nicole one year before, I'm sure I would have failed. No, I succeeded where others failed simply because the Ludlows and I managed to run into each other in exactly the right place, at exactly the right time.
COPYRIGHT 1995 Discover
COPYRIGHT 2004 Gale Group