SUMMARY
Portal vein aneurysm is a rare medical entity that can be caused by chronic hepatic diseases with portal hypertension. We describe a 45-year-old man with variceal bleeding from hepatosplenic schistosomiasis and an incidentally found intrahepatic aneurysm. Diagnosis was confirmed with non-invasive imaging exams, arteriography and liver biopsy. Following splenectomy, the aneurysm diameter decreased substantially.
KEYWORDS: Aneurysm, Portal hypertension; Portal vein; Schistosomiasis; Splenectomy
INTRODUCTION
Portal vein aneurysm is a rare finding. We reviewed the scientific literature indexed in MEDLINE and LILACS (Latin American and Caribbean literature on Health Sciences) and recorded all descriptions of portal vein aneurysms, which correspond to 53 medical articles since 1965, referring to almost 70 cases up to the present, including English and non-English articles1,4,7,814.15,17,19,21,23-26,29,30
Portal aneurysms can be caused by portal hypertension, but have never before been related to hepatosplenic schistosomiasis. We report the finding of an intrahepatic portal vein aneurysm in a patient with hepatosplenic schistosomiasis with a marked reduction in its dimensions after splenectomy.
CASE DESCRIPTION
A 45-year-old black male was admitted with a dull ache in the left hypochondrium, which was continuous and resistant to common analgesics. He had an episode of upper digestive hemorrhage six months before, manifested as hematemesis and enterorrhagia, and received three units of packed red blood cells. The endoscopic examination at that time disclosed four medium-caliber esophageal varices with red spots. Sclerotherapy was then performed and continued at monthly intervals.
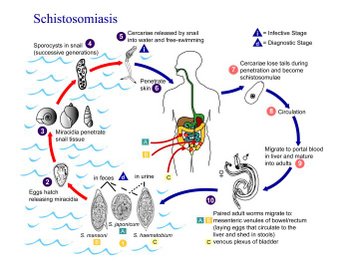
The patient had lived up to 17 years of age in an endemic area of schistosomiasis. He denied use of alcoholic beverages, as well as previous treatment with anti-parasitics. Physical examination showed good general health. The liver was of normal size and was palpable 2 cm below the xiphoid process, having a firm consistency with blunt edges. The spleen extended below the umbilicus, and its palpation elicited pain with the same characteristics as reported before by the patient.
Blood exams at admission were as follows: Hct 39.4 (40-52%), Hb 13.4 (13-18 g/dL) WBC count 3,300 (5-10,000 cells/mm^sup 3^), platelet count 101,000 (140-450,000 cells/mm^sup 3^), gamma globulins 1.7 (0.7-1.6 mg / dL), albumin 4.3 (3.5-5.0 g /dL), AST 23 (0-18 U/L), ALT 46 (0-18 U/ L), GGT 44 (4-28 U/L), alkaline phosphatase 89 (60-170 U/L), INR 1.52 and prothrombin time 13.6 (control 11.2 s). Parasitological fecal exams, including the Kato-Katz technique, were performed six times and were always negative for eggs of Schistosoma mansoni, and so was a rectal biopsy. Anti-HBc IgG, HBsAg, anti-HCV, anti-nuclear, anti-- smooth muscle and anti-LKM antibodies were negative. Serum levels of alpha-1-antitrypsin, ceruloplasmin, ferritin and transferrin saturation were normal.
The abdominal ultrasound showed a liver with blunt edges and an enlarged left lobe. There was intense wall thickening of the portal venous system up to the tertiary ramifications (Fig. 1), and splenomegaly with abundant collateral circulation in the splenic hilus. Surprisingly, an anechoic circular structure was found at the right hepatic lobe, with a thick surrounding wall. Doppler ultrasound showed biphasic waveform flow. An abdominal helicoidal computerized tomography (CT) was performed. In addition to the ultrasonographic findings, arching and distortion of the hepatic veins were noticed, and the aforementioned lesion was defined as a hypodense image in continuity with the right branch of the portal vein, which assimilated the intravenous contrast in the portal phase of the exam (Fig. 2). Magnetic resonance imaging of the abdomen confirmed that it was an aneurysmatic dilatation of the right portal branch measuring 5 x 4 x 4 cm.
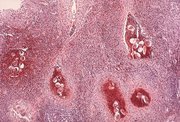
A splenectomy was indicated for the treatment of pain and portal hypertension. Preoperative arteriography revealed the aneurysm (Fig. 3) and found an elevated hepatic venous pressure gradient of 7.5 mmHg. During surgery, the main findings were gross irregularity of the liver with an enlarged left lobe and splenomegaly up to 8 cm beyond the lower left costal arch. The portal vein pressure was 15 mmHg as measured by doppler ultrasound and there were no signs of thrombosis. A wedged hepatic biopsy was also performed and the main anatomopathological results were as follows: the spleen featured sclerosis, congestion and Gamma-Gandy bodies and the liver showed non-confluent portal fibrosis, destruction of portal vein branches with smooth muscle cell disruption, sparing of ductal and arterial elements, and vascular ectatic proliferation (angiomatoid formations).
The patient was followed-up for four years after surgery. There was remission of the abdominal pain and normalization of prothrombin time and of leukocyte and platelet counts. The only complication detected was partial portal vein thrombosis, which was asymptomatic. Ultrasonographic exams demonstrated disappearance of thrombosis and progressive reduction of the aneurysm size, reaching 1.4 cm in diameter two years after surgery and stabilizing until the fourth year of follow-up.
DISCUSSION
The described patient had a chronic liver disease with portal hypertension. There were findings consistent with the diagnosis of hepatosplenic schistosomiasis, including the patient's origin from an endemic area, the ultrasonographic findings of intense wall thickening of the portal venous system up to the tertiary ramifications (the counterpart of Symmers' or pipestem fibrosis) and an increased left liver lobe contrasting to a reduced right lobe9,12 . The definitive diagnosis was made by a liver biopsy, considering the typical findings of portal fibrous enlargement, preservation of the lobular architecture and angiomatoid formations; furthermore, the presence of isolated muscle cells or fibers caused by the destruction of portal vein branches is specific for hepatosplenic schistosomiasis2,3,11 The absence of egg granulomas does not exclude the diagnosis, given the low sensitivity of this microscopic finding. This is justified by the fact that, after triggering the fibrosis, the eggs eventually become reabsorbed, either with medical treatment, or when there is a spontaneous cure of the infection. The same process can eliminate schistosomotic pigments, aborting the reactivity of immunohistochemical antigen tests2,3,11. In the case described herein, there had probably been a spontaneous resolution of the infection, because the patient had been away from the endemic area for 28 years.
Angiographic features of hepatosplenic schistosomiasis characteristically include distortion of large arterial and hepatic vein branches and the Bogliolo sign, which is the formation of an intense network of small-caliber vessels27, but these findings require portal and hepatic injection of contrast, which was not done in this case. However, vessel arching was well demonstrated by the helicoidal CT.
When considering the differential diagnosis, one would have to take into account the possibility of hepatoportal sclerosis (or idiopathic portal hypertension), which has already been related to portal vein aneurySMS14,23. In that condition there is also the formation of incomplete fibrous septa, but it can be distinguished by the characteristic microscopic finding of portal vein sclerosis, and muscle cell disruption is not one of its features6. It has also rarely been reported in Brazil22. In contrast, hepatosplenic schistosomiasis can be found in 3.2 to 7.5% of people in some hyperendemic rural communities, as demonstrated by LAMBERTUCCI et al. using a combination of positive stool exams and ultrasonographic findings.20.
An elevated hepatic venous pressure gradient was found in this case, which means that there was sinusoidal hypertension. Although hepatosplenic schistosomiasis is a classical example of presinusoidal portal hypertension, a sinusoidal mixed pattern can be found in 30% to 59% of these patients5.
Portal vein aneurysms have been considered a rare medical condition since they were first described about four decades ago. OHNISHI et al.26 have encountered only two of them out of 3,000 patients with portal hypertension on whom ultrasonography was performed26. Nevertheless, these reports have been increasingly more common in recent years, totaling now almost 70 cases, including intra- and extrahepatic locations, which is probably due to the greater availability of noninvasive abdominal imaging studies, suggesting that this will not be considered such a rare disease in the near future 1,4,7,8,14,15,17,19,21,23-26.
Portal aneurysms are most commonly found in the main portal vein branches or next to the junction of the mesenteric with the splenic vein as regards intra- and extrahepatic aneurysms, respectively. By far, the two most common causes are congenital malformations and chronic hepatic diseases. They can also be related to acquired abnormal weaknesses of the vein wall, such as those caused by abdominal trauma, acute pancreatitis, hepatic tumors, and arterioportal fistulas. Their natural history varies from incidental findings in asymptomatic patients to serious complications such as thrombosis, portal hypertension with bleeding from esophageal varices, compression of adjacent structures or rupture into the abdominal cavity, including a few fatalities. There are no reports of spontaneous regression in untreated patients. Treatment has consisted mainly of portosystemic shunts and/or aneurysm excision1,4,7,8,14,15,17,19,21,23-26.
The surgical treatment of portal hypertension in hepatosplenic schistosomiasis is still a matter of debate. The best results have been achieved with distal splenorenal shunting and with esophagogastric devascularization plus splenectomy28. In our hospital, the latter is the procedure of choice, but the patient was included in a study protocol comparing this procedure with isolated splenectomy for the treatment of portal hypertension related to schistosomiasis. Therefore, he did not undergo esophagogastric devascularization.
Portal vein thrombosis is a well-known complication of surgical interventions carried out to reduce portal venous pressure, such as splenectomy and distal splenorenal shunting. Reports of their clinical significance vary from a predominantly asymptomatic and benign course to a severe and sometimes fatal evolution. The thrombosis seems to be much more common after splenectomy in hepatosplenic schistosomiasis (13%) and idiopathic portal hypertension (25%) than in cirrhosis (1.8%), possibly because in the former two conditions there is a greater fall in portal vein pressure after surgery10,13,16,18.
Considering the present case, the regression of the aneurysm dimensions after splenectomy indicates that the excessive venous inflow from the splenic vein was contributing significantly to the portal hypertension, and therefore also to venous dilatation. Partial vein thrombosis may also have contributed to the significant reduction of the aneurysm size, although its dimensions did not increase after complete recanalization of the portal vein. According to our review of the literature, ours was the first description of a portal vein aneurysm related to hepatosplenic schistosomiasis, as well as that of a portal aneurysm's regression after splenectomy.
RESUMO
Tatamento por esplenectomia de um aneurisma de veia porta na esquistossomose hepato-esplenica
Aneurismas venosos portais sao uma entidade medica rara, ao passo que as esquistossomoses ainda constituem uma pandemia. Descrevemos um paciente de 46 anos, com esquistossomose hepato-esplenica e um aneurisma intra-hepatico confirmado por varios metodos de imagem. Apos a esplenectomia, o diametro do aneurisma dininuiu significativamente.
REFERENCES
1. ALTUNTAS, B.; ERDEN, A.; KARAKURT, C. et al. - Severe portal hypertension due to congenital hepatoportal arteriovenous fistula associated with intrahepatic portal vein aneurysm. J. clin. Ultrasound, 26: 357-360, 1998.
2. ANDRADE, Z.A.; PEIXOTO, E.; GUERRET, S. & GRIMAUD, J.A. - Hepatic connective tissue changes in HS. Hum, Path., 23: 566-573, 1992.
3. ANDRADE, Z.A. & PEIXOTO, E. - Pathology of periportal fibrosis involution in human schistosomiasis. Rev. Inst. Med. trop. S. Paulo, 34: 263-272, 1992.
4. ATASOY, K.C.; FITOZ, S.; AKYAR, G.; AKYAR, S. & ERDEN, 1. - Aneurysms of the portal venous system: gray scale and color doppler ultrasonographic findings with CT and MRI correlation. Clin. Imaging, 22: 414-417, 1998.
5. COUTINHO, A. - Hemodynamic studies of portal hypertension in schistosomiasis. Amer. J. Med., 44: 547-556, 1968.
6. BIOULAC-SAGE, P.; BAIL, B.L.; BERNARD, PH. & PALABAUD, C. - Hepatoportal sclerosis. Semin. Liver Dis., 15: 329-339, 1995.
7. BOYEZ, M.; FOURCADE, Y.; SEBAG, A. &VALETTE, M. - Aneurysmal dilatation of the portal vein: a case diagnosed by real-time ultrasonography. Gastroint. Radio!., 11: 319-321, 1986.
8. BROCK, PA.; JORDAN Jr., P.R.; BARTH, M.H. & ROSE, A.G. - Portal vein aneurysm: a rare but important vascular condition. Surgery, 121: 105-108, 1997.
9. CERRI, G.G. - A ultra-sonografia no diagnostico da forma hepato-esplenica da esquistossomose mansonica. Rev. Imagem, 6: 119-134, 1984.
10. CHAIB, E.; PUGLIESI, V.; CAPACCI, M.L. et al. - Trombose portal: complicacao precoce da desconexao ;zigo-portal no tratamento das varizes esofagianas sangrantes. Rev. Hosp. Clin. Fac. Med. S. Paulo, 45: 205-209,1990.
11. CHAPADEIRO, E. & PITANGA, L.C. - Sobre a reversao da fibrose hepAtica esquistossomotica apos terapeutica especifica. Estudo histologico. Rev. Soc. bras. Med. trop., 30: 53-56, 1997.
12. DOMINGUES, A.L; LIMA, A.R.; DIAS, A.S.; LEAO, G.C. & COUTINHO, A. - An ultrasonographic study of liver fibrosis in patients infected with Schistosoma mansoni in northeast Brazil. Trans. roy. Soc. trop. Med. Hyg., 87: 555-558, 1993.
13. EGUCHI, A.; HASHIZUME, M.; KITANO, S. et al. - High rate of portal thrombosis after splenectomy in patients with esophageal varices and idiopathic portal hypertension. Arch. Surg., 126: 752-755, 1991.
14. FUKUSHIMA, N.; DOHMEN, K.; YAMANO, Y. et al. - Idiopathic portal hypertension associated with intrahepatic portal aneurysm and splenic artery aneurysm: a case report. Jap. J. Gastroent., 88: 1130-1135, 1991.
15. GALLAGHER, D.M.; LEIMAN, S. & HUX, C.H. - In utero diagnosis of a portal vein aneurysm. J. clin. Ultrasound, 21: 147-151, 1993.
16. HENDERSON, J.M.; MILLIKAN Jr., W.J.; CHIPPONI, J. et al. - The incidence and natural history of thrombus in the portal vein following distal splenorenal shunt. Ann. Surg., 196: 1-7,1982.
17. HERMANN, R.E. & SHAFER, W.H. - Aneurysm of the portal vein and portal hypertension: first reported case. Ann. Surg., 162: 1101-1104, 1965.
19. JIN, G. & RIKKERS, L.F. - The significance of portal vein thrombosis after distal splenorenal shunt. Arch. Surg., 126:1011-1016,1991.
19. KIM, E.E.; ROMERO, J. & KIM, C.G. - Portal venous aneurysm demonstrated by magnetic resonance imaging. Clin. Imaging, 22: 360-363, 1998.
20. LAMBERTUCCI, J. R.; COTA, G.F; PINTO-SILVA, R.A. et al. - Hepatosplenic schistosomiasis in field-based studies: a combined clinical and sonographic definition. Mem. Inst Oswaldo Cruz, 96 (suppl): 147-150, 2001.
21. LEE, H.C.; YANG, YC.; SHIH, S.L. & CHIANG, H.J. - Aneurysmal dilatation of the portal vein. J. pediat. Gastroent. Nutr., 8: 387-389, 1989.
22. MAKSOUD, J.G.; MIES, S. & GAYOTTO, L.C.C. - Hepatoportal sclerosis in childhood. Amer. J. Surg., 151: 484-488, 1986.
23. MALDE, H.M. & CHADHA, D. - Extrahepatic portal vein aneurysm in non-cirrhotic portal fibrosis. Aust. Radiol., 37: 221-222, 1993.
24. MIYAZAKI, T.; YAMASHITA, Y.; TOMODA, K. et al. - Transarterial embolization of an extrahepatic portal vein aneurysm with arterioportal fistula. Cardiovasc. intervent Radiol., 18: 189-191, 1995.
25. OHNAMI, Y; ISHIDA, H.; KONNO, K. et al. - Portal vein aneurysm: report of six cases and review of the literature. Abdom. Imaging, 22: 281-286, 1997.
26. OHNISHI, K.; NAKAYAMA, T.; SAITO, M. et al. - Aneurysm of the intrahepatic branch of the portal vein. Report of two cases. Gastroenterology, 86: 169-173, 1984.
27. RAIA, S.; MIES, S. & MACEDO, A.L. - Surgical treatment of portal hypertension in schistosomiasis. Wid. J. Surg., 8: 738-752, 1984.
28. RAIA, S.; SILVA, L.C.; GAYOTTO, L.C.C. et al. - Portal hypertension in schistosomiasis: a long-term follow-up of a randomized trial comparing three types of surgery. Hepatology, 20: 398-403, 1994.
29. THOMAS, T.V. - Aneurysm of the portal vein: report of two cases, one resulting in thrombosis and spontaneous rupture. Surgery, 61: 550-555, 1967.
30. VINE, H.S.; SEQUEIRA, J.C.; WIDRICH, W.C. & SACKS, B.A. - Portal vein aneurysm. Amer. J. Roentgenol., 132: 557-560, 1979.
Received: 10 April 2002
Accepted: 25 July 2002
Marcos MUCENIC(1), Manuel de Souza ROCHA(2), Antonio Atilio LAUDANNA(1) & Eduardo Luiz Rachid CANCADO(1,3)
(1) Department of Gastroenterology, University of Sao Paulo School of Medicine, Sao Paulo, SP, Brasil.
(2) Department of Radiology, University of Sao Paulo School of Medicine, Sao Paulo, SP, Brasil.
(3) Laboratory of Medical Investigation/Immunopathology of Schistosomiasis, Institute of Tropical Medicine, University of Sao Paulo School of Medicine, Sao Paulo, SP, Brasil.
Correspondence to: Marcos Mucenic, Natingui 452, 05443-000 Sao Paulo, Brasil. Telephone number 00-55-I 1-94058085, fax number 00-55-11-94058085, fax number 00-55-11-30645132, e-mail: mmucenic@terra.com.br
Copyright Instituto de Medicina Tropical de Sao Paulo Sep/Oct 2002
Provided by ProQuest Information and Learning Company. All rights Reserved