Interconnected brain areas that use split-second timing to interpret new information suffer a communication breakdown in people with schizophrenia, a new study suggests.
The finding hinges on measurements of some brain waves that arise from synchronized activity in large clusters of neurons.
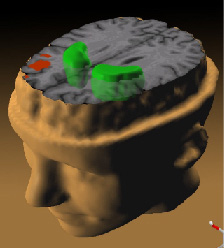
In healthy adults listening to two different tones in a sequence, for example, these aligned brain waves occur about one-tenth of a second after a person first recognizes the tones' difference, say neuroscientist Leanne M. Williams of Westmead (Australia) Hospital and her colleagues. The synchronized electrical outbursts appear most prominently in the frontal brain, a region regarded as a key part of a network that interprets novel perceptions against a background of prior knowledge.
In contrast, people diagnosed with their first bout of schizophrenia display a decline in neural synchrony, especially in the frontal brain, in the fraction of a second after discerning a particular tone, Williams' team reports in the March American Journal of Psychiatry. Individuals with schizophrenia exhibit unusually low levels of synchronized neural firing to begin with, the researchers note.
If confirmed in further work, these findings raise the likelihood that "a breakdown in the synchrony of distributed neural networks is a marker for the onset of schizophrenia," the researchers conclude.
For their study, the scientists enrolled 40 people receiving outpatient treatment for an initial episode of schizophrenia--a condition often marked by hallucinations, delusions, incoherence, and apathy--and 40 individuals with no psychiatric condition. All participants were either teenagers or young adults. In the schizophrenia group, 36 volunteers had been taking a prescribed antipsychotic medication for around 10 months. The other 4 volunteers had received no such drug.
Scalp electrodes recorded gamma waves, which arise when thousands of neurons emit matching electrical signals around 40 times a second. Other scientists have linked gamma activity to basic types of learning and perception (SN: 2/20/99, p.122). Brain wave measurements were taken as participants tried to ignore low-frequency tones played repeatedly through headphones. The volunteers were instructed to press a button as fast as possible whenever they heard high-frequency tones that the researchers also played into the headphones.
As in previous studies, schizophrenia patients took substantially longer to respond to high-frequency tones than their healthy peers did. Moreover, their gamma-wave readings reflected a lack of synchrony.
Williams and her colleagues suspect that their new finding reflects the disease process rather than the effects of antipsychotic medication. To make sure, they plan to study brain wave responses of additional medication-free individuals in the early stages of schizophrenia.
The new data "suggest a disintegration of fast [neural] signaling in early perceptual processing" in schizophrenia, writes neuroscientist Karl Friston of University College London in comments published with the new report. Out-of-sync neurons can disrupt different parts of brain networks that orchestrate perceptual or emotional learning, perhaps contributing to schizophrenia's variety of symptoms, Friston proposes.
Psychiatrist Daniel R. Weinberger of the National Institute of Mental Health in Bethesda, Md., takes a cautious approach to the new study. Disorganized activity in critical brain networks may foster schizophrenia, he says, but it's not clear what causes disrupted gamma-wave activity or how a loss of neural synchrony reverberates through the brain.
COPYRIGHT 2005 Science Service, Inc.
COPYRIGHT 2005 Gale Group