As NPs continue to play an important role in health care as administers of prescriptions, the value of reviewing the latest Food and Drug Administration (FDA) approvals for new drugs and devices is immeasurable. In 2002, the FDA approved several new drugs and devices, as well as monitored previously approved drugs for adverse reactions and untoward events. This article provides a brief review of relevant primary care topics.
* Drugs to Treat Heroin and Opiate Addiction
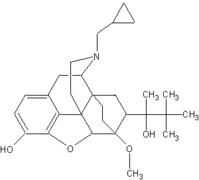
In early October 2002, the FDA announced the approval of Subutex (buprenorphine hydrochloride) and Suboxone tablets (buprenorphine hydrochloride and naloxone hydrochloride) for the treatment of opiate dependence. Subutex contains only buprenorphine hydrochloride and was developed as the original product. The second medication, Suboxone, contains another ingredient, naloxone, an opiate antagonist, to guard against misuse. Subutex is administered during the first few days of treatment, while Suboxone is used during the maintenance phase of treatment.
Presently, opiate dependence treatments such as methadone can only be dispensed in clinics that specialize in addiction treatment. However, there aren't adequate numbers of treatment centers to help all patients seeking treatment.1 Under the Drug Abuse Treatment Act (DATA) of 2000, Subutex and Suboxone are the first narcotic drugs available for the treatment of opiate dependence that can be prescribed in an office setting by specially-trained health care providers, allowing treatment access to more patients.
In a double-blind placebo and active controlled study, 326 heroin-addicted subjects were randomly assigned to either Suboxone 16 mg per day, 16 mg Subutex per day, or placebo tablets.2 Subjects were instructed to hold the medication under the tongue for approximately 5-10 minutes, or until completely dissolved. Subjects received I hour of individual counseling per week and a single session of HIV education.
The primary study comparison was to assess the efficacy of Subutex and Suboxone individually against placebo. The percentage of thrice-weekly urine samples that tested negative for nonstudy opioids was statistically higher for both Subutex and Suboxone, than for placebo.
The most common reported side effects of Subutex and Suboxone include cold or flu-like symptoms, headaches, sweating, sleeping difficulties, nausea and mood swings.2 Similar to other opioids, Subutex and Suboxone have been associated with respiratory distress, especially when combined with other depressants.
Suboxone and Subutex are controlled as Schedule III narcotics. Buprenorphine is a partial agonist at the mu-opioid receptor and chronic administration produces dependence of the opioid type, characterized by moderate withdrawal upon abrupt discontinuation or rapid taper. The withdrawal symptoms are milder than full agonists, and may be delayed at onset.
Neonatal withdrawal has been reported in infants born to mothers treated with Subutex during pregnancy. Suboxone contains naloxone and, if misused parenterally, is highly likely to produce marked and intense withdrawal symptoms.
Subutex and Suboxone are administered sublingually as a single, daily dose in the range of 12 to 16 mg/day. When taken sublingually, Suboxone and Subutex have similar clinical effects and are interchangeable. Subutex contains no naloxone and is preferred for use during induction. Following induction, Suboxone, due to the presence of naloxone, is preferred when clinical use includes unsupervised administration. The recommended maintenance target dose of Suboxone is 16 mg/day. The dosage should be adjusted in progressive increments/decrements of 2-4 mg to a level that holds the patient in treatment and suppresses opioid withdrawal effects.
Health care providers must meet the following Drug Enforcement Administration (DEA) requirements to qualify for prescription privileges for Subutex and Suboxone: 1) Have the necessary unique DEA identification number to prescribe these specific drugs; 2) Complete no less than 8 hours of authorized training on the treatment or management of opioid-dependent patients. This training may include classroom situations, seminars at professional society meetings, or other media. The Web site www.suboxone.com provides further details about scheduled training sessions; 3) Notify the Substance Abuse and Mental Health Services Administration (SAMHSA) of the intent to treat patients with these products. Notification is handled within SAMHSA by the Center for Substance Abuse Treatment (CSAT).
As a convenience, CSAT has developed a form that may be used for notification. The notification form may be completed online or downloaded at CSAT's Web site, www.dpt.samhsa.gov. CSAT will communicate with the DEA, review the notification and then notify DEA that the provider is qualified as required by DATA. This review process takes approximately 45 days. Additionally, the following criteria must be met: 1) Have the capacity to provide or refer patients for necessary ancillary services, such as psychosocial therapy; and 2) Agree to treat no more than 30 patients at any one time in the practice.
* Migraine Relief
Frovatriptan succinate (Frova, Elan Corp.) is the sixth triptan to be marketed for treatment of migraine headaches. All of the triptans are indicated for the acute treatment of migraine with or without aura in adults. There are relatively few studies that directly compare the triptans, but the first five agents (almotriptan (Axert), naratriptan (Amerge), rizatriptan (Maxalt), sumatriptan (Imitrex), and zolmitriptan (Zomig)) have generally been considered similar in efficacy.
The 2-hour headache response rates reported with frovatriptan (range 37% to 46% in clinical trials) suggest that it is less effective than its predecessors. The mean terminal elimination half-life of frovatriptan is 26 hours, the longest of all the triptans. Like naratriptan, it has a slow onset of action, however, the longer duration of action reduces the need to administer additional doses. Also, in patients who found migraine pain relief using frovatriptan, the drug may be more effective in preventing headache recurrence because of its long duration of action.
Most patients in clinical trials tolerated frovatriptan well. The adverse events experienced most often, and at an incidence higher than with placebo, include dizziness (8%), fatigue (5%), headache (4%), paresthesia (4%), hot or cold sensation (3%), dry mouth (3%) and chest pain (2%).
Serious adverse events experienced by a small number of patients following triptan use include peripheral vascular ischemia and colonic ischemia with abdominal pain and bloody diarrhea. There have been rare reports of sometimes fatal cerebrovascular events such as stroke, cerebral hemorrhage and subarachnoid hemorrhage attributed to the use of triptans.
As with naratriptan, and sumatriptan, frovatriptan is contraindicated in patients with ischemic heart disease, cerebrovascular disease or peripheral vascular disease.
The concurrent use of rizatriptan, sumatriptan, or zolmitriptan with an MAO type A inhibitor, or within 2 weeks of discontinuation of MAO inhibitor therapy is contraindicated. However, although concomitant use is best avoided, frovatriptan, almotriptan or naratriptan could be used with caution in patients treated with an MAO-type A inhibitor. The pharmacokinetic profile of a single dose of frovatriptan was not affected when it was administered to individuals receiving moclobemide (an MAO inhibitor not available in the United States).
Frovatriptan and the other triptans are classified in Pregnancy Category C and should be used during pregnancy only if the anticipated benefit justifies the risk to the fetus. It is not known if frovatriptan is secreted in human milk, and caution should be exercised if it is administered to a nursing woman. The effectiveness and safety of the triptans in pediatric patients have not been established.
The recommended dosage of frovatriptan is 2.5 mg with fluids. If the headache recurs after initial relief, another dose of 2.5 mg may be administered at least 2 hours after the first dose. The total daily dosage should not exceed 7.5 mg, with doses administered at intervals of at least 2 hours. It has not been established whether a second dose of frovatriptan would be effective in patients who do not respond to the first dose.
* Atopic Dermatitis Treatment
Atopic dermatitis (eczema) is a chronic inflammatory disease that often begins in childhood and is associated with the occurrence of skin lesions characterized by scaling, pruritus and inflammation. Treatment typically includes using emollients and topical corticosteroids, however some patients do not respond adequately to these therapies, or experience adverse events such as skin atrophy or striae with the use of a corticosteroid.
Pimecrolimus (Elidel-Novartis) is an ascomycin derivative with properties similar to tacrolimus, an agent originally marketed (Program to prevent the rejection of organ transplants and subsequently approved (Protopic)for topical use in the treatment of atopic dermatitis. The medication is thought to act by inhibiting production of inflammatory cytokines and mediators from mast cells.
Pimecrolimus is indicated for topical short-term and intermittent long-term therapy in the treatment of mild to moderate atopic dermatitis in nonimmunocompromised patients 2 years of age and older in whom the use of alternative, conventional therapies is deemed inadvisable. It is also indicated for treatment of patients who are not adequately responsive to or intolerant of alternative conventional therapies.
Pimecrolimus is also being evaluated for the topical treatment of psoriasis and other dermatological disorders, as well as for oral use.
In clinical studies, most patients experienced at least one adverse event, however the incidence of many of these reactions in the vehicle-controlled studies was similar to or less than the incidence in individuals treated with only the vehicle. Application site reactions and cutaneous infections were among the most common adverse events. In short-term studies (6 weeks) of pediatric patients (2-17 years), application site burning was reported in 10% of patients, and in a generally-similar percentage of those treated with the vehicle alone. Headache was experienced by 14% of patients. Application site symptoms are most common during the first few days of treatment, are usually mild to moderate in severity, usually last no more than 5 days, and typically improve as the lesions of atomic dermatitis resolve. If the reaction is severe or persists for more than a week, the patient should contact the prescriber.
Pimecrolimus is classified in Pregnancy Category C and should not be used during pregnancy unless it is clearly needed. It is not known whether it is excreted in human milk and a decision should be made whether to discontinue nursing or not use the drug.
In the 1-year safety study of pediatric patients, adverse events with pimecrolimus reported at a significantly higher incidence than the vehicle included headache (25%), cough (16%), pyrexia (13%), nasopharyngitis (26%), influenza (13%), pharyngitis (8%) and viral infection (7%).
In a study of pediatric patients aged 3-23 months, there was a higher incidence of respiratory symptoms/infections compared with the experience of older children. Although a casual relationship was not established, the use of pimecrolimus in children under 2 years of age is not recommended.
Following topical application, blood concentrations of pimecrolimus are very low. The new agent may be less likely than topically-applied tacrolimus or corticosteroids to cause systemic immunosuppression. The use of pimecrolimus in patients with Netherton's syndrome is not recommended because of the potential for increased systemic absorption.
Patients with atopic dermatitis are predisposed to superficial skin infections, which should be appropriately managed before treatment with pimecrolimus is initiated. Treatment may be associated with increased risk of varicella zoster virus infection (chicken pox or shingles), herpes simplex virus or eczema herpeticum. Pimecrolimus should not be applied to areas of active cutaneous viral infections. Skin papillomas or warts were observed in 1% of patients treated with pimecrolimus. If skin papillomas worsen or do not respond to conventional therapy, consider discontinuing treatment until complete resolution of the warts is achieved.
Pimecrolimus cream contains the drug in a 1% concentration. A thin layer of the cream should be rubbed into the affected skin gently and completely twice a day. The cream may be applied to all skin surfaces including head, neck and intertriginous areas. The drug should be used for as long as symptoms persist; however, if symptoms persist longer than 6 weeks, the patient should be reevaluated.
The safety of using pimecrolimus under occlusion has not been studied and it is recommended that it not be used with occlusive dressings.
* Anti-inflammatory Agent
Valdecoxib (Bextra)is the third selective cyclooxygenase-2 (COX-2) inhibitor and is indicated for the relief of symptoms of osteoarthritis and adult rheumatoid arthritis, as well as the treatment of primary dysmenorrhea.
In 1999, celecoxib (Celebrex) and rofecoxib (Vioxx) were marketed as the first selective COX-2 inhibitors. Although comparisons with older NSAIDs have not yet provided definitive conclusions, the selective COX-2 inhibitors appear to be just as effective, and associated with a lower risk of serious GI adverse events.
The contraindications, precautions and adverse events associated with the use of valdecoxib are generally similar to those of other nonsteroidal antiinflammatory drugs (NSAIDs). All NSAIDs are contraindicated in patients who have experienced asthma, urticaria or allergic-type reactions after taking aspirin or another NSAID, because of the potential for severe, and even fatal, anaphylactic-type reactions. Such experiences are most likely to occur in patients with asthma, however, exercise caution with all patients because fatal reactions have resulted when an NSAID was taken by a patient with a history of hypersensitivity to aspirin that was either unknown or overlooked by the NSAID prescriber.
As with other NSAIDs, GI effects are the adverse events most often associated with the use of valdecoxib (dyspepsia [8%], nausea [7%], and diarrhea [6%]). Although more serious GI reactions such as bleeding, perforation or ulceration, appear less likely to occur with valdecoxib and the other selective COX-2 inhibitors than with older NSAIDs, pay particular attention to patients with prior history of peptic ulcer disease and/or GI bleeding. Other factors that increase risk of GI bleeding include treatment with oral corticosteroids or anticoagulants, older age, smoking and alcoholism.
In addition, some patients experienced fluid retention and edema when treated with NSAIDs and, in the clinical trials of valdecoxib, peripheral edema was reported in 2% of patients. These drugs should be used with caution in patients with fluid retention, hypertension, or heart failure.
Renal adverse events also occurred in some patients treated with NSAIDs, including renal papillary necrosis and a reduction in renal blood flow that may precipitate overt renal decompensation. Although these reactions are infrequent, the risk is greater when an NSAID is used on a long-term basis, and in elderly patients with impaired renal or hepatic function, or heart failure, and those taking a diuretic and/or angiotensin-converting enzyme inhibitor (ACEI). The risk of renal effects appears to be similar among the NSAIDs. Valdecoxib and the other selective COX-2 inhibitors have not been evaluated in patients with advanced renal disease, and their use is not recommended in these patients.
Borderline elevations of one or more liver function tests occurred in up to 15% of patients using NSAIDs, and notable elevations of alanine aminotransferase (ALT) and aspartate aminotransferase (AST), to three or more times the upper limit of normal in approximately 1% of patients. Rare cases of severe hepatic reactions including jaundice, hepatitis and hepatic failure, have also been reported. Although the risk of hepatic reactions with the use of valdecoxib appears to be very low, patients with signs, symptoms, or abnormal laboratory tests that suggest liver dysfunction should be carefully monitored. The use of valdecoxib in patients with severe hepatic impairment is not recommended.
Because of the possibility of premature closure of the ductus arteriosus, valdecoxib and other NSAIDs are not recommended in the third trimester of pregnancy. Valdecoxib is classified in Pregnancy Category C. It is not known whether the new agent is excreted in human milk and, when considering its use in a nursing mother, a decision should be made whether to discontinue nursing or not take the medication.
Following oral administration, valdecoxib achieves peak plasma concentrations in approximately 3 hours and its absolute bioavailability is 83%. Although the time to achieve peak plasma concentrations may be slightly delayed when the drug is taken with a high-fat meal, valdecoxib may be administered without regard to food. Valdecoxib is extensively metabolized and less than 5% of a dose is excreted unchanged in urine and feces. Approximately 70% of a dose is excreted in the urine as metabolites and about 20% as glucuronide derivative.
The recommended dosage of valdecoxib in the treatment of osteoarthritis and rherumatoid arthritis is 10 mg once a day and, in the treatment of primary dysmenorrhea is 20 mg twice a day as needed. The tablets are supplied in 10 mg and 20 mg potencies.
* Diagnostics
Rapid HIV Test Kit-OraQuick Rapid HIV-1 Antibody Test (OraSure Technologies, Inc.) is a rapid HIV diagnostic test kit, approved in November 2002, that provides results with 99.6 percent accuracy in as little as 20 minutes. Using less than a drop of collected blood, this test can quickly and reliably detect antibodies to HIV-1, the HIV virus that causes infection in most U.S. cases. Unlike other antibody tests for HIV, this test can be stored at room temperature, requires no specialized equipment, and maybe considered for use outside of traditional laboratory or clinical settings.
To perform the test, a fingerstick sample of blood is transferred to a vial and mixed with a developing solution. The test device, which resembles a dipstick, is then inserted into the vial. In as little as 20 minutes, the test will indicate if HIV-1 antibodies are present in the solution by displaying two reddish-purple lines. Although the results of rapid screenings will be reported in point-of-care settings, if the OraQuick test gives a reactive test result, it must be confirmed with an additional specific test such as the ELISA. The OraQuick test has not been approved to screen blood donors.
FDA currently categorizes the OraQuick test as "moderate complexity" under the Clinical Laboratory Improvement Amendments of 1988 (CLIA). Under CLIA, new tests are categorized as either moderate or high complexity. This designation means that the OraQuik test can only be given in CLIA-approved labs by CLIA-certified laboratory technicians or medical staff. If the test manufacturer applies for a CLIA waiver, the FDA can evaluate it for use under less stringent conditions.
The Centers for Disease Control and Prevention (CDC) estimates that one fourth of the approximately 900,000 HIVinfected people in the U.S. are not aware that they are infected. Because of the potential public health benefits of rapid HIV testing, the CDC and the Centers for Medicare and Medicaid Services (CMS) are working with state and other health officials to make the test widely available and to offer technical assistance and counseling training for its use.3
Lab Test for Congestive Heart Failure-The Elecsys proBNP Immunoassay (Roche Diagnostics, Inc.) is the first fully automated test for NT-proBNP, and is approved as an aid in diagnosing congestive heart failure. The immunoassay detects the level of a peptide, NT-proBNP, that is secreted almost exclusively by the heart. An elevated level may indicate the presence of congestive heart failure and the test can help clinicians differentiate between congestive heart failure and other problems, such as lung disease.
FDA approved the test based on the manufacturer's clinical studies of more than 2,000 healthy and sick men and women at 16 medical centers in the United States and Europe. The studies showed a relationship between the severity of congestive heart failure symptoms and the levels of NT-proBNP.4
* Device for Women's Health
FDA expedited review of the Essure System (Conceptus, Inc.) because of its potential benefit to couples seeking alternative means of sterilization. This small metallic implant is placed into the fallopian tubes of women who wish to be permanently sterilized. Unlike other currently available surgical sterilization procedures for women, placement of the device does not require an incision or general anesthesia.
During the implantation procedure, the clinician uses a special catheter to insert a device through the vagina, into the uterus and then into each of the fallopian tubes. The device induces scar tissue to form over the implant, blocking the fallopian tube and preventing fertilization.
During the first 3 months, women cannot rely on the Essure implants and must use alternate contraception. At the 3-month point, women must undergo a final x-ray procedure in which dye is placed in the uterus and an x-ray confirms proper device placement. Once placement is confirmed, the alternate contraception can be discontinued.
In one clinical trial, placement of the Essure implants in both fallopian tubes (bilateral placement) was achieved in 200 of 227 women. Following confirmation of placement after 3 months, 194 women began relying exclusively on the device to prevent pregnancy. Of those, 181 women relied on the device for at least 24 months and another 12 women relied on the device for at least 12 months. To date, none of the women have reported pregnancy.5
In a second study, bilateral placement of the Essure implants was attempted in 518 women between ages 21 and 40. All women used an alternate form of contraception for the first 3 months.
Following confirmation of proper placement, 449 women began relying on the device alone to prevent pregnancy. The women were then followed to see if any became pregnant or had any other adverse events. In this study, FDA considered 1-year data on 439 women, and 2-year data on 16 women. To date, none of these women have reported pregnancy.
Researchers failed to achieve bilateral placement of the Essure implants at first attempt with 14 percent of patients in the study.6 As a condition of approval, Conceptus will conduct a post-approval study to document the placement failure rate with newly trained clinicians and to identify factors associated with placement failure.
Because the device is meant for permanent sterilization, the FDA will require all study participants from both clinical studies to be followed for at least 5 years to evaluate long-term contraceptive effectiveness. Women who choose this device for sterilization should be aware that the procedure is irreversible, and should carefully evaluate their age and the possibility that they could wish to become pregnant in the future. Women should also know that pregnancies following sterilization can occur, even many years after the procedure, and are at increased risk to be ectopic, a life-threatening condition.
* Recalls
Pharmacia Corporation initiated a voluntary recall of Lunelle Monthly Contraceptive Injection (medroxyprogesterone acetate and estradiol cypionate injectable suspension) in prefilled syringes due to doubts of full potency and possible risk of contraceptive failure. As a precaution, Pharmacia is voluntarily recalling all Lunelle prefilled syringe lots currently on the market. Lunelle packaged in vials is not affected by this recall, nor is any other Pharmacia contraceptive product.
Lunelle is a combined hormonal contraceptive that is administered as a monthly injection. A sub-potent dose of Lunelle may not be effective in preventing pregnancy. Women who have been using Lunelle are advised to seek the advice of a health care professional regarding alternative methods of birth control and to use an additional barrier method of birth control (such as male or female condoms, diaphragm, or spermicide) until beginning a new form of hormonal contraception.7(
REFERENCES
1. FDA Talk Paper, October 8,2002 (www.fda.gov/bbs/topics).
2. Clinical Trial (unpublished). Reckitt-Benckiser Pharmaceuticals, Inc.
3. FDA Talk Paper, November 7,2002 (www.fda.gov/bbs/topics).
4 FDA Talk Paper, November 19, 2002 (www.fda.gov/bbs/topics).
5. Pivotal Trial (unpublished). Conceptus, Inc.
6 Kerin JF, Aust N Z J Obstet Gynaecol, 2001 Nov; Vol. 41 (4), pp. 364-70.
7. FDA News Release, October 10, 2002) Pharmacia Corporation Announces Voluntary Recall of Lunelle- Monthly Contraceptive Injection (www.fda.gov/bbs/topics).
Candace Berardinelli PhD, RN
Deborah Kupecz, PhD, NP
Copyright Springhouse Corporation Mar 2003
Provided by ProQuest Information and Learning Company. All rights Reserved