EVIDENCE-BASED ANSWER
When the standard therapies--mild topical corticosteroids and moisturizers--fail in the treatment of atopic dermatitis, patients are left with few proven remedies. The recently introduced topical immunosuppressive treatments--pimecrolimus and tacrolimus--offer an alternative to topical corticosteroids.
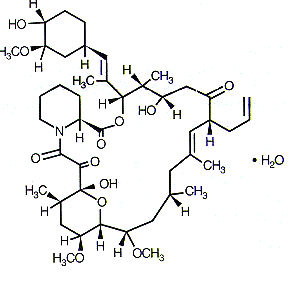
Tacrolimus 0.1% (Protopic) appears to be both safe and effective in treating eczema in adults and children (strength of recommendation [SOR]: A). In multiple studies, it has been as effective as potent topical corticosteroids and more effective than mild topical corticosteroids (SOR: A).
Pimecrolimus (Elidel) is more effective than placebo but less effective than potent topical corticosteroids (SOR: A). At this time, no data compare pimecrolimus with mild corticosteroids.
It is important to note that while the studies with the topical immunosuppressive agents included patients with mild to severe atopic dermatitis, none assessed the use of these agents on patients with steroid-refractory atopic dermatitis. The US Food and Drug Administration (FDA) has recommended limited use of these agents in atopic dermatitis because of potential cancer risk (SOR: C).
CLINICAL COMMENTARY
Benefits of topical immunosuppressants don't overcome cost and risks
This Clinical Inquiry is an excellent example of how evidence has to be used in a broader context when making clinical decisions, and how evidence is critical in evaluating both benefits and risks of treatments. There seems to be strong evidence that topical immunosuppressants are at least as good as topical steroids, but not better. They apparently do not have a lower risk of infection. We are then left with the only potential benefits being that of not causing HPA axis suppression and possibly not causing skin thinning.
However, this seems to be a small benefit for the enormous cost of these products (more than $60 for a 30-g tube) as well as increased burning on application. In the end, this is all trumped by the recent FDA Advisory warning of a potential cancer risk and advising use only as second-line agents and for short intermittent periods. The practical answer to this question, therefore, is to use the decades-old treatment of higher potency topical steroids with prudence.
Allen Daugird, MD
University of North Carolina, Chapel Hill
* Evidence summary
A recent meta-analysis included 25 randomized controlled trials involving tacrolimus and pimecrolimus. (1) This review included trials of tacrolimus and pimecrolimus in comparison with placebo, topical corticosteroids of varying strengths, and each other. They reported on both safety and efficacy. Fifteen vehicle-controlled trials of pimecrolimus and tacrolimus were reviewed. Both medications proved to be significantly more effective than the vehicle alone. A total of 3 trials (732 patients) compared tacrolimus 0.1% with potent topical corticosteroids (hydrocortisone butyrate 0.1%, beta-methasone valerate 0.1%) and found it to be as effective as the topical steroids after 3 weeks of application (number needed to treat [NNT]=6). (2,3)
At both the 0.03% and 0.1% strengths, tacrolimus was found to be more effective than mild topical corticosteroids (hydrocortisone acetate 1%) in 2 studies enrolling a total of 1183 children with moderate to severe atopic dermatitis (4,5) (NNT=5 for the tacrolimus 0.03%, and NNT= 3 for tacrolimus 0.1%). (6) A randomized, double-blinded, multicenter trial compared the use of pimecrolimus 1% cream with 0.1% triamcinolone acetonide cream and 1% hydrocortisone acetate cream for 658 adults with moderate-to-severe atopic dermatitis. (7) The majority of patients used either form of treatment for 1 year.
Although long-term safety and tolerability were similar, topical corticosteroids were more efficacious (NNT=13). Another study compared pimecrolimus 1% with betamethasone valerate 0.1% (a potent corticosteroid) in a study of 87 patients. (8) At the end of 3 weeks, the pimecrolimus 1% cream was significantly less effective than betamethasone valerate 0.1% (NNT=4).
In a meta-analysis of 3 randomized studies of head-to-head comparison of pimecrolimus 1% and tacrolimus 0.03% or 0.1% among children and adults, tacrolimus ointment was more effective than pimecrolimus cream at the end of the study for adults (P<.0001), for children with moderate-to-severe disease (P=.04), in the combined analysis (P<.0001), and at week 1 for children with mild disease (P=.04). No significant difference was seen in the incidence of adverse effects, although more pimecrolimus-treated patients withdrew from the studies because of a lack of efficacy (P [less than or equal to] .03) or adverse events (P=.002; pediatric mild). (9)
The authors of the first meta-analysis concluded that pimecrolimus 1% was more effective compared with placebo, less effective than potent topical corticosteroids, and had yet to be studied in comparison with low-potency topical corticosteroids. Tacrolimus 0.1% was more effective than placebo, more effective than mild corticosteroids, and as effective as potent topical corticosteroids. It was noted that both these agents caused more burning of the skin than topical corticosteroids--pimecrolimus 1% compared with betamethasone valerate 0.1% (number needed to harm [NNH]=50); tacrolimus 0.1% compared with betamethasone valerate 0.1% and hydrocortisone butyrate 0.1% (NNH=3); and tacrolimus 0.03% compared with the mild corticosteroid hydrocortisone acetate 1% (NNH=10). However, there was no significant difference in the rate of skin infections.
Recommendations from others
In 2003, a work group of dermatologists appointed by the president of the American Academy of Dermatology published a technical report on the guidelines of care for atopic dermatitis. (10) This group evaluated the effectiveness of several topical treatments for the treatment of atopic dermatitis. They noted that coal tar and its derivatives may reduce the severity of atopic dermatitis symptoms, but there are significant barriers to compliance. The severity of pruritus associated with atopic dermatitis may be reduced with shortterm use of topical doxepin.
Evidence supports the use of emollients in combination with other topical corticosteroid treatments to reduce the severity of atopic dermatitis. However, emollients need frequent application, which may be associated with poor compliance. The work group also concluded that both tacrolimus and pimecrolimus are effective and safe in reducing the severity of atopic dermatitis symptoms for both children and adults up to 1 year of treatment.
In March 2005, the FDA posted a Public Health Advisory and Alerts for Healthcare Professionals regarding the potential cancer risk from the use tacrolimus and pimecrolimus products when applied to the skin to treat atopic dermatitis. These creams will carry a "black box" warning regarding this potential risk. They recommended use only as a second-line therapy, at minimal amounts necessary, and for short periods of time, not continuously. They also recommended against their use for children aged <2 years and for people with diminished immune systems.
REFERENCES
(1.) Ashcroft D, Dimmock P, Garside R, Steinand K, Williams H. Efficacy and tolerability of topical pimecrolimus and tacrolimus in the treatment of atopic dermatitis: meta-analysis of randomized controlled trials. BMJ 2005; 330;516. Epub 2005 Feb 24.
(2.) Reitamo S, Rustin M, Ruzicka T, et al. Efficacy and safety of tacrolimus ointment compared with that of hydrocortisone butyrate ointment in adult patients with atopic dermatitis. J Allergy Clin Immunology 2002; 109:547-555.
(3.) FK506 Ointment Study Group. Phase III comparative study of FK506 ointment vs betamethasone valerate ointment in atopic dermatitis (trunk/extremities] [in Japanese]. Nishinihon J Dermatol 1997; 59:870-879.
(4.) Reitamo S, Van Leent E JM, Ho V, et al. Efficacy and safety of tacrolimus ointment compared with that of hydrocortisone acetate ointment in children with atopic dermatitis. J Allergy Clin Immunology 2002; 109:539-546.
(5.) Reitamo S, Harper J, Bos JD, et al. 0.03% tacrolimus ointment applied once or twice daily is more efficacious than 1% hydrocortisone acetate in children with moderate to severe atopic dermatitis: results of a randomized double-blind controlled trial. Br J Dermatol 2004; 150:554-562.
(6.) Flaherty RJ. A simple method for evaluating the clinical literature. Fam Pract Manag 2004; 47-52.
(7.) Luger T, Lahta M, Folster-Holst R, et al. Long term safety and tolerability of pimecrolimus cream 1% and topical corticosteroids in adults with moderate to severe atopic dermatitis. J Dermatol Treatment 2004; 15:169-178.
(8.) Luger T, Van Leent E JM, Graeber M, et al. SDZ ASM 981: an emerging safe and effective treatment for atopic dermatitis. Br J Dermatol 2001; 144:788-794.
(9.) Pallet AS, Lebwohl M, Fleischer AB Jr, et al. Tacrolimus ointment is more effective than pimecrolimus cream with a similar safety profile in the treatment of atopic dermatitis: results from 3 randomized, comparative studies. J Am Acad Dermatol 2005; 52:810-822.
(10.) American Academy of Dermatology. Guidelines of Care for Atopic Dermatitis. Technical report. 2003. Available at: www.aad.org/public/DermatologyA-Z/ Atoz_e.htm. Accessed on July 6, 2005.
FAST TRACK
The FDA has posted a Public Health Advisory regarding the potential cancer risk from these products when used to treat atopic dermatitis
Sara Trammell, MD, Amer Shakil, MD
Department of Family Medicine and Community Medicine, University of Texas
Southwestern, Dallas
Laura Wilder, MLS
University of Texas Southwestern Medical Center Library, Dallas
COPYRIGHT 2005 Dowden Health Media, Inc.
COPYRIGHT 2005 Gale Group