Abstract
Annular erythema is an unusual, often idiopathic disorder that tends to respond poorly to topical therapy.
Two patients with idiopathic, topical corticosteroid-resistant annular erythema showed prompt clearing of lesions treated with 0.1% tacrolimus ointment and persistence of untreated ones which themselves responded to subsequent treatment.
These two cases demonstrate a clear-cut therapeutic response of chronic, topical corticosteroid-resistant annular erythema to topical tacrolimus ointment 0.1% BID. Additional experience with tacrolimus ointment, hopefully in controlled circumstances, should clarify its potential value in treating annular erythema.
Case Report
Annular erythemas are unusual, often idiopathic lesions that occur most commonly in young and middle-aged adults. A small pink infiltrated papule slowly enlarges to form an annular, gyrate, or circinate lesion as the central area flattens and fades, often with fine scale trailing behind the advancing erythematous edge (1). Lesions may be solitary but are more commonly multiple. Although most cases are idiopathic, some are associated with infection, drugs, autoimmune diseases, hyperthyroidism, liver disease, and rarely, malignancy (2-9). Histology reveals a lymphohistiocytic infiltrate around vessels in the papillary and upper reticular dermis. Epidermal changes, if present, include spongiosis, focal parakeratotic scale, and exocytosis of lymphocytes (10). Specific treatment of annular erythema is directed at eradication of the underlying cause. Idiopathic cases often respond poorly to topical and oral corticosteroids, and eventually tend to resolve on their own. Below we describe two individuals who showed a clear-cut therapeutic response to tacrolimus ointment.
Case 1
A 42-year-old woman with a past medical history of depression and hypercholesterolemia presented with a 2.2 cm x 1.4 cm erythematous lesion with raised border and central clearing on her left cheek. The patient had a history of similar lesions on her breast and leg that had spontaneously resolved after 2-3 months. 3 mm punch biopsy revealed an unremarkable epidermis with a superficial and deep perivascular dermal lymphocytic infiltrate. Complete blood count was 12,900, anti-nuclear antibodies (ANA) were negative, and sedimentation rate was 3. The patient was treated with mometasone furoate 0.1% cream BID to the annular cheek lesion. On follow up two weeks later, it appeared that the annular lesion was resolving; however, one month later the lesion recurred despite continuation of the topical corticosteroid, and a new, similar lesion appeared on her back (Figure 1). Her medications (sertraline, bupropion, niacin, simvastatin, and pantoprazole) had been stopped for several weeks without any effect on the rash. She was then treated with tacrolimus ointment 0.1% BID to the facial lesion only. On follow up three weeks later, this lesion was resolving, but her back lesion was slightly larger. The lesion of the back was then treated with tacrolimus ointment 0.1% BID. On follow up three weeks later, the upper three-fourths of this lesion was resolving as well; this corresponded to her ability to reach the lesion for ointment application. The lesion on her cheek was almost completely gone.
[FIGURE 1 OMITTED]
Case 2
A 56-year-old woman with a past medical history of diabetes, hypertriglyceridemia, and hypertension presented with a five-year history of annular, scaly, darkly erythematous lesions of her legs (Figure 2). KOH was negative and the lesions did not respond to topical clotrimazole, betamethasone cream, or ketoconazole cream. The patient's oral medications were glipizide, metformin, lisinopril, conjugated estrogens, and gemfibrozil. She described repeated exacerbations of the rash that responded to clobetasol propionate 0.05% cream. The patient presented with a flare-up that was resistant to topical corticosteroids. Tacrolimus ointment 0.1% was applied BID to the left leg only. On follow up two weeks later, the left leg revealed post-inflammatory hyperpigmentation and mild scaling but no erythema or induration. The patient then applied tacrolimus 0.1% BID bilaterally with similar resolution of the right leg lesion six weeks later.
[FIGURE 2 OMITTED]
Discussion
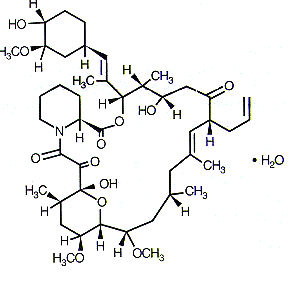
These two cases demonstrate a clear-cut therapeutic response of chronic, topical corticosteroid-resistant annular erythema to topical tacrolimus 0.1% ointment. Topical tacrolimus ointment has been used with success in atopic dermatitis (11,12). Case reports have shown success of topical tacrolimus in treating psoriasis, pyoderma gangrenosum, alopecia areata, and lichen planus (13). Tacrolimus binds to immunophilin proteins in the cytoplasm of lymphocytes, and this complex then binds calcineurin, resulting in inhibition of transcription of T-cell activation genes encoding a number of pro-inflammatory cytokines (14).
Claims of therapeutic success in conditions prone to spontaneous clearing can be a "tough sell." When large controlled trials are not feasible and when topical therapy is appropriate, the technique of treating some lesions and leaving others as untreated controls can generate useful data with few patients. The ideal scenario occurs when asymmetrical dermatoses are treated in a paired comparison with one side receiving active drug and the other receiving vehicle as a control with applications performed by the investigator. For practical reasons our cases were not handled with quite this degree of vigor. No vehicle control for tacrolimus ointment was available, and in only one of the cases was there symmetric disease. We also had to rely on patients to apply their own treatment.
Despite these limitations, the prompt clearing of treated lesions with persistence of untreated ones that then responded to subsequent treatment seems hard to dismiss as spontaneous resolution. Additional experience with tacrolimus ointment, hopefully in controlled circumstances, should clarify its potential value in treating annular erythema.
References
(1.) Dowd PM. Champion RH. Annular Erythema. In: Textbook of Dermatology (Champion RH, Burton JL, Burns DA, Breathnach SM, eds), 6th ed. Oxford, Blackwell Scientific Publications, 1998; 2087-9.
(2.) Phillips W, et al. Erythema annulare centrifugum unresponsive to immunosuppressive therapy. Br J Dermatol 1994; 131:587.
(3.) Furue M, et al. Erythema annulare centrifugum induced by molluscum contagiosum. Br J Dermatol 1993; 129:646-7.
(4.) Borbujo J, et al. Erythema annulare centrifugum and Escherichia coli urinary infection. Lancet 1996; 347:897-8.
(5.) Tsuji T, et al. Erythema annulare centrifugum associated with gold sodium thiomalate therapy. J Am Acad Dermatol 1992; 27:284-7.
(6.) Garty, B. Erythema annulare centrifugum in a patient with polyglandular autoimmune disease type 1. Cutis 1998; 62:231-2.
(7.) Watanabe T, et al. Annular erythema associated with lupus erythematosus/Sjogren's syndrome. J Am Acad Dermatol 1997; 36:214-8.
(8.) Kawakami T, Saito R. The relationship between facial annular erythema and anti-SS-A/Ro antibodies in three East Asian women. Br J Dermatol 1999; 140:136-40.
(9.) Tsuji T, Kadoya A. Erythema annulare centrifugum associated with liver disease. Arch Dermatol 1986; 122:1239-40.
(10.) Hood AF. Superficial and Deep Infiltrates of the Skin. In: Pathology of the Skin (Farmer ER, Hood AF, eds), 1st edn. Norwalk, Appleton and Lange, 1990; 193.
(11.) Hannifin J, et al. Tacrolimus ointment for the treatment of atopic dermatitis in adult patients: Part I, Efficacy. J Am Acad Dermatol 2001; 44(1 Suppl):S28-38.
(12.) Soter N, et al. Tacrolimus ointment for the treatment of atopic dermatitis in adult patients: Part II, Safety. J Am Acad Dermatol 2001; 44(1 Suppl):S39-46.
(13.) Skaehill, P. Tacrolimus in Dermatologic Disorders. The Annals of Pharmacotherapy 2001; 35:582-587.
(14.) Zabawski E, et al. Tacrolimus: Pharmacology and Therapeutic Uses in Dermatology. International Journal of Dermatology 2000; 39:721-727.
(15.) Bressler G, Jones R. Erythema Annulare Centrifugum. J Am Acad Dermatol 1981; 4:598-602.
(16.) Gniadecki R. Calcipitriol for erythema annulare centrifugum. Br J Dermatol 2002; 146:317-9.
(17.) Ling, MR. Topical Tacrolimus and Pimecrolimus: Future Directions. Seminars in Cutaneous Medicine and Surgery 2001; 20:268-274.
(18.) Tyring, S. Reactive Erythemas: Erythema Annulare Centrifugum and Erythema Gyratum Repens. Clinics in Dermatology 1993; 11:135-9.
(19.) White, J. Gyrate Erythema. Dermatologic Clinics 1985; 3:129-39.
NIKHIL G RAO BA (1)
ROBERT J PARISER MD (2)
(1) MEDICAL STUDENT, UNIVERSITY OF VIRGINIA SCHOOL OF MEDICINE, CHARLOTTESVILLE, VIRGINIA
(2) PROFESSOR, DEPARTMENT OF DERMATOLOGY AND ASSISTANT PROFESSOR, DEPARTMENT OF PATHOLOGY, EASTERN VIRGINIA MEDICAL SCHOOL, NORFOLK, VIRGINIA
ADDRESS FOR CORRESPONDENCE:
Robert J Pariser
601 Medical Tower,
Norfolk, Virginia 23507
Phone: 757-622-6315
Fax: 757-625-6940
E-mail: rpariser@pol.net
COPYRIGHT 2003 Journal of Drugs in Dermatology
COPYRIGHT 2003 Gale Group