Two of the agents widely used to treat bipolar illness are established teratogens. Lithium is associated with a 0.05% risk of Ebstein's anomaly, a modest teratogenic effect. Sodium valproate is associated with a risk as high as 8% for major congenital malformations, most notably, neural tube defects and cardiac malformations, according to recent data from the North American Antiepileptic Drug (AED) Pregnancy Registry.
This increased risk for major organ malformations associated with first trimester exposure to these compounds raises concerns about the possible risk of longer term neurobehavioral sequelae associated with prenatal exposure.
Several studies published over the last few years have consistently shown an association between developmental delay and an increased risk for behavioral problems associated with in utero exposure to anticonvulsants, particularly sodium valproate. This growing literature has suggested associations between in utero exposure and higher rates of problems ranging from mild behavioral disruption in school, attention-deficit disorder, and other behavioral problems characterized by hyperactivity, autistic-like behaviors, and problems with learning, speech delay, and gross motor delay.
One study of 52 children exposed to anticonvulsants in utero found that 77% had developmental delay or learning difficulties when followed up at a mean age of 6 1/2 years; 80% had been exposed in utero to sodium valproate (J. Med. Genet, 2000;37:489-97).
In another prospective study, children born to women with epilepsy were assessed between ages 4 months and 10 years. The risk of adverse outcomes, including developmental delay, was higher among those exposed to sodium valproate than carbamazepine (Tegretol). Most of the cases were children born to women who received sodium valproate doses that were greater than 1,000 mg/day (Seizure 2002;11:512-8).
These studies were not ideally designed and have inherent methodologic limitations. Eventually, we will have long-term prospective data on children exposed in utero to anticonvulsants. These data will come from the North American AED Registry. Until then, however, the findings of these studies are consistent enough to indicate that in utero exposure to anticonvulsants may have neurotoxic effects; this appears to be the case particularly with sodium valproate monotherapy and polytherapy.
The potential for neurobehavioral sequelae is an issue that has not been adequately factored into the risk-benefit decision for treating women with epilepsy or bipolar disorder during pregnancy. For women with epilepsy, the situation is more difficult, since seizures during pregnancy are associated with particularly bad perinatal outcomes. But for bipolar disorder, we have a spectrum of treatment options.
Often women and their physicians choose to discontinue a psychotropic drug in the first trimester, and they assume that therapy can safely be reintroduced during the second trimester. Still, the data on potential behavioral toxicity, particularly with sodium valproate, should make one pause before reinstituting treatment with sodium valproate during the second and third trimester--and the data should raise the question of whether this is an appropriate medicine to be using at any point during pregnancy in women with bipolar illness.
There is no perfect answer. The goal is to keep women emotionally well during pregnancy and to avoid relapse during pregnancy. Prenatal exposure to a drug is sometimes necessary to sustain well-being of patients. Nevertheless, recent data have indicated that the risk of polycystic ovarian syndrome is increased in women treated with sodium valproate. When this finding is considered with the teratogenicity data for sodium valproate and its possible longer term neurobehavioral sequelae, one has to reconsider the wisdom of using this medication in reproductive-age women, particularly since some of the treatment alternatives for bipolar illness are either less teratogenic or appear to be nonteratogenic.
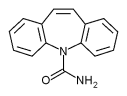
Reproductive-age women who want to become pregnant or who are already pregnant should consult their physicians about alternative treatment strategies that can be continued throughout pregnancy. Such alternatives are lithium or lamotrigine (Lamictal), both of which may be used with or without one of the older typical antipsychotics, which do not appear to be teratogenic.
Our goal is to avoid exposure to a drug with known teratogenicity with respect to organs, and quite probably, with respect to behavior.
BY LEE COHEN, M.D.
DR. COHEN directs the perinatal psychiatry program at Massachusetts General Hospital, Boston, which offers information about pregnancy and mental health at www.womensmentalhealth.org. He is a consultant to GlaxoSmithKline, manufacturer of Lamictal, and has conducted research funded by GlaxoSmithKline and by Abbott Pharmaceuticals, manufacturer of Depakote.
COPYRIGHT 2004 International Medical News Group
COPYRIGHT 2005 Gale Group