Think of someone - a child or an adult - racked by uncontrolled coughing. With a heaving, distended chest, neck muscles straining, and eyes showing alarm verging on panic, the Person can utter only a few brief words between rasping, wheezing, frantic efforts to breathe.
The person puts a tubelike device in his or her mouth and inhales twice. Within minutes, remarkably it seems, the crisis is over. Breathing returns to normal. The person can go back to school or work or even jogging - until the next attack, which might be hours or months away.
Asthma attacks are often milder than this description - just a shortness of breath that soon passes without treatment. But they can also be much, much worse, requiring a hurried trip to the hospital for emergency - sometimes lifesaving - care. Even in severe cases, hospital treatment usually enables asthma patients to regain near-normal breathing. But not always. Almost 5,000 asthma deaths were reported in the United States in 1992, according to the American Lung Association (1992 is the most recent year for which statistics are available). Most of the deaths occurred in patients who misjudged the severity of symptoms or failed to reach a hospital or clinic in time to prevent respiratory failure.
Although African-Americans make up approximately 12 percent of the U.S. population, they account for 21 percent of deaths due to asthma, according to the American Lung Association.
For reasons that are not well understood, the number of newly diagnosed cases of asthma in the United States is rising sharply, up 56.7 percent between 1982 and 1992. Asthma deaths, too, are climbing - 4,964 in 1992 compared with 2,598 in 1979. Lack of necessary health care, especially among the urban poor, is thought to play an important role in the rising asthma death rate.
Ironically, these increases are taking place at a time when some things believed to be associated with asthma - such as air pollution, dust, molds, and tobacco smoke - are better understood and often under better control than they once were. The reason for the increases remains a mystery, but some investigators think one contributing factor is modern, tightly sealed homes and workplaces that trap and recirculate contaminants, increasing exposure to them in the air we breathe.
Inflamed Airways
Most of America's 12 million to 14 million people with asthma, of whom more than 4 million are under age 18, have a relatively mild illness. About a quarter of asthmatic children seem to "outgrow" their disease in their teen years or as young adults. It's not certain, however, that they are completely free of asthma. Studies of people with late-onset asthma - asthma that first shows up in the fifth or sixth decade of life or even later - have found that many of them experienced asthma-like breathing difficulties as children.
There is no known cure, but most asthma can be controlled by a strategy aimed at preventing acute episodes and halting those that do occur.
This two-pronged attack is increasingly effective because scientists are piecing together a more comprehensive picture of the nature of asthma and gaining new insights into the cause, prevention and management of acute asthma attacks. New information is changing the way practicing physicians and the Food and Drug Administration view the role of drugs in asthma treatment and prevention.
Changing Theories
Until the 1970s and early 1980s, asthma was understood to result from over-responsiveness of the tubes (bronchi and bronchioles) that carry air to and from the lungs. People with hypersensitive airways, when exposed to certain irritants called "triggers" - such as household dust, tobacco smoke, cat fur (dander), cockroach droppings, air pollutants, even vigorous exercise or cold air - would experience "bronchospasm," a narrowing of the airways caused by contraction of the muscles that encircle the bronchial tubes.
Asthmatics also tend to produce thick, sticky mucus and have inflamed, damaged airways, both of which worsen the breathing restriction caused by bronchospasm. During an acute attack, asthmatics seem to have a hard time getting their breath. Actually they are struggling to push air out of over-inflated lungs through constricted airways.
That understanding of asthma led to treatments aimed primarily at opening up the bronchial tubes by using drugs that cause the bronchial muscles to relax their grip on air passages. Bronchodilators are still a mainstay of asthma therapy. But Robert Meyer, M.D., of FDA's Center for Drug Evaluation and Research, notes that scientists' understanding of asthma has changed significantly over the last decade or so.
He points out that since the early 1980s, increasing scientific evidence shows that inflammation is as much responsible for bronchospasm as anything else. Today, Meyer says, "putting primary emphasis on controlling bronchospasm rather than chronic airway inflammation "looks like putting the cart before the horse."
The evidence Meyer refers to strongly indicates that asthma is a chronic inflammatory disease that usually develops within the first few years of life. Much of this evidence is discussed by H.W. Kelly of the University of New Mexico College of Pharmacy in the October 1992 issue of the Journal of Clinical Pharmacology and Therapeutics.
In people with asthma, whether mild or severe - even in asthmatics whose first acute attack occurs long after childhood - the air passages are continuously inflamed, causing them to be swollen and to react strongly to inhaled irritants. But because patients may not be aware of any symptoms, this inflammation is sometimes called "the quiet part" of asthma.
People with chronically inflamed airways may show no outward signs of asthma until the first acute attack requires urgent medical attention, often at a hospital emergency department. Emergency care physicians and nurses - who are all too familiar with acute asthma - are able to administer powerful drugs to open the patient's air passages and restore virtually normal breathing. They are likely to recommend the patient be seen by an asthma specialist, who can devise a combination of treatment and prevention measures aimed at avoiding or minimizing further acute asthma attacks. The first step in that process is an accurate diagnosis.
Diagnosing Asthma
The diagnosis of asthma is based on repeated, careful measurements of how efficiently the patient can force air out of the lungs and on a thorough medical history and laboratory tests to find out what "triggers" the patient's acute attacks.
People with asthma react to external irritants in a way that non-asthmatics don't. Many but not all asthmatics have allergies that cause their bodies to produce an abnormal array of chemicals in response to environmental allergens. In that sense, asthma is akin to pollen allergies, hives, and eczema. But in asthma, the allergic reaction contributes to inflammation of the airways rather than of skin, eyes, or nose and throat. An acute asthma attack may come on rapidly after exposure to an irritant or develop slowly over several days or weeks, which can complicate the job of identifying a patient's asthma "triggers."
Which drugs asthma patients need, when to use them, and how much to use depend largely on the character of their illness, as shown by the degree of breathing impairment, and the frequency and severity of acute attacks. Asthma experts agree, however, that the first line of defense is avoidance of whatever brings on an acute asthma episode. Though for most patients "triggers" - there are often more than one - are likely to be common allergens or air pollutants. In some asthmatics, attacks can be brought on by strenuous exercise, exposure to cold outdoor air, industrial or household chemicals (cleaning fluids, for example), and food additives such as sulfites. In other cases, the triggers cannot be identified, even after a thorough investigation.
Asthma Drugs
Knowing what provokes an asthma attack is critically important in prevention, but it's often difficult or impractical to avoid contact with triggering irritants. Today, however, physicians can prescribe drugs to lessen the risk of acute attacks after exposure to an offending irritant, as well as halt attacks that can't be prevented.
The drugs used to treat asthma fall into two broad categories: controllers to prevent acute attacks and relievers that check acute symptoms when they occur. Some drugs do both.
In light of mounting evidence that asthma is fundamentally an inflammatory disease, asthma authorities today regard inhaled corticosteroids - marketed under numerous brand names, including Aerobid, Azmacort, Beclovent, and Vanceril - as the most effective agents for controlling airway inflammation and thus preventing acute asthma attacks. Corticosteroids in pill or tablet form (such as Medrol) and in liquid form for children (such as Pediapred and Prelone) are prescribed for some patients with severe asthma.
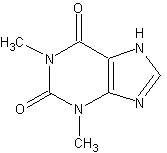
Other inhaled anti-inflammatory controller drugs include Intal (cromolyn sodium), which is useful in preventing asthma brought on by exercise, and Tilade (nedrocromil sodium). Long-acting inhaled bronchodilators, such as Serevent (salmeterol), and long-acting oral bronchodilators, such as Alupent (metaproterenol), Proventil (albuterol sulfate), Theo-24 (theophylline anhydrous), and many others, are often used in conjunction with anti-inflammatory agents to control symptoms. They don't provide immediate relief of symptoms, but their preventive action persists for many hours, which makes them useful in controlling attacks that might occur during hours of sleep.
Drugs to bring quick relief in acute asthma attacks are chiefly short-acting inhaled bronchodilators that act rapidly but for a relatively brief time to relax bronchial constriction. There are many short-acting bronchodilators to chose from, including Alupent or Metaprel (metaproterenol), Brethaire (terbutaline), and Ventolin or Proventil (albuterol). Although these drugs are effective in treating asthma, there is some controversy about their safety, especially when they are overused. Scientific debate makes it clear, however, that an increasing need for inhaled bronchodilators, or a decreasing response to each dose, is a signal that the patient's asthma is not being adequately controlled. Patients who have an increasing need for short-acting inhaled bronchodilators should be reevaluated promptly by their physicians.
Nonprescription Products
Both prescription and over-the-counter (OTC) short-acting bronchodilators are available. The OTC drugs generally contain lesser amounts of the active agent than prescription forms and are effective for a shorter period. They may be useful, however, as temporary treatment for mild asthma attacks. Ready availability in drugstores makes the OTC products potentially helpful as a "stopgap" for patients who do not have their prescription medication at hand when an asthma attack occurs.
In July 1995, FDA removed from the market OTC bronchodilators such as Primatene tablets that contain theophylline. The agency determined that the amount of such products needed to improve breathing could be toxic or lifethreatening for some people. In addition, the agency's review of numerous studies found no evidence that the theophylline in these OTC drug products contributed to the treatment benefits claimed for them.
The key to effective, long-term treatment of asthma is finding the drugs and dosage plan most effective in dealing with or preventing acute episodes. But effective treatment depends as well on the patient and the care-giver knowing what the various anti-asthma drugs do, when and in what amount each drug should be used, when a change in symptoms or in the response to a particular drug requires a call or visit to the physician, and when to get emergency help. Physicians who specialize in treating asthmatics go over these points in detail as part of an overall treatment plan designed and, as necessary, adjusted to meet needs of each individual patient.
A cure for asthma is judged by experts to be still a far-off possibility. But the majority of asthma sufferers can lead essentially normal, symptom-free lives by understanding and sticking to a well-planned strategy to keep clear of asthma triggers and to use the right drugs in the right way.
It isn't easy, but it works.
COPYRIGHT 1996 U.S. Government Printing Office
COPYRIGHT 2004 Gale Group