To determine the impact of transplantation-associated injury on the clearance mechanisms of pulmonary edema, we created a canine single lung transplant model. After 3 hours of preservation and 4 hours of reperfusion, right native lungs and left transplanted lungs were used to measure alveolar liquid clearance (ALC) in ex vivo liquid-filled lung preparations. We also examined the role of the pulmonary circulation in edema clearance in in vivo liquid-filled lungs between 4 and 8 hours of reperfusion. To study molecular modifications in ALC, we also measured expression levels of the epithelial sodium channel (ENaC) and sodium-potassium-adenosine triphosphatase (ATPase). We found that ALC was significantly lower in transplanted than in right native lungs ex vivo (p
Keywords: lung transplantation; ischemia-reperfusion injury; alveolar liquid clearance; epithelial sodium channel; sodium-potassium-adenosine triphosphatase
Lung transplantation has become a successful therapeutic option in several types of end-stage lung diseases for nearly 2 decades (1). However, primary graft failure in the early postoperative period continues to be a significant cause of morbidity and mortality despite advances in perioperative patient management (2, 3). Primary graft failure is considered to be secondary to ischemia-reperfusion injury leading to noncardiogenic pulmonary edema (4). Although the precise mechanisms culminating in this pathophysiological condition remain unclear, neutrophils are believed to play a significant role in the process (4).
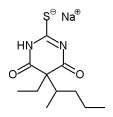
Accumulating evidence indicates that the capacity of the lungs to clear edema liquid is essential for the evolution and prognosis of cardiogenic and noncardiogenic pulmonary edema (5, 6). The physiological process of edema clearance most likely takes place in the alveolar spaces and depends on active sodium (Na+) transport. The Na+ channel at the apical surface and sodium-potassium-adenosine triphosphatase (Na+-K+-ATPase) at the basolateral surface of alveolar type II pneumocytes are two essential components of the transepithelial transport system (7-10). Through this mechanism, Na+ is actively transported from the apical to the basolateral side of alveolar epithelial cells (7, 10), creating an osmotic gradient that leads to transalveolar liquid transport.
One clinical study has suggested that alveolar liquid clearance (ALC) might be important for the resolution of pulmonary edema associated with lung transplantation (11). In fact, in patients suffering from reperfusion lung injury with no net alveolar liquid fluid clearance, the trend is toward more prolonged stays in the intensive care unit, and longer mechanical ventilation (11). Although some studies have evaluated the effect of ischemia-reperfusion on ALC (12), there are no experimental data on the impact of actual lung transplantation on ALC. The objective of the present study was to determine if ALC is altered in an experimental model of canine left lung transplantation. ALC was measured in both ex vivo and in vivo liquid-filled lung preparations. The influence of [beta]-adrenergic stimulation was also examined, because [beta]-adrenergic agonists have been shown to increase ALC in normal and mildly injured lungs (13-15). Finally, to explore the mechanisms that could explain the abnormal ALC observed in our model, we investigated the effect of preservation and reperfusion on messenger RNA (mRNA) and protein expression levels of the epithelial Na+ channel (ENaC) and mRNA expression levels of Na+-K+-ATPase because these two molecules are considered essential for transalveolar Na+ transport (16, 17).
METHODS
Animals
The rate of transalveolar liquid transport is known to vary between species (18). Because we wished to create an animal model relevant to clinical lung transplantation, we chose the dog, a well-defined lung transplantation paradigm with an ALC rate similar to that in humans (19, 20). We used 32 dogs of either sex weighing 18-25 kg. Eleven left orthotopic lung transplants were performed in 11 size-matched animals, including one experiment for the sole purpose of histologic analysis. Ten dogs underwent a left-sided thoracotomy only and served as control animals. These experiments were conducted in accordance with the Principles of Laboratory Animal Care formulated by the Institute of Laboratory Animal Resources and the Guide for the Care and Use of Laboratory Animals (National Institutes of Health Publication No. 86-23, revised 1985) as applied by the institutional animal care committee of the Centre hospitalier de l'Universite de Montreal.
Surgical Procedures
Surgical procedure for harvesting donor lungs. Each donor was anesthetized by intravenous injection of thiopental sodium (10 mg/kg; Abbott Laboratories Limited, St-Laurent, Montreal, Quebec, Canada) after intramuscular injection of glycopyrrolate (0.01 mg/kg; Sabex Inc., Montreal, Quebec, Canada), Atravet (0.04 mg/kg; Ayerst Laboratories, Boucherville, Quebec, Canada), and Meperidine (4 mg/kg; Sabex) as premedication. After endotracheal intubation, the dogs were ventilated with a volume-cycled ventilator (Harvard Apparatus, Dover, MA) at a tidal volume of 18 ml/kg, a respiratory rate of 15 breaths/minute, an inspiratory oxygen concentration of 1.0, and a positive end-expiratory pressure of 5 cm water. Anesthesia was maintained with isoflurane (1.5%; Abbott Laboratories Limited) and intravenous Cisatracurium (0.05 mg/kg; GlaxoWellcome Inc., St-Laurent, Quebec, Canada). After a median sternotomy, heparin sodium (400 U/kg; Leo Pharma Inc., Ajax, Ontario, Canada) was given intravenously, and a catheter was inserted into the trunk of the pulmonary artery (PA). Immediately after clamping the superior vena cava and the ascending aorta, and sectioning of the inferior vena cava and left atrial appendage, the donor pulmonary vasculature was flushed with cold modified Euro-Collins solution (50 ml/kg; Baxter Corporation, Toronto, Ontario, Canada) through the PA catheter at a height of 30 cm. Topical cooling was achieved with cold Ringer's lactate solution. After flushing, the lungs were inflated with ambient air, clamped at the trachea, excised, and placed in a plastic bag containing Ringer's lactate solution. The bag was sealed and placed in crushed ice.
Surgical procedure for the recipients. The recipients were anesthetized by the same procedures as for the donors. Before performing a left-sided thoracotomy, a 16-gauge catheter was inserted in the femoral artery for arterial pressure measurements and blood sampling, and a 7 Fr. Swan-Ganz catheter was introduced into the PA for pressure measurements. The native left lung was excised through a left-sided thoracotomy. The donor lungs were taken from the plastic bag, and the left PA, left main bronchus, and left atrium were dissected free. Anastomoses of the left main bronchus, left PA, and left atrium were performed. The lung was reperfused, and ventilation was re-established; thereafter, the animals were monitored for 4 hours (in the ex vivo liquid clearance group) (n = 6), or for 8 hours (in the in vivo liquid clearance group) (n = 4). Total ischemic time was 193 + or - 4 minutes. Mean arterial pressure, mean pulmonary arterial pressure, and heart rate were recorded during anesthesia. Arterial blood samples were taken before and hourly after surgery.
Surgical procedure for control animals. We conducted experiments in a group of animals that only underwent a left-sided thoracotomy (without lung resection) and anesthesia, because halothane and isoflurane have been shown to decrease ALC in rats (21). Immediately after left-sided thoracotomy under the same conditions as in the transplantation groups, the thoracotomy incision was closed, and the animals were monitored for 4 hours (n = 6) or 8 hours (n = 4) and subjected to the same ex vivo or in vivo ALC measurements. All these procedures were performed with minimal manipulation of the lungs. The same physiological measurements were recorded as in the experimental group.
ALC Studies
Ex vivo ALC measurements. Six transplanted animals and six control animals were used to evaluate ALC in ex vivo fluid-filled lung preparations after 4 hours of reperfusion after transplantation. With this technique, we could assess ALC from different lobes in the same animal, allowing us to study ALC with and without [beta]-adrenergic agonist stimulation. Furthermore, we could compare ALC between transplanted and native right lungs of the same animal. This approach has a physiological rationale because it was shown recently that ALC is similar in different lobes of the lung (20).
For these measurements, a clamshell incision was made 4 hours after reperfusion, and the animals were killed by cross-clamping the PA and ascending aorta. The heart-lung block was removed, and the transplanted left lung and native right lung were divided into three lobes on each side. The middle lobes were blotted, snap-frozen in liquid nitrogen, and stored at - 40[degrees]C for mRNA, wet-to-dry lung weight ratio, and lung myeloperoxidase (MPO) activity analyses.
The upper and lower lobes from each side were separated and prepared for ALC measurements. To do this, each bronchus was cannulated with a catheter (Tygon Tubing; Cole-Parmer Instrument Co., Vernon Hills, IL) connected to a stopcock; the lobe was then inserted in a plastic bag, sealed, and placed in a water bath at 37[degrees]C for the duration of the experiment. Through the catheter, we instilled, into each lobe, a solution (130 mM Na+, 4 mM K+, 1.5 mM calcium ions, 109 mM chloride ions, 28 mM lactate, 11.1 mM glucose, 5.0 g/dl bovine serum albumin (Sigma Chemical Co., St. Louis, MO)) prewarmed to 37[degrees]C. As baseline, we aspirated approximately 700 [mu]l of this solution 1 minute after instillation and considered it as the initial alveolar liquid. To examine the effect of [beta]-adrenergic stimulation on ALC, we added 10^sup -5^ M terbutaline (Sigma Chemical Co.) to the instillate solution of one lobe on each side (left transplanted and right native lungs). After 4 hours, the instillate solution was aspirated and used as the final alveolar liquid. The aspirated liquid was then centrifuged (5,000 rpm for 5 minutes), and the supernatant was collected for the measurement of total protein concentration by the Biuret method (22).
ALC was calculated from initial (1 minute after instillation) and final alveolar protein concentrations with the following formula (13, 23): ALC (%) = (V^sub i^ X Fw^sub i^-V^sub f^ x Fw^sub f^)/(V^sub i^ x Fw^sub i^) x 100, where Fw is the water fraction of the initial (i) and final (f) alveolar liquid. The water fraction is the volume of water per volume of solution measured by the gravimetric method. V represents the volume of the initial (i) and final alveolar liquid (f), and V^sub f^ is calculated by the following equation: V^sub f^ = (V^sub i^ x TP^sub i^)/TP^sub f^, where TP is the protein concentration.
In vivo measurements. Because ALC measurements in nonperfused lungs, as used in our ex vivo preparations, can be altered in the presence of interstitial edema (24), we also quantitated ALC in in vivo preparations where the pulmonary circulation remains intact. These experiments were performed in four transplanted dogs and four control animals in an identical manner to the previous experiments except that 4 hours after transplantation, a left-sided thoracotomy was undertaken, the left lower lobe bronchus was cannulated, and 30 ml of the prewarmed instillate solution (composition identical to that in the ex vivo experiments) were introduced into the left lower lobe. The instilled lobe was kept inflated by continuous positive air pressure of 6 to 7 cm water (FI^sub O^sub 2^^ = 0.21) but not ventilated. About 1 ml of alveolar liquid was aspirated 1 minute after instillation as the initial alveolar liquid, and approximately 700 [mu]l was aspirated every hour for 4 hours to calculate the ALC, using the methods and formulas described previously. Eight hours post-transplantation, the animals were killed by cross-clamping of the PA and ascending aorta, and the heart-lung block was removed. The lung was divided into lobes that were snap-frozen in liquid nitrogen and stored at -40[degrees]C for further study (mRNA, lung MPO and mRNA analyses).
To compare the findings of ALC obtained in our model with clinical data, we also measured the pulmonary edema liquid-to-plasma total protein concentration ratio (5), an approach similar to the one used in the clinical setting to monitor the integrity of the alveolar-capillary barrier. To do so, at the time of alveolar liquid aspiration, an arterial blood sample was drawn to measure plasma total protein concentration. We then used the total protein concentrations of the alveolar liquid and plasma samples to calculate the pulmonary edema liquid-to-plasma total protein concentration ratio at each time point over 4 hours.
Northern Blot Hybridization and Western Blotting
Total RNA was prepared from lung tissues by homogenizalion and acid phenol/chloroform extraction with TRIZOL reagents (Life Technologies, Grand Island, NY) following the manufacturer's instructions. Total RNA was measured by absorption spectrophotometry at 260 nm. The 260/280 ratio averaged 1.6 to 1.8. For Northern blotting, 10 [mu]g/ lane of total RNA was fractionated by electrophoresis on 1% agarose-formaldehyde gel. Total RNA was transferred to GeneScreen nylon membranes (NEM, Boston, MA) by overnight blotting with 10x standard sodium citrate buffer. The membranes were ultraviolet-cross-linked, baked, and stored at 4[degrees]C until hybridization, which was performed overnight with deoxycytidine 5-triphosphate ^sup 32^P random-labeled (Multiprime DNA kit; Amersham Biosciences Inc., Baie d'Urfe, Quebec, Canada), full-length or subunit-specific short cDNA probes for [alpha]ENaC, [beta]ENaC, [alpha]^sub 1^Na+-K+-ATPase, or [beta]^sub 1^Na+-K+-ATPase. The [alpha], [beta], and -[gamma]ENaC probes were gifts from Dr. B.C. Rossier (Institut de Pharmacologie et de Toxicologie, Universite de Lausanne, Lausanne, Switzerland), and the [alpha]^sub 1^ and [beta]^sub 1^Na+-K+-ATPase probes were gifts from Dr. J. Orlowski (Physiology Department, McGill University, Montreal, Quebec, Canada). Because the Na+ channel is made up of three subunits, [alpha], [beta], and [gamma], we also attempted to hybridize for [gamma]ENaC. However, we could not detect any significant signals for [gamma]ENaC with our probe. Transcripts were visualized by standard PhosphorImaging and autoradiography. RNA integrity and comparable RNA loading between lanes were assessed by hybridization of membranes with a complementary DNA probe for mouse 18S ribosomal RNA. After normalizing the expression with 18S ribosomal RNA, the relative expression for each probe ([alpha]ENaC, [beta]ENaC, [alpha]^sub 1^Na^sup +^-K^sup +^-ATPase, or [beta]^sub 1^Na^sup +^-K^sup +^-ATPase) was calculated by comparing specific densitometric signals of left lung mRNA with corresponding right lung mRNA in each experiment. The data are presented as percent expression of the right lungs: specifically, in the control animals (thoracotomy alone), the expression of the left lung was compared with that of the right lung; in transplanted animals, the left transplanted lung was compared with the right native lung.
For Western blotting, frozen lung tissue was solubilized in 60 [mu]l of lysate solution (250 mM sucrose, 10 mM tris(hydroxymethyl)amino-methane-hydrochloric acid, pH 7.4, 1 mM ethyleneglycol-bis-([beta]-amino-ethyl ether)-N,N'-tetraacetic acid, 0.5% vol/vol Triton X-100, 1 mM o-phenylmethylsulfonyl fluoride and 25 [mu]g/ml leupeptin) for 30 minutes on ice. The protein concentration was evaluated by the Bradford method (25) with the Pierce reagent (Rockford, IL, USA). Fifty micrograms of total protein were subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis and transferred electrophoretically on a Bio-Rad poly(vinylidene difluoride) membrane (Bio-Rad, Hercules,CA, USA). The membranes were blocked for 16 hours at 4[degrees]C with 5% wt/vol skimmed milk in phosphate-buffered saline Tween buffer (137 mM NaCl, 2.7 mM KCl, 1.5 mM potassium phosphate, 8.1 mM sodium phosphate, 0.05% vol/vol Tween 20, and 0.02% Thimerosal) before incubation in the same buffer for 16 hours at 4[degrees]C with a 1/1,000 dilution of a polyclonal antibody directed against the N-terminal portion of the rat [beta]ENaC subunit (26). After incubation for 2 hours at room temperature with 1/4,000 dilution of a horeseradish peroxidase-linked secondary antibody (Cells Signaling Technology, Beverly, MA) in 5% skimmed milk phosphate-buffered saline Tween, the band was detected by enhanced chemiluminescence (Amersham Biosciences, Piscataway, NJ) on Kodak X-K1 film. For quantification, the X-ray films were scanned on a HP ScanJet scanner and the bands quantified, using NIH ImageJ software. The Western blots were repeated four times (n = 4) from lysates extracted from the lungs [(left lung (transplanted) and right lung (native lung)] of four different animals.
Pulmonary MPO Measurements
A MPO assay was performed on lung tissue samples to quantify neutrophil sequestration (27). A section of previously frozen tissue was weighed and homogenized in 0.5% hexadecyltrimethylainmonium bromide (Sigma Chemical Co.) in 50 mM potassium phosphate buffer at pH 6.0 on ice. The homogenate was centrifugea at 37,000 x g for 20 minutes at 4[degrees]C, the supernatant decanted, and the pellet weighed and resuspended in hexadecyltrimethylammonium bromide. The pellet-hexadecyltrimethylammonium bromide suspension was freeze-thawed three times, followed by repeated sonications. The lung suspension was centrifuged at 37,000 x g for 20 minutes at 47deg;C, and the supernatant collected. MPO activity in the supernatant was assayed by a standard spectrophotometric technique.
Gravimetric Measurements
After homogenizing 2 g of lung parenchyma, we measured the wet-to-dry lung weight ratio (g water/g dry lung) adjusted for lung hemoglobin concentration, according to a previously described method (13).
Histologic Examination
To evaluate the histologic changes associated with lung transplantation, we performed additional left lung transplantations with a total of 8 hours of reperfusion. A small wedge lung biopsy was obtained before pulmonary flushing from the right lower lobe of the donor lung, and after 4 and 8 hours of reperfusion post-transplantation from the lingula and left lower lobe of the transplanted lung, respectively. Immediately after biopsy, the tissues were divided into halves that were fixed by direct needle injection with a tuberculin syringe of either 10% buffered formalin for light microscopy, or 1% glutarylaldehyde and 4% paraformaldehyde at pH 7.4 for electron microscopy, followed by immersion in the corresponding fixative solutions. For light microscopy, the tissues were processed by routine histologic techniques, embedded in paraffin, sectioned at 5 [mu]m, and stained with hematoxylin and eosin (H&E). For electron microscopy, the tissues were embedded in Epon resin; semi-thin sections (1 [mu]m) were cut with glass knives and stained with toluidine blue; thin sections (silver-gold) were cut with diamond knives, stained with uranyl acetate, and examined by electron microscopy, specifically for areas with alveolar tissue and type II pneumocytes.
Statistical Analyses
All results are expressed as means + or - standard error of the means. Means within the same experimental group were compared by Student's paired t test, and means between two groups, by Student's unpaired t test. In vivo ALC and pulmonary edema liquid-to-plasma total protein concentration ratio data were analyzed by linear regression to determine whether there was a significant change in clearance and ratios with time. Physiological parameters between control and transplanted groups were compared by analysis of variance for repeated measures. PhosphorImager readings of the mRNAs of interest were adjusted for corresponding 18S ribosomal RNA readings. Differences with a p value less than 0.05 were regarded as statistically significant.
RESULTS
Physiological Parameters During Reperfusion
The mean arterial pressure, mean pulmonary arterial pressure, heart rate, and pH data before surgery and for 4 hours posttransplantation are shown in Table 1. During the 4 hours of monitoring, there were no clinically significant differences in mean arterial pressure, mean pulmonary arterial pressure, heart rate, and pH between control and transplanted animals except for a transient fall in mean arterial pressure immediately after reperfusion. Data on the arterial PO^sub 2^ to inspired O2 fraction ratio (Pa^sub o^sub 2^^/FI^sub o^sub 2^^), used to evaluate oxygenation before surgery and for 4 hours of the monitoring period, are presented in Figure 1. During the monitoring period, no significant changes in Pa^sub o^sub 2^^/FI^sub o^sub 2^^ were evident in control animals (thoracotomy only), whereas transplanted animals showed a gradual and significant decrease in Pa^sub o^sub 2^^/FI^sub o^sub 2^^ for the 4 hours of monitoring.
Wet-to-Dry Lung Weight Ratio and MPO Activity
A significant increase was noted in the wet-to-dry lung ratio of the left transplanted lungs after 4-hour reperfusion, but not of the right native lungs of transplanted animals or the left or right lungs of the control animals (thoracotomy only) (Figure 2A). Similarly, MPO activity was significantly elevated in left transplanted pulmonary tissue, with no rise in animals following left-sided thoracotomy alone (Figure 2B).
Comparable increases were observed in the wet-to-dry lung weight ratios of left transplanted lungs and in MPO activity of four animals followed for 8 hours post-transplantation (Figures 3A and 3B).
ALC
ALC was identical in the right and left lungs of control animals (thoracolomy alone) (right: 20.0 + or - 0.8% vs. left: 22.6 + or - 2.0%). Terbutaline nearly doubled ALC in both the right and left lungs of the control animals (right: 35.5 + or - 5.0%, left: 36.6 + or - 2.6%) (Figure 4A). After 4 hours of reperfusion after transplantation, basal and stimulated ALC of the right native lungs was at the same level as in the lungs of control animals (20.9 + or - 5.5% and 33.2 + or - 6.8%, respectively). There was a significant decrease of ALC in left transplanted lungs compared with right native lungs (13.5 + or - 4.2%, p
To evaluate the potential role of the pulmonary circulation in reducing ALC measured in nonperfused lobe preparations, we measured ALC in vivo. In the control animals, ALC was significantly increased (r^sup 2^ = 0.41, p
The pulmonary edema liquid-to-plasma total protein concentration ratio rose gradually in the control animals over 4 hours (r^sup 2^ = 0.59, p
ENaC and Na+-K+-ATPase Expression During 4- and 8-Hour Monitoring
Left-sided thoracotomy followed by 4 hours of monitoring did not affect the expression levels of [alpha]ENaC, [beta]ENaC, [alpha]^sub 1^Na+-K+ATPase, and [beta]^sub 1^Na+-K+-ATPase mRNA in the left lungs of control animals (Figures 7A and 7B). In contrast, [alpha]ENaC and [beta]ENaC expression decreased significantly (-75% and -50%, respectively) in left transplanted lungs after 4 hours of reperfusion (Figure 7A). However, there were no significant changes in [alpha]^sub 1^Na+-K+-ATPase and [beta]^sub 1^Na+-K+-ATPase mRNA expression levels in transplanted lungs (Figure 7B). A similar pattern of [alpha]ENaC, [beta]ENaC, [alpha]^sub 1^Na+-K+-ATPase, and [beta]^sub 1^Na'-K+-ATPase expression was observed after 8 hours of post-transplantation reperfusion (Figures 8A and 8B). To confirm that the decrease in [alpha]ENaC mRNA led also to a decline in protein expression, we measured the level of [alpha]ENaC protein in the transplanted lung. Our results show that there was a 75% reduction of [alpha]ENaC in transplanted lungs (Figure 9).
Histology
Histologic examination of hematoxylin and eosin-stained sections revealed the presence of small numbers of neutrophils in the alveolar spaces and interstitium after 4 hours of reperfusion, with mild to moderate interstitial and focal alveolar edema (Figures 10A and 10B), compared with control lungs that were completely normal (Figures 11A and 11B). After 8 hours, there were substantially more numerous neutrophils as well as multiple areas of both interstitial and alveolar edema (Figures 12A and 12B). However, no obvious changes in the morphology of alveolar-capillary barrier cells were observed by light or electron microscopies. In particular, alveolar type II pneumocytes were not significantly altered (Figures 10C, 11C, and 12C).
DISCUSSION
This study demonstrates that ALC is significantly decreased in transplanted lungs in association with a significant increase in the wet-to-dry ratio, histologic evidence of interstitial and alveolar edema and neutrophil accumulation in the lungs. Moreover, the [beta]-adrenergic agonist terbutaline did not stimulate ALC in transplanted lungs. In parallel with this dysfunction of the alveolar liquid transport system after lung transplantation, we also observed a decrease in pulmonary ENaC expression.
Severe ischemia-reperfusion lung injury causing noncardiogenic edema reportedly occurs in 15 to 22% of lung transplantation recipients, resulting in increased mortality and morbidity (3, 28). Although the exact pathogenesis of this injury remains unclear, it is considered to be mediated by various mechanisms, including neutrophil adhesion and transendothelial migration with the release of proinflammatory mediators, cytokines, and reactive oxygen species (29, 30). The primary target of ischemia-reperfusion injury has been considered to be the enclothclium, causing increased microvascular permeability (31). However, recent experimental and clinical data suggest that dysfunction of the alveolar epithelium might also play a significant role in the severity of lung injury (16). Indeed, a recent clinical study of alveolar epithelial liquid transport after lung transplantation suggested that measurements of ALC are valuable in the clinical settings to evaluate alveolar epithelial transport function and predict outcome in patients with reperfusion injury after lung transplantation (11). Therefore, it appears important to explore the integrity of the alveolar epithelium, especially ALC in the post-transplantation period.
Our results showed a significant reduction in ALC in transplanted lungs compared with right native lungs after 4 hours of reperfusion. In contrast, ALC levels in right native lungs were similar to those found in control animals undergoing only a thoracotomy. These results are novel because there are no previous experimental data exploring the ALC capacity of transplanted lungs. We addressed this question in ex vivo nonperfused lung preparations to evaluate clearance in transplanted as well as in right native lungs of the same animals. This approach also enabled us to determine in the same animals if we could stimulate fluid clearance in the injured lungs with a [beta]-adrenergic agonist. We believed that this experimental method was valid, because it has been reported recently that ALC was identical between different lobes in the dog (20). We have shown that the decrease in ALC occurred only in transplanted and not in right native lungs. Because an increased wet-to-dry ratio and neutrophils accumulation are mainly observed in transplanted lungs, it is suggested that the reduction of clearance was related to local factors associated with the injury, and not to systemic circulating factors.
Could the decrease in ALC observed in our model be related to a greater level of injury than what one would expect after lung transplantation? This seems unlikely because the level of injury we observed is similar to that reported by others in canine lung transplantation models. Depending on the model and on the duration of reperfusion, it has been shown that the wet-to-dry ratio can increase between 6 and 14 (32-35), which is similar to what we measured. Furthermore, the level of neutrophil accumulation in transplanted lungs (2.1 times higher than in control lungs) is also similar to that reported by Yamashita and colleagues (36). Histologic examination also demonstrated that our model produced a moderate level of lung injury. Although we can clearly observe by light microscopy the presence of pulmonary edema after reperfusion, electron microscopic examination did not reveal any significant morphological changes in alveolar epithelial cells. Thus, we believe that we have created moderate injury. This level of injury might seem high considering the short ischmie time (193 minutes) before transplantation. However, it is important to note that we did not try to decrease the injury by adding pharmacological agents, like prostaglandins, or by using other types of flushing solutions known to decrease ischemia-reperfusion injury (37). Thus, our data are consistent with the notion that moderate injury to transplanted lungs leads to reduced ALC.
Before attributing these results directly to transplantation, we had to consider that the altered clearance could be related to factors other than transplantation. According to a recent paper, halothane and isoflurane reduce ALC in rats (21). Thus, we decided to determine if the anesthesia or thoracotomy could potentially explain our results: we performed experiments in a control group anesthetized and thoracotomized in a similar manner as the transplanted animals. After thoracotomy, these control animals were monitored for 4 hours like the transplanted animals, and ALC was measured in the right and left lungs. We found that ALC in them was similar to that in the right native lungs of transplanted animals. Furthermore, our data were similar to those reported in normal dog lungs and in resected human lungs under baseline and terbutaline-stimulated conditions (19, 20, 38). Therefore, it is unlikely that the decreased clearance that we observed after transplantation is related to thoracotomy or anesthesia.
Another potential weakness of our ex vivo model was the absence of the pulmonary circulation. Indeed, although it has been shown that the presence of the pulmonary circulation does not affect ALC in normal canine lungs (20), very little is known about its role in injured lungs. Fukuda and colleagues (24) recently suggested that interstitial fluid accumulation slows ALC in the absence of the pulmonary circulation and ventilation. Because the transplanted lungs after 4 hours of reperfusion were already edematous in our experiments, interstitial edema could explain the significant decrease of ALC in our ex vivo studies. Therefore, we measured ALC in vivo in the presence of the pulmonary circulation, and observed a progressive increase in ALC in the lungs of control animals over 4 hours; at that time, the ALC measured in the in vivo model was identical to that in the ex vivo model (22.6%). These results confirmed that the pulmonary circulation does not influence ALC in normal lungs. Although the ALC measured in transplanted lungs of the in vivo model (14.0%) was not identical to the ex vivo preparation (-18.94%), they both convey the same information. In the ex vivo preparation, we saw a decrease of ALC in transplanted lungs, whereas in the in vivo model, there was either a total absence of liquid clearance or even potentially an influx of edema fluid in the alveolar space. The difference between these results could be attributed to the fact that the injury was still progressing in the in vivo model, because the lungs were still perfused by the pulmonary circulation. In contrast, the progression of injury was slower in the ex vivo preparations, because there was no pulmonary circulation. In fact, we noticed a significant increase in the wet-to-dry ratio in the in vivo model (12.0 + or - 1.0) compared with the ex vivo preparations (7.6 + or - 0.7). Interestingly, we were also able to show that the pulmonary edema liquid-to-plasma total protein concentration ratio, used clinically as an index of alveolar-capillary barrier integrity, provided information similar to the more classical way of measuring ALC. Overall, these results suggest a significant reduction in ALC in the transplanted lung in both in vivo and ex vivo models, indicating that this decrease was not related to the model.
Although no previous work has evaluated ALC in transplanted lungs, some investigators have examined it in models of hypothermia or ischemia-reperfusion. Sakuma and colleagues (39) have shown that gradual rewarming of human lungs after severe hypothermia does not decrease ALC, unlike hypothermia. Furthermore, the same group reported that ALC was also preserved in a model of ischemia-reperfusion without flushing of the pulmonary circulation (41). Our model is quite different. We flushed the pulmonary circulation of the donor lungs with a cold preservation solution followed by hypothermic preservation in ice for a total ischemic period of 3 hours, and we then performed left lung transplantation. In our model, which closely mimics the clinical process, we found significant alterations of alveolar liquid transport. The differences in these results suggest that pulmonary flushing with cold preservation solution and reimplantation might have a significant impact on the functional ability of the epithelium to transport liquid. Indeed, pulmonary flushing with preservation solution alone has been reported to decrease ALC ability, and this change is accompanied by reduced transalveolar Na+ transport ability (40, 41). Another important factor that seems to influence ALC during preservation is the degree of inflation. In fact, Sakuma and colleagues (12) have shown that lung volume, more than hypothermia, might affect ALC after preservation. Although we kept the donor lungs inflated during preservation, which prevents a decrease in ALC during hypothermie preservation, they had to be deflated at the time of reimplantation, and it is possible that this also influenced the response. Finally, it is possible that the decrease in ALC is related to increased permeability of the epithelial barrier. In many lung injury models where an increase in epithelial permeability is observed, there is a decline of ALC (42, 43). Although we did not directly measure alveolar permeability in our model, it has been shown in the past that ischemia-reperfusion injury can lead to a change in epithelial permeability(11, 44). Further studies are needed to determine the effects of pulmonary flushing with cold preservation solution, inflation, and deflation, in combination with ischemia-reperfusion on epithelial permeability and ALC in transplanted lungs.
[beta]-Adrenergic stimulation is known to enhance transalveolar Na+ and liquid transport in normal and mildly injured lungs (13, 15, 45, 46). However, we observed no increase of ALC in transplanted lungs after stimulation with the [beta]-adrenergic agonist terbutaline, although it significantly augmented ALC in the control animals and in the right native lungs of transplanted animals. Because it is known that high levels of circulating catecholamine can inhibit the increase in ALC induced by [beta]-adrenergic agonists (47), one could hypothesize that the lack of response to such agonists in the transplanted lung could be related to endogenous circulating catecholamines. However, if this mechanism is responsible for the lack of response to terbutaline in transplanted lungs, we should have seen a similar response in the right native lungs of transplanted animals exposed to the same level of endogenous catecholamines. In contrast, baseline ALC of the right native lungs in transplanted animals remained similar to that in the control animals. Furthermore, the right native lungs of transplanted animals responded normally to terbutaline stimulation. Therefore, it is unlikely that the failure to respond to terbutaline was caused by elevated endogenous catecholamines. Another possibility is that ischemia-reperfusion injury is associated with [beta]-adrenergic receptor dysfunction. Disturbances in ALC following terbutaline stimulation have been reported in another model of neutrophil-dependent oxidant injury to the alveolar epithelium (48). Because the large increase of lung MPO activity in transplanted lungs in our study indicates significant neutrophil accumulation, neutrophil-dependent oxidant injury could explain the lack of stimulation of ALC. These results are different from those of Ware and colleagues (49) who showed that the [beta]-adrenergic response was normal in lungs that have been preserved but not used for transplantation. However, there is a major difference between the two experimental conditions. Although the human lungs used in their experiments were submitted to cold preservation and gradual rewarming, they were never exposed to pulmonary preservation solutions and reperfusion. Overall, these results suggest that the dysfunction to the [beta]-adrenergic agonist is more likely related to the ischemia-reperfusion injury rather than the preservation technique. Further studies, however, are needed to elucidate this question.
Although these experiments were not designed to evaluate in detail the mechanism that could alter ALC in the transplanted lung, we nevertheless performed exploratory experiments to investigate potential pathways. We examined the expression levels of [alpha] and [beta] ENaC and [alpha]^sub 1^ and [beta]^sub 1^Na+-K+-ATPase because they are the principal molecules involved in Na+ transport, the most important mechanism responsible for ALC (16). The expression levels of both [alpha] and [beta]ENaC mRNA were significantly decreased in transplanted lungs after 4 and 8 hours of reperfusion. It can be hypothesized that this lowered [alpha]ENaC mRNA expression might have contributed to the reduced ability of the alveolar epithelium to eliminate liquid. This hypothesis is plausible because mice deficient in the [alpha]ENaC gene alone die within 40 hours after birth due to their inability to clear lung liquid (50). Furthermore, adult transgenic rescue mice, which express a lower level of [alpha]ENaC, have been shown to have a lower sodium transport capacity especially after hypoxia (51) and to be more susceptible to pulmonary edema (52). The decrease in [beta]ENaC mRNA expression might also have caused functional alterations because both [beta] and [gamma]ENaC mRNA expression levels have been found to potentiate amiloride-sensitive Na+ currents (53). However, a change in mRNA expression is not necessarily associated with a change in protein expression or function. We explored this question by performing Western blot analysis of the transplanted lung using a polyclonal antibody against ENaC (26). The results reveal that the reduction of ENaC mRNA expression is associated with decreased protein expression. Nevertheless, further experiments will be necessary to clearly establish a link between the changes in ENaC expression and edema susceptibility because it has also been shown in a bleomycin lung injury model that lung liquid clearance can be stimulated when there is a fall in ENaC mRNA in the lung (54). Even if the modulation of ENaC expression is not associated with the decrease in ALC it is likely to be important in the injury process because it has been observed in two other models of lung injury. In viral pneumonia (55) and bleomycin-induced lung injury (54), ENaC mRNA expression falls in the injured lung. However, the demonstration of a decreased ENaC protein expression in the injured transplanted lung is novel. Overall, the reduction of ENaC expression in the injured lung surely merits further exploration.
Other molecules modulating Na+ transport in alveolar epithelial cells could also be important in lung injury. It has been well-documented that lung injury affect the expression and function of alveolar epithelial Na+-K+-ATPase (16, 17, 56). Recently, Kim and colleagues (57) reported that ischemia-reperfusion injury resulted in initial upregulation of Na+-K+-ATPase mRNAs after 12 hours of preservation and 20 minutes of reperfusion in a rat model. In our canine model, however, there were no significant changes in the expression of either [alpha]^sub 1^ or [beta]^sub 1^Na+-K+-ATPase mRNA in transplanted lungs compared with right native lungs after reperfusion. These two experimental models were different not only in the animal species studied but also in the duration of the reperfusion period. These differences in the experimental protocol might explain the difference in the data. However, the lack of decrease in Na+-K+-ATPase mRNA expression does not necessarily mean that there is no Na+-K+-ATPase dysfunction in transplanted lungs because there could be abnormal regulation of the membrane trafficking of the Na+ pump that could lead to dysfunction of the pump (56). Further studies will be needed to evaluate if lung transplantation can lead to a dysfunction of Na+-K+-ATPase. Moreover, because it has been shown that supplementation of Na+-K+-ATPase by gene therapy can decrease the severity of lung injury (58, 59), one might consider this approach in lung transplantation to decrease edema formation.
In summary, we demonstrated that lung injury caused by lung transplantation is associated with decreased ALC. There is also significantly reduced ENaC mRNA expression in transplanted lungs. Further studies will determine if the decreased clearance seen in transplanted lungs is related to lower ENaC expression or potentially to a dysfunction of Na+-K+-ATPase.
Acknowledgment: The authors thank Ms. E. Dedelis and Ms. N. Rousseau for their invaluable help with the surgical preparation of the animals, Ms. M. Masluch for her expert technical assistance in electron microscopy, and Mr. O. Da Silva for editing this manuscript.
References
1. Keller CA. The donor lung: conservation of a precious resource. Thorax 1998;53:506-513.
2. Hosenpud JD, Bennett LE, Keck BM, Boucek MM, Novick RJ. The Registry of the International Society for Heart and Lung Transplantation: eighteenth Official Report-2001. J Heart Lung Transplant 2001; 20:805-815.
3. Christie JD, Bavaria JE, Palevsky HI, Litzky L, Blumenthal NP, Kaiser LR, Kotloff RM. Primary graft failure following lung transplantation. Chest 1998:114:51-60.
4. Sakuma T, Takahashi K, Ohya N, Kajikawa O, Martin TR, Albertine KH, Matthay MA. Ischemia-reperfusion lung injury in rabbits: mechanisms of injury and protection. Am J Physiol 1999;276:L137-L145.
5. Matthay MA, Wiener-Kronish JP. Intact epithelial barrier function is critical for the resolution of alveolar edema in humans. Am Rev Respir Dis 1990:142:1250-1257.
6. Ware LB, Matthay MA. Alveolar fluid clearance is impaired in the majority of patients with acute lung injury and the acute respiratory distress syndrome. Am J Respir Crit Care Med 2001;163:1376-1383.
7. Saumon G, Basset G. Electrolyte and fluid transport across the mature alveolar epithelium. J Appl Physiol 1993;74:1-15.
8. Matalon S. Mechanisms and regulation of ion transport in adult mammalian alveolar type II pneumocytes. Am J Physiol 1991;261:C727-C738.
9. O'Brodovich HM. The role of active Na+ transport by lung epithelium in the clearance of airspace fluid. New Horiz 1995;3:240-247.
10. Matthay MA, Folkesson HG, Verkman AS. Salt and water transport across alveolar and distal airway epithelia in the adult lung. Am J Physiol 1996;270:L487-L503.
11. Ware LB, Golden JA, Finkbeiner WE, Matthay MA. Alveolar epithelial fluid transport capacity in reperfusion lung injury after lung transplantation. Am J Respir Crit Care Med 1999;159:980-988.
12. Sakuma T, Tsukano C, Ishigaki M, Nambu Y, Osanai K, Toga H, Takahashi K, Ohya N, Kurihara T, Nishio M, et al. Lung deflation impairs alveolar epithelial fluid transport in ischemic rabbit and rat lungs. Transplantation 2000;69:1785-1793.
13. Berthiaume Y, Staub NC, Matthay MA. Beta-adrenergic agonists increase lung liquid clearance in anaesthetized sheep. J Clin Invest 1987; 79:335-343.
14. Frank JA, Wang Y, Osorio O, Matthay MA. Beta-adrcnergic agonist therapy accelerates the resolution of hydrostatic pulmonary edema in sheep and rats. J Appl Physiol 2000;89:1255-1265.
15. Azzam ZS, Saldias FJ, Cornelias A, Ridge KM, Rutschman DH, Sznajder JI. Catecholamines increase lung edema clearance in rats with increased left atrial pressure. J Appl Physiol 2001;90:1088-1094.
16. Berthiaume Y, Lesur O, Dagenais A. Treatment of adult respiratory distress syndrome: plea for rescue therapy of the alveolar epithelium. Thorax 1999;54:150-160.
17. Berthiaume Y, Folkesson HG, Matthay MA. Lung edema clearance: 20 years of progress: invited review: alveolar edema fluid clearance in the injured lung. J Appl Physiol 2002;93:2207-2213.
18. Matthay MA, Clerici C, Saumon G. Invited review: active fluid clearance from the distal air spaces of the lung. J Appl Physiol 2002;93:1533-1541.
19. Berthiaume Y, Broaddus VC, Gropper MA, Tanita T, Matthay MA. Alveolar liquid and protein clearance from normal dog lungs. J Appl Physiol 1988;65:585-593.
20. Grimme JD, Lane SM, Maron MB. Alveolar liquid clearance in multiple nonperfused canine lung lobes. J Appl Physiol 1997;82:348-353.
21. Rezaiguia-Delclaux S, Jayr C, Luo DF, Saidi NE, Meignan M, Duvaldestin P. Halothane and isoflurane decrease alveolar epithelial fluid clearance in rats. Anesthesiology 1998;88:751-760.
22. Doumas BT, Bayse DD, Carter RJ, Peters T Jr, Schaffer R. A candidate reference method for determination of total protien in scrum: development and validation. Clin Chem 1981;27:1642-1650.
23. Rezaiguia S, Garat C, Delclaux C, Meignan M, Fleury J, Legrand P, Matthay MA, Jayr C. Acute bacterial pneumonia in rats increases alveolar epithelial fluid clearance by a tumor necrosis factor-alpha-dependent mechanism. J Clin Invest 1997;99:325-335.
24. Fukuda N, Folkesson HG, Matthay MA. Relationship of interstitial fluid volume to alveolar fluid clearance in mice: ventilated vs. in situ studies. J Appl Physiol 2000:89:672-679.
25. Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 1976;72:248-254.
26. Johnson MD, Widdicombe JH, Allen L, Barbry P, Dobbs LG. Alveolar epithelial type I cells contain transport proteins and transport sodium, supporting an active role for type I cells in regulation of lung liquid homeostasis. Proc Natl Acad Sci USA 2002;99:1966-1971.
27. Goldblum SE, Wu KM, Jay M. Lung myeloperoxidase as a measure of pulmonary leukostasis in rabbits. J Appl Physiol 1985:59:1978-1985.
28. King RC, Binns OA, Rodriguez F, Kanithanon RC, Daniel TM, Spotnitz WD, Tribble CG, Kron IL. Reperfusion injury significantly impacts clinical outcome after pulmonary transplantation. Ann Thorac Surg 2000;69:1681-1685.
29. Khan SU, Salloum J, O'Donovan PB, Mascha EJ, Mehta AC, Matthay MA, Arroliga AC. Acute pulmonary edema after lung transplantation: the pulmonary reimplantation response. Chest 1999;116:187-194.
30. Kelly RF. Current strategics in lung preservation. J Lab Clin Med 2000; 136:427-440.
31. Hidalgo MA, Shah KA, Fuller BJ, Green CJ. Cold ischemia-induced damage to vascular endothelium results in permeability alterations in transplanted lungs. J Thorac Cardiovasc Surg 1996;112:1027-1035. 32. Bryan CL, Patefield AJ, Cohen D, Nielsen JL, Emanuel B, Calhoon JH. Assessment of injury in transplanted and nontransplanted lungs after 6 h of cold storage with glutathione. J Appl Physiol 1994;76:1232-1241.
33. Bryan CL, Cohen DJ, Dew JA, Trinkle JK, Jenkinson SG. Glutathione decreases the pulmonary reimplantation response in canine lung autotransplants. Chest 1991;100:1694-1702.
34. Lin PJ, Hsieh MJ, Cheng KS, Kuo TT, Chang CH. University of Wisconsin solution extends lung preservation after prostaglandin El infusion. Chest 1994;105:255-261.
35. Aoe M, Okabayashi K, Cooper JD, Patterson GA. Hyperinflation of canine lung allografts during storage increases reperfusion pulmonary edema. J Thorac Cardlovasc Surg 1996:112:94-102.
36. Yamashita M, Schmid RA, Okabayashi K, Ando K, Kobayashi J, Cooper JD, Patterson GA. Pentoxifyllinc in flush solution improves early lung allograft function. Ann Thorac Surg 1996;61:1055-1061.
37. Novick RJ, Gehman KE, Ali IS, Lee J. Lung preservation: the importance of endothelial and alveolar type 11 cell integrity. Ann Thorac Surg 1996;62:302-314.
38. Sakuma T, Okaniwa G, Nakada T, Nishimura T, Fujimura S, Matthay MA. Alveolar fluid clearance in the resected human lung. Am J Respir Crit Care Med 1994;150:305-310.
39. Sakuma T, Suzuki S, Usuda K, Handa M, Okaniwa G, Nakada T, Fujimura S, Matthay MA. Preservation of alveolar epithelial fluid transport mechanisms in rewarmed human lung after severe hypothermia, J Appl Physiol 1996;80:1681-1686.
40. Sugita M, Suzuki S, Kondo T, Noda M, Fujimura S. Transalveolar fluid absorption ability in rat lungs preserved with euro-collins solution and EP4 solution. Transplantation 1999;67:349-354.
41. Sugita M, Suzuki S, Fujimura S, Kondo K, Saito R, Matsumura Y, Sado T, Tanita T, Sakuma T, Handa M. Effects of flushing temperature and preservation solution on alveolar fluid clearance in the preserved rat lungs. Transplant Proc 1997;29:1354-1356.
42. Modelska K, Pittet JF, Folkesson HG, Broaddus VC, Matthay MA. Acid-induced lung injury: protective effect of anti-interleukin-8 pretreatment on alveolar epithelial barrier function in rabbits. Am J Respir Crit Care Med 1999;160:1450-1456.
43. Laffon M, Pittet JF, Modelska K, Matthay MA, Young DM. Interleukin-8 mediates injury from smoke inhalation to both the lung endothelial and the alveolar epithelial barriers in rabbits. Am J Respir Crit Care Med 1999;160:1443-1449.
44. Khimenko PL, Barnard JW, Moore TM, Wilson PS, Ballard ST, Taylor AE. Vascular permeability and epithelial transport effects on lung edema formation in ischemia and reperfusion. J Appl Physiol 1994: 77:1116-1121.
45. Garat C, Meignan M, Matthay MA, Luo DF, Jayr C. Alveolar epithelial fluid clearance mechanisms are intact after moderate hyperoxic lung injury in rats. Chest 1997;111:1381-1388.
46. Saldias FJ, Lecuona E, Cornelias AP, Ridge KM, Rutschman DH, Sznajder JI. Beta-adrenergic stimulation restores rat lung ability to clear edema in ventilator-associated lung injury. Am J Respir Crit Care Med 2000:162:282-287.
47. Morgan EE, Hodnichak CM, Stader SM, Macnder KC, Boja JW, Folkesson HG, Maron MB. Alveolar epithelial ion and fluid transport: prolonged isoprotcrcnol infusion impairs the ability of beta(2)-agonists to increase alveolar liquid clearance. Am J Physiol 2002;282:L666-L674.
48. Modelska K, Matthay MA, Brown AS, Deutch E, Lu LN, Pittet JF. Inhibition of [beta]-adrenergic-dependent alveolar epithelial clearance by oxidant mechanisms after hemorrhagic shock. Am J Physiol 1999;276: L844-L857.
49. Ware LB, Fang X, Wang Y, Sakuma T, Hall TS, Matthay MA. Selected contribution: mechanisms that may stimulate the resolution of alveolar edema in the transplanted human lung. J Appl Physiol 2002;93: 1869-1874.
50. Hummler E, Barker P, Gatzy J, Beermann F, Verdumo C, Schmidt A, Boucher R, Rossier BC. Early death due to defective neonatal lung liquid clearance in [alpha]ENaC-deficient mice. Nat Genet 1996;12:325-328.
51. Olivier R, Scherrer U, Horisberger JD, Rossier BC, Hummler E. Selected contribution: limiting Na(+) transport rate in airway epithelia from alpha-ENaC transgenic mice: a model for pulmonary edema. J Appl Physiol 2002;93:1881-1887.
52. Egli M, Sartori C, Duplain H, Lepori M, Hummler E, Nicod P, Rossier BC, Scherrer U. Impaired alveolar fluid clearance and augmented susceptibility to lung edema in mice with defective amiloride-sensitive sodium transport [abstract]. FASEB J 2000;14:127.
53. Canessa CM, Schild L, Buell G, Thorens B, Gautschi I, Horisberger JD, Rossier BC. Amiloride-sensitive epithelial Na+ channel is made of three homologous subunits. Nature 1994;367:463-467.
54. Folkesson HG, Nitenberg G, Oliver BL, Jayr C, Albertine KH, Matthay MA. Upregulation of alveolar epithelial fluid transport after subacute lung injury in rats from bleomycin. Am J Physiol 1998;275:L478-L490.
55. Towne JE, Harrod KS, Krane CM, Menon AG. Decreased expression of aquaporin (AQP)1 and AQP5 in mouse lung after acute viral infection. Am J Respir Cell Mol Biol 2000;22:34-44.
56. Sznajder JI, Factor P, Ingbar DH. Invited review: lung edema clearance: role of Na(+)-K(+)-ATPase. J Appl Physiol 2002;93:1860-1866.
57. Kim JD, Baker CJ, Danto SI, Starnes VA, Barr ML. Modulation of pulmonary Na+ pump gene expression during cold storage and reperfusion. Transplantation 2000;70:1016-1020.
58. Factor P, Dumasius V, Saldias F, Brown LA, Sznajder JI. Adenovirus-mediated transfer of an Na+/K+-ATPase beta1 subunit gene improves alveolar fluid clearance and survival in hyperoxic rats. Hum Gene Ther 2000;11:2231-2242.
59. Stern M, Ulrich K, Robinson C, Copeland J, Griesenbach U, Masse C, Cheng S, Munkonge F, Geddes D, Berthiaume Y, et al. Pretreatment with cationic lipid-mediated transfer of the Na+K+ ATPase pump in a mouse model in vivo augments resolution of high permeability pulmonary edema. Gene Ther 2000;7:960-966.
Makoto Sugita, Pasquale Ferraro, Andre Dagenais, Marie-Eve Clermont, Pascal Barbry, Rene P. Michel, and Yves Berthiaume
Centre de Recherche, Centre hospitalier de l'Universite de Montreal, Hotel-Dieu; Departements de medecine et de chirurgie, Universite de Montreal; Department of Pathology, McGill University, Montreal, Quebec, Canada; CNRS/UNSA UMR 6097, IPMC, F-06560 Sophia-Antipolis, France
(Received in original form April 12, 2002; accepted in final form January 21, 2003)
Supported in part by grants from the Medical Research Council of Canada (MT-10273) and Fujisawa Canada, Inc. M.S. is the recipient of a Canadian Cystic Fibrosis Foundation/Medical Research Council of Canada fellowship. Y.B. is a Fonds de la recherche en Sante du Quebec scholar.
Correspondence and requests for reprints should be addressed to Dr. Yves Berthiaume, M.D., M.Sc, Centre de recherche, Hotel-Dieu du CHUM, 3850 St-Urbain, Montreal, Quebec H2W 1T7, Canada. E-mail: yves.berthiaume@umontreal.ca
Am J Respir Crit Care Med Vol 167. pp 1440-1450, 2003
Originally Published in Pressas DOI: 10.1164/rccm.200204-312OC on January 24, 2003
Internet address: www.atsjournals.org
Copyright American Thoracic Society May 15, 2003
Provided by ProQuest Information and Learning Company. All rights Reserved