Background: Hemodynamic assistance with a miniature intracardiac pump may fill the treatment gap between use of an intraaortic balloon pump (IABP) and the current, more invasive ventricular assist devices. The objective of this study was to compare the hemndynamic efficacy of a miniature intracardiac pump device with that of IABP.
Methods and results: Reversible acute mitral regurgitation (AMR) was induced in eight calves by stenting the mitral valve using a vena cava Filter. Full and partial AMR assist were compared with maximum IABP support in each animal. In full-support mode, both assist systems increased cardiac output (miniature intracardiac pump, 13% [p < 0.05]; IA_BP, 3% [p < 0.05]), mean aortic pressure (miniature intracardiac pump, 13% [p < 0.05]; IABP, 8% [p < 0.05]), carotid artery flow (miniature intracardiac pump, 29% [p < 0.05]; IABP, 5% [difference not significant]), and coronary blood flow (miniature intracardiac pump, 25% [difference not significant]; IABP, 34% [p < 0.05]). Again in full-support mode, both systems reduced left atrial pressure (miniature intracardiac pump, 2.4 mm Hg [p < 0.05]; IABP, 0.7 mm Hg [p < 0.05]), peak left ventricular (LV) pressure (miniature intracardiac pump, 13% [p < 0.05]; IABP, 5% [p < 0.05]), and external LV work (miniature intracardiac pump, 29% [p < 0.05]; IABP, 3% [p < 0.05]). Only full miniature intracardiac pump support reduced both end-diastolic LV volume (7%; p < 0.05) and end-systolic LV volume (10%; p < 0.05). IABP mainly improved coronary perfusion, while the miniature intracardiac pump proved more capable of genuinely unloading the LV.
Conclusions: We conclude that during severe acute LV failure, the miniature intracardiac pump is capable of more effective cardiac unloading and circulatory support than IABP.
(CHEST 2004; 126:896-902)
Key words: assist device; hemodynamics; intracolporeal circulation; shock; ventricular unloading
Abbreviations: AMR acute mitral regurgitation; CDO = conductance derived output; DCF = diastolic coronary flow fraction; EDV = end-diastolic left ventricular volume; ESV - end-systolic left ventricular volume; IABP intraaortic balloon pump; IMP = Impella miniature intracardiac pump; LAP = leti atrial pressure; LV = left ventricle, ventricular; LVW = external left ventricular work; PASC = ascending aortic pressure; PLVpeak = peak systolic left ventricular pressure; PP = pulse pressure; QAV = mean flow through the aortic valve; QCOR = coronary artery flow; QIMP = flow of the Impella miniature intracardiac pump; QPA pulmonary ariery flow; QR = regurgitant flow across mitral valve
**********
During the past 4 decades, the intraaortic balloon pump (IABP) has established itself as the standard mechanical cardiac assist option for treating patients who are in acute cardiogenic shock, (1-5) In search of more effective alternatives, new intravascular devices have been developed and used for cardiac support in postcardiotomy cardiogenic shock and during coronary artery bypass surgery. (6-9)
The Impella intracardiac microaxial pump (IMP) [Impella Cardiotechnik AG; Aachen, Germany] is a new, catheter-based cardiac assist device that is designed to provide ventricular support in bypass mode. Although the IMP has been introduced clinically recently, the hemodynamic efficacy has not yet been extensively evaluated. (10,11) In the present study, left ventricular (LV) support using the IMP and an IABP (System 98 XT; Datascope; Fairfield, NJ) were evaluated in an animal model of acute mitral regurgitation (AMR). (5)
MATERIALS AND METHODS
Animal Preparation
Eight calves (mean weight, 81 kg; range, 60 to 92 kg) were premedicated with atropine (0.05 mg/kg subcutaneously). Anesthesia was induced with sodium thiopental (20 mg/kg IV bolus) and was maintained with a 1:2 mixture of [O.sub.2]/[N.sub.2]O and halothane (1.5%). After the administration of analgesic: buprenorphine (0.01 mg/kg IV bolus) and the muscle relaxant suxamethonium (0.1 mg/kg IV bolus), a left thoracotomy was performed. The anticoagulation regimen was as follows: administration of heparin (200 IU/kg IV bolus); and monitoring by activated clotting time (> 400 s). Animals were killed by pentobarbital overdose (80 mg/kg IV bolus). All animals received humane care in compliance with the Guide for the Care arid Use of Laboratory Animals of the National Institutes of Health, and the study was approved by the Animal Ethical Committee at the University" of Maastricht.
Cardiac Support Systems
The IMP features an integrated cannula-pump assembly that is 6.4 mm in diameter and 100 mm in length, which is suitable for placement across the aortic valve. The axial impeller of the pump (ie, an Archimede screw) continuously recruits blood from the LV via the cannula and drains the blood into the aorta just above the aortic valve. The pump housing contains an integrated solid-state differential pressure sensor that registers the pressure gradient across the pump. The device is powered mad controlled by a pump console via a connecting catheter. The placement of the catheter pump occurs via percutaneous access or intraoperatively via aortic cannulation. The pump is designed for short-term to mid-term support (maximum duration, 7 days). (12,13)
The IMP was introduced via the left carotid artery and was placed across the aortic valve with the inflow cannula in the LV, and with the pump housing and outlet just above the aortic valve. Positioning was facilitated by the pressure gradient reading on the pump console.11,13 Routine checks with fluoroscopy confirmed the proper placement of the pump. Immediately after placement of the IMP, the pump rate was set to a minimum level that was sufficient to prevent aortic retrograde flow. The IMP console flow measurement was calibrated by the automated console calibration sequence after pump positioning.
A 40-mL intraaortic balloon catheter (Datascupe) was introduced via the right femoral artery and was placed in the high descending aorta. The IABP was triggered on the ECG.
Instrumentation
A Swan-Ganz thermodilution catheter (Arrow International; Reading, PA) was advanced into the pulmonary artery via a jugular vein. A conductance catheter, incorporating a pressure sensor (CD Leycom; Zoetermeer, the Netherlands), was positioned in the LV via the left femoral artery. The conductance catheter was connected to a conductance console (Sigma 5/DF; CD Leycom), which was used in the dual-frequency mode. (14) Solid-state pressure catheters (CD Leycom) were placed in the abdominal aorta via the left femoral artery and in the left atrium through a purse-string suture. BP in the aortic arch was measured via the lumen of the intraoortic balloon catheter with a standard pressure transducer (Baxter International Inc; Deerfield, IL). Ultrasonic flow probes (Transonic Systems; Ithaca, NY) were placed on the pulmonary artery, the right carotid artery, and on a side branch of the left anterior descending coronary artery. All hemodynamic data were acquired and stored using a 16-channel acquisition system (CD Leycom).
To induce AMR, an incision was made in the left atrium through which a retrievable steel wire cage (Gunther Tulip Vena Cava Filter; Cook Europe; Bjaeverskov, Denmark) was placed in the mitral valve. (5,9) The degree of AMR was assessed and controlled by the monitoring of real-time LV pressure and volume, and left atrial pressure (LAP). The induction of mitral regurgitation was consistently aimed at maximizing the regurgitant orifice.
Conductance Calibration
Parallel conductance was determined by injecting 7.5 mL 6.5% hypertonic saline solution into the pulmonary artery. (15) A 5-mL blood sample was collected in a sampling cuvette for blood resistivity measurement (CD Leycom). (16) The gain calibration factor was determined by comparing LV conductance-derived output (CDO) with pulmonary artery flow (QPA) in the healthy animal. The conductance data were analyzed with all appropriate software package (Circlab 2000; GTX Medical Software; Leiden, the Netherlands).
Measurements and Analysis
Both the IABP and the IMP were tested in each animal, in an alternated sequence in consecutive experiments. The 1ABP was driven in 1:1 mode and was tuned to maximize LV afterload reduction and diastolic aortic pressure augmentation. (1-3) The IMP was run at medium speed (24,000 revolutions per minute; performance level, P5) and full speed (33,000 revolutions per minute; performance level, P9). Approximately 10 s after the creation of mitral regurgitation, assist was initiated and maintained for 30 s.
The hemodynamic data were analyzed and processed to obtain objective measures for left heart pump function, myocardial working conditions, and peripheral perfusion. At baseline (ie, during calibration) the GDO (ie, stroke volume x heart rate) was set equal to the QPA, and the flow through the aortic valve (QAV) was considered to be equal to the QPA. During mitral regurgitation, the CDO expresses both the forward output (ie, the QAV) and the regurgitant flow across the (stented) mitral valve (QR), and thus CDO QAV + QR (in liters per minute). During IMP support, part of the QAV no longer occurs through the aortic valve but through the IMP, and QAV is calculated as QPA the flow of the IMP (QIMP). QAV is solely due to the contraction of the LV. QIMP is the flow measured through the IMP. The QPA is then the result of the combined effects of LV contraction and IMP aspiration.
Pulse pressure (PP) was calculated as the differential between the maximum and minimum values of ascending aortic pressure (PASC). The diastolic coronary flow fraction (DCF) was calculated as the ratio of antegrade diastolic coronary flow (QCOR) to the mean QCOR, multiplied by 100%. External LV work (LVW) was calculated as follows: (peak systolic LV pressure [PLVpeak] -LAP) x (QAV + QR) [in Joules per second). The QPA/LAP ratio was calculated as an index of left heart pump function. (17) A measure for the balance in coronary demand and supply was defined by the LVW/QCOR ratio (in Joules per milliliter). For each setting, the on condition (ie, AMR plus assist) and the off condition (ie, AMR plus assist idle) were compared by the application of the nonparametric Wilcoxon signed rank test (eight subjects). Significance was assumed if the p values were < 0.05.
RESULTS
Pump Characteristics
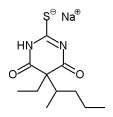
Figure 1 shows the performance of the IMP with measurements made in vivo. The measurements were performed during AMR and at four different performance levels. The pump flow values were taken from the flow reading of the console. Average pump flow has a linear relationship to the selected rotational speed and ranges from 1.9 to 4.2 L/min. The SD remains fairly constant at 0.5 L/min throughout the range.
[FIGURE 1 OMITTED]
Hemodynamic and Functional Effects
The effects of support on hemodynamics and cardiac function are summarized in Table 1. Only the IMP in P9 mode significantly reduced both end-diastolic LV volume (EDV) [by 7%] and end-systolic LV volume (ESV) [by 10%]. The IMP assist mode had a greater effect (reduction, 7 mm Hg) than the IABP assist mode (reduction, 3 mm Hg) on PLVpeak. Ascending aortic PP was significantly reduced by the IMP, with a maximum reduction of 6 mm Hg in P9 mode. In contrast, the IABP increased PP by 6 mm Hg. Mean carotid artery flow was augmented significantly only by the IMP (hemodynamics increase, 15%; cardiac function increase, 29%), while mean QCOR was enhanced significantly only by the IABP (increase, 34%). QPA was increased significantly by both the IABP (3%) and the IMP (P5 mode, 6%; P9 mode, 13%).
Figure 2 defines the various flow modes. The heights of the columns correspond with the mean values stated in Table 1. The IABP increased QAV by 3%, whereas the IMP reduced QAV by 38% in the P5 mode, and by 52% in the P9 mode (Table 1). Regurgitant flow through the mitral valve was reduced to some extent in the IMP P9 mode only (QR reduction, 15%; difference not significant). External LVW was significantly reduced only with full IMP support (LVW decrease in P9 mode, 29%). The index for left heart pump function (ie, QPA/LAP) significantly increased with assist (IMP: P5 mode, 21%; P9 mode, 41%; IABP, 7%) [Table 1]. In Figure 3, the effects on left heart pump function are further analyzed by incorporating the preassist hemodynamic condition in each individual. Preassist QPA values ranged from 2 to 12 L/min (ie, after the induction of mitral regurgitation). The trends indicate that support is more effective with lower preassist QPA values. The difference in effectiveness between the IABP and the IMP increases with the same trend. Table 1 also shows that the LVW/QCOR index decreased significantly in the 1:1 IABP mode (18%), and with the IMP in the P5 mode (20%) and the P9 mode (36%). Figure 4 focuses on the improvement in the balance of coronary demand and supply in each individual. (Note that a decrease in the LVW/QCOR ratio corresponds to an improvement in the coronary demand-supply balance.)
[FIGURES 2-4 OMITTED]
Hemodynamic Trends
Among the subjects who had a preassist cardiac output of < 4 L/min, pronounced effects on pump function and coronary balance were seen (Fig 3, 4). Figure 5 shows paired trends (obtained from one single animal) that are typical of the full LV bypass situation observed in these particular subjects. After switching on P9 mode IMP support, the PLVpeak progressed below even diastolic aortic pressure levels. Apparently, during systole there was no longer a forward pressure gradient and therefore no QAV (Fig 5).
[FIGURE 5 OMITTED]
Peak PASC and pulsatility are increased by the IABP. The IMP increases the mean PASC while it reduces pulsatility. The QCOR recordings showed that both pumps enhance the primarily diastolic QCOR. This observation was sustained by the results for DCF (Table 1).
DISCUSSION
Circulatory Support
The reduction of elevated LAPs, indicative of mitral regurgitation, implies that pulmonary venous congestion was suppressed, which ,nay counter the development or further progress of lung edema. Peripheral perfusion was significantly improved, which shows that both, assist systems provide circulatory support in the event of left heart failure (Table 1).
Cardiac Unloading
The reduction of LVW and oxygen consumption is an essential element of cardiac unloading and car dioprotective therapy. Afterload is a major determinant of myocardial work),is PLVpeak as a measure of LV afterload was reduced with use of the assist mode (Table 1). (19) In general, a suitable definition for LV pressure load would be PASC - LAP, (20) but this factor is prone to error in the ease of LV mid aortic pressure dissociation (Fig 5). Therefore, external LV pressure work was estimated as PLVpeak - LAP.
The IMP, in P9 mode, reduced both regurgitant valve flow (15%) and aortic valve flow (52%), as well as external LVW (29%) and LV volume (EDV, 7%; ESV, 10%). These data suggest that during full IMP support total LVW and myocardial oxygen consumption are reduced) (18,21,22) The IABP showed less effective unloading capabilities.
Myocardial Support
In general, myocardial function is supported by reducing myocardial work and augmenting coronary perfusion. The IMP improved coronary perfusion (QCOR increase, 25%) and strongly reduced cardiac workload (LVW decrease, 29%; PLVpeak decrease, i3%). (18) The IABP primarily improved coronary perfusion (QCOR increase, 34%) as work reduction was only marginal (LVW decrease, 3%; PLVpeak decrease, 5%). The coronary demand-supply balance was significantly improved (ie, LVW/QCOR ratio decreased) by both devices (Table 1), but the overall effectiveness of the IMP was greater than that of the IABP (Fig. 3). The LVW/QCOR ratio reflects both the ventricular unloading and coronary perfusion aspects. In clinical practice, the priority may lie with either one of these. If the priority lies with myocardial oxygen supply (ie, control of ischemia), the IABP remains an effective, well-proven tool for therapy. (23) When additional LV unloading and immediate circulatory support are mandatory, the IMP may present a solid alternative.
Impact of Preassist Condition
An analysis of the effect of support among individual subjects shows that functional improvements with assist are greater in weaker subjects (Fig 3, 4). In the P9 setting, the average IMP flow was 4.2 L/min (Fig 1). With preassist cardiac out-puts of > 8 L/min, a bypass flow of 4 L/min naturally has only limited impact. In individuals with insufficient cardiac output (ie, < 4 L/min), pump function improvement was more pronounced (IMP, > 100%; IABP, [less than or equal to] 25%) [Fig 3]. These trends and the data in Table 1 suggest that the IMP has greater effectiveness in improving overall pump function than the IABP. Figure 4 shows that the IABP partially compensates for its poor volume unloading performance by improving the coronary perfusion aspect. (1,5,9)
LV Output and IMP Output
Table 1 gives the values for QPA, QR, and QAV. Figure 2 provides a detailed overview of the LV and device-related contributions to forward cardiac output. Apparently, CDO is the sum of QB, QAV, and QIMP. The slight discrepancy found when calculating CDO from Table 1 is due to rounding errors (ie, EDV - ESV x HR [congruent to] 13.7 L/min, while QR + QAV + QIMP [congruent to] I4 L/min). Output analysis shows that part of the stroke volume ejected by the LV is via the IMP (ie, CDO contains QIMP) [Fig 2]. The QIMP is due to the simultaneous effect of LV contraction and IMP aspiration. Essentially, the IMP acts as an afterload reduction device that augments ventricular output toward the aorta, which effectively redistributes forward output and regurgitant flow. (The cumulative bar is lifted with respect to the zero output level in Fig 2.)
LVW was calculated from (PLVpeak- LAP) x (QAV + QR), which implies that the fraction of LV stroke output through the IMP does not contribute to external LVW. Realistically, this assumption may introduce some error. While both the LV and IMP work simultaneously, the exact share of pump and cardiac work cannot be identified.
Pulsatility
Whereas the IMP reduces the pulsatility in the aorta, the IABP increases PP (Fig 5 and Table 1). The evaluation of the quality of pulseless perfusion based solely on hemodynamic measurements is controversial and therefore was not addressed further. (24) Moreover, the present study is focused oil acute hemodynamic collapse, which renders the long-term pulseless perfusion effects less relevant. Interestingly, however, the IMP did not flatten the QCOR curve but exhibited a behavior comparable to that of the IABP during systole (Fig 5). The decreased systolic flow seen with use of the IABP can be attributed to the intentional aortic pressure reduction at end-diastole. The decrease in systolic flow with the IMP may be caused by a pressure decline due to an accelerated jet (ie, the Venturi effect) from the outflow of the IMP. (25)
Model
Other investigators (20) who tested a device similar to the IMP reported less promising results. In their bovine ischemic LV dysfunction model (coronary ligation), mean aortic pressures of 88 mm Hg existed in the presence of a cardiac index of 2.1 L/min/[m.sup.2] (values for this study: aortic pressure, < 50 mm Hg; cardiac index, 3.2 L/min/[m.sup.2]). As the presence of high afterload limits the efficacy of axial flow pumps, insufficient hemod3malnic collapse will not challenge these devices. As the IMP was designed to provide support up to 4.5 L/min, a substantial level of hemodynamic compromise is considered necessary to assess the potential of the device. (9) The induction of AMR did not lead to substantially elevated LAPs. (5) The pre-AMR values of QPA and PASC in Table 1 could be indicative of a distended peripheral arteriolar vascular bed at baseline. Vasodilation is known to reduce the effects of mitral regurgitation. (26) Ultimately, the level of hemodynamic compromise obtained in the present study proved to be effective in characterizing the IMP and the IABP.
Clinical Implications
The present results suggest that the IMP can effectively reduce the cardiac workload while increasing cardiac output and that it outperforms the IABP in low-cardiac-output conditions. This implies that the IMP may be a better alternative in circulatory collapse patients. (4,27) Moreover, in the critical situation of sudden left heart deterioration, the IMP may provide a safety net, buying time for the medical team to act.
Although the present study has illustrated the potential of the IMP to take over the left heart pump function (Fig 5), it must be realized that the pumping capacity heavily depends on the availability of preload. Right-sided circulatory failure seriously limits the effectiveness of LV assist devices and is a contraindication for their use. (28,29)
In the treatment of unstable patients with angina, both the IMP and the IABP would be beneficial in terms of sustained afterload reduction and coronary perfusion enhancement. (23) As timing and synchronization are critical when using the IABP, the continuous-flow IMP might perform more consistently than the IABP in rhythmically unstable patients (eg, atrial fibrillation).
The IMP is a device with a diameter of 6.4 mm (19F) that requires surgical implantation under direct vision. A smaller version of the IMP would allow easier percutaneous introduction and might stretch the indications for intracorporeal support beyond those for the IABP. Moreover, both systems could prove synergetic when applied simultaneously.
CONCLUSION
We studied the hemodynamic efficacy of the IMP and an IABP in a bovine model of AMR. We concluded that in more severely compromised subjects, and in the event of sudden decompensation due to severe acute LV pump failure, the IMP is capable of more effective cardiac and circulatory support than the IABP.
* From the Departments of Cardiothoracic Surgery, (Mr Reesink, Mr. Dekker, and Drs. Soemers, Geskes, van der Veen, and Maessen) and Cardiology, (Dr. van Ommen), Cardiovascular Research Institute Maastricht, Academic Hospital Maastricht, Maastricht, the Netherlands.
REFERENCES
(1) Weber KT, Janicki JS. Intraaortic balloon counterpulsation: a review of physiological principles, clinical results, and device safety. Ann Thorac Surg 1974; 17:602-636
(2) Kantrowitz A, Cardona RR, Freed PS. Percutaneous intraaortic balloon counterpulsation. Crit Care Clin 1992; 8:819-837
(3) Mueller HS. Role of intra-aortic counterpulsation in cardiogenic shock and acute myocardial infarction. Cardiology 1994; 84:168-174
(4) Hollenberg SM, Kazinsky CJ, Parrillo JE. Cardiogenic shock. Ann Intern Med 1999; 131:47-59
(5) Dekker AL, Reesink KD, van der Veen FII, et al. Intraaortic balloon pumping in acute mitral regurgitation reduces aortic impedance and regurgitant fraction. Shock 2003; 19:334-338
(6) Lonn U, Peterzen B, Granfeldt H, et at. Hemopump treatment in patients with postcardiotomy heart failure. Ann Thorac Surg 1995; 60:106-1071
(7) Nishimura Y, Meyns B, Ozaki S, et al. The enabler cannula pump: a novel circulatory support system. Int J Artif Organs 1999; 22:317-323
(8) Dekker AL, Geskes GG, Cramers AA, et al Right ventricular support for off-pump coronary artery bypass grafting studied with bi-ventricular pressure-volume loops in sheep. Eur J Cardiothorac Surg 2001; 19:179 184
(9) Dekker AL, Reesink KD, van der Veen FH, et al. Efficacy of a new intra-aortic propeller pump versus the intra-aortic balloon pump: an animal study. Chest 2003; 123:2089-2095
(10) Autschbach R, Rauch T, Engel M, et al A new intracardiac microaxial pump: first results of a multicenter study. Artif Organs 2001; 25:327-330
(11) Meyns B, Autschbach R, Boning A, et al. Coronary artery bypass grafting supported with intracardiac microaxial pumps versus normothermic cardiopulmonary bypass: a prospective randomized trial. Eur J Cardiothorac Surg 2002; 22:112-117
(12) Reul HM, Akdis M. Blood pumps for circulatory support. Perfusion 2000; 15:295-311
(13) Siess T, Nix C, Menzler F. From a lab type to a product: a retrospective view on Impella's assist technology. Artif Organs 2001; 25:414-421
(14) Steendijk P, van der Velde ET, Baan J. Left ventricular stroke volume by single and dual excitation of conductance catheter in dogs. Am J Physiol 1993; 264:H2198-H2207
(15) Baan J, Van der Velde ET, De Bruin PIG, et al. Continuous measurement of left ventricular volume in animals and humans by conductance catheter. Circulation 1984; 70:812-823
(16) Amirhamzeh MM, Dean DA, Jia CX, et al. Validation of right and left ventricular conductance and echocardiography for cardiac function studies. Ann Thorac Surg 1996; 62:1104-1109
(17) Guyton AC, Hall JE. Textbook of medical physiology. 9th ed. Philadelphia, PA: WB Saunders, 1996; 116
(18) Suga H, Hisano R, Hirata S, et al Mechanism of higher oxygen consumption rate: pressure-loaded vs. volume-loaded heart. Am J Physiol 1982; 242:H942-H948
(19) Norton JM. Toward consistent definitions for preleod and afterload. Adv Physiol Educ 2001; 25:53-61
(20) Marks JD, Pantalos GM, Long JW, et al. Myocardial mechanics, energetics, and hemodynamics during intraaortic balloon and transvalvular axial flow hemopump support with a bovine model of ischemic cardiac dysfunction. ASAIO J 1999; 45: 602-609
(21) Suga H. Total meebanieal energy if a ventricle model and cardiac oxygen consumption. Am J Physiol 1979; 236:H498-H505
(22) Teien DE, Jones M, Shiota T, et al. Left ventricular stroke work in mitral regurgitation: an animal experimental study. J Heart Valve Dis 1997; 6:613-620
(23) Torchiana DF, Hirsch G, Buckley MJ, et al. Intraaortic balloon pumping for cardiac support: trends in practice and outcome, 1968 to 1995. J Thorac Cardiovasc Surg 1997; 113:758-769
(24) Hornick P, Taylor K. Pulsatile and nonpulsatile perfusion: the continuing controversy. J Cardiothorac Vase Anesth 1997; 11:310-315
(25) Van Ommen VG, van den Bus AA, Pieper M, et al. Removal of thrombus from aortocoronary bypass grafts and coronary arteries using the 6Fr Hydrolyser. Am J Cardiol 1997; 79:1012-1016
(26) Yoran C, Yellin El, Becker RM, et al. Mechanism of reduction of mitral regurgitation with vasodilator therapy. Am J Cardiol 1979; 43:773-777
(27) Nishimura RA, Schaff HV, Shub C, et al. Papillary muscle rupture complicating acute myocardial infarction: analysis of 17 patients. Am J Cardiol 1983; 51:373-377
(28) Farrar D, Compton P, Hershon J, et al. Right ventricular function in an operating room model of mechanical left ventricular assistance and its effects in patients with depressed left ventricular function. Circulation 1985; 72:1279-1285
(29) Chen JM, Rose EA. Management of periooperative right-sided circulatory failure. In: Goldstein DJ, Oz M, eds. Cardiac assist devices. Armonk, NY: Futura Publishing, 2000; 83-101
Manuscript received July 29, 2003; revision accepted April 29, 2004.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org)
Correspondence to: Frederik H. van der Veen, PhD, Department of Cardiothoracic Surgery, Academic Hospital Maastricht, P. Debyelaan 25, 6229HX, Maastricht, the Netherlands; e-mail; Erik.vanderveen@ctc.unimaas.nl
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group