Study objectives: Inhalation of nitric oxide (NO) can ameliorate pulmonary ischemia/reperfusion (I/R) injury of the lung in several experimental models, but toxic effects of NO were also reported. Here we investigate whether NO inhalation for a short period prior to surgery is sufficient to prevent symptoms of lung I/R injury, especially the inflammatory response.
Design: Using an in situ porcine lung model, normothermic left lung ischemia was maintained for 90 min, followed by a 5-h reperfusion period (group 1, n = 7). In group 2 (n = 6), I/R was preceded by inhalation of NO (10 min, 15 ppm). Animals in group 3 (n = 7) underwent sham surgery without NO inhalation or ischemia.
Measurements: Oxygenation and hemodynamic parameters were measured as indicators of lung functional impairment. Plasma levels of interleukin (IL)-1[beta], IL-6, and transforming growth factor (TGF)-[beta]1 were determined throughout the I/R maneuver. In addition, tissue macrophages were analyzed by lectin binding.
Results: Symptoms of I/R injury (pulmonary hypertension and decreased oxygenation) in group 1 animals were attenuated by NO inhalation. The reperfusion-induced increases of the levels of IL-1[beta] and IL-6 in plasma were reduced by NO pretreatment. A peak of TGF-[beta]1 immediately after NO administration was observed in group 2, but not in groups 1 and 3. There was no significant effect of NO on tissue macrophages.
Conclusion: NO inhalation for a short period prior to lung I/R is sufficient to protect against pulmonary hypertension, impaired oxygenation, and the inflammatory response of pulmonary I/R injury.
Key words: cytokine; inflammation; lung; nitric oxide; pig; preconditioning; reperfusion injury
Abbreviations: DBL = Dolichos biflorus lectin; ELISA = enzyme-linked immunosorbent assay; IL = interleukin; I/R = ischemia/reperfusion; NO = nitric oxide; TGF = transforming growth factor
**********
Lung transplantation is currently an accepted therapeutic option for several end-stage pulmonary diseases. (1.2) Despite improvements in surgical and perioperative techniques, ischemia/reperfusion (I/R) injury is still a major cause of early graft failure. Pulmonary I/R injury is characterized by several interacting processes, including impairment of epithelial integrity and permeability, release of inflammatory cytokines and reactive oxygen species, cellular infiltration, and microvascular injury. These effects can result in edema, pulmonary hypertension, impaired oxygenation, mad hypoxemia. Severe I/R injury can be associated with an increased risk of rejection. (3)
In spite of extended research efforts, the ability to prevent I/R injury is still limited. At least in experimental animal models, the application of brief, sublethal ischemic episodes (ischemic preconditioning) can ameliorate file consequences of extended I/R later on. (4) The inhalation of nitric oxide (NO), a compound with vasodilatory, anti-inflammatory, and anticoagulative activity, is another approach to attenuate symptoms of I/R injury. Conflicting results were reported, which may be due to different dosage, duration, and timing of administration. (5-12) The application of NO strictly ahead of the ischemic period in a preconditioning mode was only rarely evaluated. Short-term inhalation of NO maintained the endothelial integrity during a subsequent I/R treatment in an ex vivo rabbit lung model, and evidence was presented that nonvasodilatory and cyclic guanosine monophosphate-independent mechanisms are largely responsible for this effect. (11) In this laboratory, a porcine model of in situ I/R was used to further evaluate the effects of short-term NO inhalation on the consequences of a subsequent I/R maneuver. (13) Measurements of several hemodynamic parameters and of plasma levels of reactive oxygen species throughout ischemia and a 5-h reperfusion phase indicated the amelioration of I/R injury.
The pathologic picture in ischemic tissue injury shares features with the inflammatory response, including production of proinflammatory cytokines and the activation and tissue invasion of mononuclear and polymorphonuclear leukocytes. (3) Interleukin (IL)-1[beta] and IL-6 are among the most frequently studied cytokines in relation to lung inflammatory injuries. IL-1[beta] is a 17-kd polypeptide that is to a major part produced in monocytes and macrophages. The expression of this cytokine in rat lung tissue was closely related to I/R injury, (14) and intratracheal instillation of recombinant IL-1[beta] together with tumor necrosis factor induced edema. (15) Only recently, a functional role of IL-1[beta] in an intact animal model of lung I/R injury was established. Administration of anti-IL-1[beta] antibodies before reperfusion significantly reduced lung permeability, neutrophil content, and general histologic injury. (16) IL-6 is a pleiotropic cytokine with both proinflammatory and anti-inflammatory functions. This cytokine is produced in a variety of cell types, including macrophages, lymphocytes, epithelia and endothelia, smooth-muscle cells, and fibroblasts. Exposure of rats and mice to moderate systemic hypoxia for only 1 to 2 h is sufficient to induce the rapid release of IL-6 into the plasma and to trigger the synthesis in the lung endothelium and in vascular smooth-muscle cells. (17,18) Furthermore, the postoperative levels in plasma have been found to be predictive for the outcome of lung transplantations. (19)
Transforming growth factor (TGF)-[beta]1 is a multifunctional polypeptide that is probably produced by all cell types in the body. TGF-[beta]1 plays important roles in many physiologic processes that are related to the interaction of cells with the extracellular matrix, including immunoregulation, fibrosis, and wound healing. The immunomodulatory function is expressed in multiple ways, for example by antagonizing inflammatory cytokines and by modulating the activation and tissue invasion of leukocytes. (20) The role of TGF-[beta]1 in lung transplantation and I/R is underlined by the observation that gene transfer of active TGF-[beta]1 into recipient rats, alone or in combination with IL-10, ameliorated lung graft reperfusion injury and acute lung rejection. (21,22)
Since the release of cytokines from different cell types is known to be regulated by NO from exogenous sources or by modulation of NO synthase activity, (23-25) we speculate that inhalation of NO for a short period prior to an I/R treatment may be sufficient to ameliorate the I/R-induced symptoms of inflammation later on. To address this question in the present investigation, the recently described porcine one-lung in situ model of I/R injury was used. (26) This experimental setting allows for measuring directly and continuously the impact of ischemia and reperfusion on blood constituents, oxygenation, and hemodynamic parameters, with minimal surgical damage to the organ. The plasma levels of IL-1[beta], IL-6, and TGF-[beta]1 were measured to characterize the inflammatory response during treatments. In addition, tissue macrophages were counted after visualizing by lectin binding, since macrophages rather than neutrophils play a major role in the early phase of lung I/R injury. (27,28)
MATERIALS AND METHODS
Surgery and Lung Model
The protocol was approved by the Animal Care Section of the Saxonian Government, Dresden, Germany. and the Animal Care Committee of the University of Dresden. All animals received humane care in compliance with the 1996 guidelines for the care and use of laboratory animals of the National Research Council. Domestic pigs weighing 26 to 33 kg were used in this investigation.
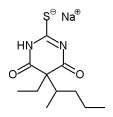
The surgical techniques of thoracotomy and I/R were outlined in a previous communication. (26) Briefly, initial anesthesia was induced by an IM injection of azaperon (200 mg), diazepam (10 mg), and atropine (0.5 mg), followed by infusion of thiopental sodium (6 mg/kg/h) and fentanyl (5 mg/kg/h) into a peripheral ear vein. Animals were placed in supine position for tracheostomy and ventilation (8 to 10 mL/kg body weight, fraction of inspired oxygen of 0.5, and positive end-expiratory pressure of 3 mm Hg). Ventilator settings for a pressure-regulated, volume-controlled mode were initially adjusted to achieve physiologic arterial pH and PC[O.sub.2] values (ABL 700 blood gas analyzer; Radiometer Medicals A/S; Copenhagen, Denmark). This setting was only modified for single lung ventilation during left lung ischemia. Catheters were advanced through the right jugular vein into the right pulmonary artery, through the right carotid artery into the aorta, and ,after 90 min of ischemia into a pulmonary vein of the left lung. Left lateral thoracotomy in the fifth intercostal space was carried out after positioning the animals on their right side. The left lung was then mobilized, the pulmonary hilum was dissected, and perivascular and peribronchial tissue was removed. The animals were placed on a heating pad throughout the experiment to guarantee normothermic conditions.
Study Groups
Animals in group 1 (n = 7, the ischemia group) were heparinized (initially 500 IU/kg, then 160 IU/kg every 2 h), the left pulmonary artery and fire pulmonary veins were clamped, while the left main bronchus was cut off from oxygen supply with a Fogarty catheter. Ventilation continued at twofold frequency and 50% tidal volume (single lung ventilation). These conditions of normothermic ischemia were maintained for 90 min, followed by 5 h of reperfusion. A catheter was placed into the left inferior pulmonary vein at the end of the ischemic period to collect blood directly from the ischemic organ. Group 2 animals (n = 6, the NO group) were treated in the same way as in group 1, except that NO (15 ppm) [Pulmonix; Messer Griesheim; Krefeld, Germany] was mixed to the inspiratory gas flow for 10 min before ischemia was induced. Animals in group 3 (n = 7, control group) underwent sham surgery without NO inhalation and without ischemia-reperfusion. The other surgical steps were the same as in groups 1 and 2.
Analytic Procedures
Numerous hemodynamic and respiratory parameters as well as blood gases and pH were measured and recorded as outlined in a previous commmunication. (26) The timing of data assessment is illustrated in a schematic diagram of the study protocol (Fig 1).
Representative tissue samples from the left lung were excised after dissection of the hilum (sample 2 in Fig 1) and at the end of the observation period (sample 8). The incisions were sealed with a 3/0 polypropylene suture. For lectin staining of macrophages, (29) lung tissue samples were fixed in 4% formaldehyde and embedded in paraffin. Binding sites in deparaffinized and hydrated sections were demasked by ultrasonic treatment in Na-citrate buffer (10 mmol/L, pH 6.0). The sections were overlaid with biotin-conjugated lectin from Dolichos biflorus (dilution, 1:800; Vector Laboratories; Burlingame, CA) for 16 h at 4[degrees]C. After washing in phosphate-buffered saline solution, the avidin-biotinperoxidase complex technique (Vectastain ABC kit; Vector Laboratories) in combination with diaminobenzidine as peroxidase substrate (DAB Chromogen; Dako Diagnostika; Hamburg, Germany) was used to visualize lectin-binding sites. Sections were then counterstained with Mayer hemaioxylin (Merck KgaA; Darmstadt, Germany) and coverslipped with Vectamount (Vector Laboratories). For quantification of cells, 20 fields (50x50[micro]m) were evaluated in every group.
[FIGURE 1 OMITTED]
The levels of IL-1[beta] and IL-6 in arterial plasma were measured using commercial enzyme-linked immunosorbent assay (ELISA) kits (Quantikine colorimetric ELISA for porcine cytokines; R&D Systems GmbH; Wiesbaden, Germany). The TGF-1[beta] ELISA kit used in this study (ELISA for human TGF-[beta]1; R&D Systems) is cross-reactive for porcine samples (data not published). The procedure to activate latent TGF-[beta]1 in the test kit was not used for the detection of active TGF-[beta]1
Statistical Analysis
All values are expressed as mean [+ or -] SD. Differences between groups over time were analyzed with analysis of variance for repeated measurements. After global testing, post hoc Bonferroni procedures were applied; p<0.05 was considered statistically significant.
RESULTS
Functional Lung Parameters
At the end of a 90-min ischemia and 5-h reperfusion regime, the ischemic (left) lungs of group 1 animals showed a marked impairment of lung function (Fig 2). The pulmonary vascular resistance was increased 1.4-fold over control animals, and the pulmonary venous P[O.sub.2] was reduced to 63% of control group. When lungs were ventilated for 10 min with 15 ppm of NO shortly before onset of ischemia, both parameters showed exactly the same values as in control animals.
[FIGURE 2 OMITTED]
Plasma Cytokines
The concentration of several cytokines in arterial plasma from the aorta was determined at various time points throughout the I/R maneuver. The concentration of IL-1[beta] in group 1 animals was significantly decreased, close to control group levels, at the end of the ischemia period (Fig 3, top, A). The plasma IL-1[beta] level started to increase after 1 h of reperfusion to 122 pg/mL after 5 h, with a highly significant intermediary drop to near baseline level. The effect of NO on the IL-1[beta] level is characterized by a peak directly after inhalation (sample 2), and the subsequent reduction to the level in the control group.
[FIGURE 3 OMITTED]
In contrast, IL-6 was below detection level in all groups during NO inhalation and ischemia (Fig 3, middle, B). The plasma concentration in the ischemia group started to increase after 1 h of reperfusion to reach 316 pg/mL at the end of the observation period, with a significant intermediary drop after 4 h of reperfusion (sample 7), while an only moderate increase of IL-6 was observed in the NO group and, at a very low level, in control animals.
Among the tested cytokines, TGF-[beta]1 was least affected by the different treatments (Fig 3, bottom, C). The most remarkable finding was the 2.2-fold reversible increase over baseline in the NO group directly after inhalation. At 10 min into ischemia (sample 3), levels of TGF-[beta]1 in both groups 1 and 2 dropped to nearly the same low values of 2,050 pg/mL and 2,240 pg/mL, respectively, accounting for a 3.3-fold decrease in the NO group. At the end of the observation period, the levels in control animals (2.2-fold) and in the ischemia group (1.9-fold) were higher compared to NO-treated animals.
Tissue Macrophages
Macrophages in lung tissue sections were detected by histochemical means using Dolichos biflorus lectin (DBL). A pronounced raise over control animals was observed in both/JR groups--4.8-fold (I/R) and 5.6-fold (I/R and NO)--at the end of the reperfusion period (sample 8), but without a significant difference between these groups. However, the number of DBL-binding macrophages was significantly higher in the I/R and NO group compared to group 1 (2.3-fold) and group 3 (3.1-fold) when samples were taken at the second point in time, directly after the end of the NO inhalation.
DISCUSSION
Ischemia for 90 min and reperfusion (5 h) in the porcine in situ one-lung model resulted in the deterioration of two essential functional parameters: oxygenation capacity and pulmonary venous resistance. Both effects were completely prevented by short-term inhalation of NO in a moderate concentration of 15 ppm (Fig 2). NO was only applied strictly ahead of the ischemic phase, and therefore it has to be concluded that the direct impact of NO and its metabolites on the vascular tone and on oxygenation has long vanished when the amelioration of the I/R injury was observed. In a previous communication,(13) it was therefore suggested to use the term NO preconditioning in this connection, by analogy with the long-known ischemic preconditioning.
Several reports (5-12) on the effect of inhaled NO lung I/R injury have been presented, but NO was usually administered during the ischemia and/or the reperfusion phase. In most cases, at least a partial amelioration of the I/R-induced lung damage was found. However, the underlying mechanisms are not completely dear, since different and partly contradictory results were observed. For example, Murakami et al (7) suggested that the reduction of I/R injury in blood-perfused isolated rat lungs might be mediated by the inhibition of neutrophil sequestration, whereas a mechanism independent of inhibition of leukocyte-endothelial cell interactions was suggested by Chetham et al (9) using a salt solution-perfused rat lung model. Eppinger et al (5) reported that I/R injury in an in situ rat lung model follows a bimodal pattern, with injury peaks at 30 min and 4 h of reperfusion. The 4-h peak is dependent on neutrophil participation, and the first peak is not. Inhalation of NO was toxic in the early phase, possibly because of the formation of peroxynitrite from NO and superoxide shortly after the beginning of reperfusion, whereas NO inhalation was protective at 4 h of reperfusion, partially due to reduction of neutrophil sequestration. (5) The observation that NO inhalation during the early reperfusion phase can lead to exacerbation of I/R injury was supported by Kao et al, (12) who found increased lung permeability after 50 min of reperfusion using a similar in situ, perfused rat model. Taken together, attempts to use NO inhalation during I/R have led to contradictory results, depending oil the experimental setting and timing of both, NO application and I/R. Inhalation of NO during a short phase directly at the beginning of reperfusion can result in deleterious effects, especially in in situ, blood-perfused lung models. In the present report, we show that these problems can be avoided when NO is applied in low dose and for a short phase before the onset of ischemia.
The I/R injury is usually accompanied by a systemic inflammatory reaction, and the release of proinflammatory cytokines sets the stage for the graft rejection response and other complications later on. (3) It is well known that inflammatory processes, like neutrophil adsorption/invasion and cytokine release, are suppressed in the presence of increased NO levels. (23-25) Figure 3 shows that NO, when applied in the preconditioning mode before ischemia, also prevented the reperfusion-induced increase of the proinflammatory cytokines, IL-1[beta] and IL-6. The levels in plasma of both cytokines show a biphasic response during I/R. A first peak at 2 h of reperfusion (IL-1[beta]) and at 3 h (IL-6) is followed by a pronounced drop at 4 h and an increase at the end of the observation period (5 h of reperfusion). The underlying mechanism was beyond the scope of this study, but it may be speculated that this observation is functionally related to the previously described bimodal development of I/R injury in the rat model, (27,28) Further, increased plasma levels of IL-1[beta] before the onset of I/R at the first and second time points were also observed. This effect may be due to initial surgery, narcosis, and general mechanical trauma of the lung.
The secondary mediator, IL-6, is a reliable indicator of the extent of inflammation in various injuries. (30) We have shown an increase of IL-6 during the reperfusion period, in accordance with the conclusion of others that reperfusion injury, rather than ischemia, is the stimulus for the release of the cytokine. (31) Inhalation of NO significantly abrogates this effect (Fig 3). Together with the similar observations with IL-1[beta], the results suggest that early NO inhalation ameliorates the reperfusion-induced systemic inflammation. As the pleiotropic cytokine IL-6 is produced in numerous cell types, further studies have to show how far macrophages or other inflammatory cells are responsible of these effects, especially, the cellular basis for the drop of the IL-6 plasma level at 4 h of reperfusion is not clear.
Gene transfer experiments have shown that increased expression of TGF-[beta]1 protects from I/R related lung impairments. (21,22) Here we have demonstrated that NO inhalation results in an intermediary increase of the TGF-[beta]1 plasma level directly following administration. This effect was completely reversed during the subsequent ischemia episode (Fig 3, bottom, C). The NO-stimulated release of TGF-[beta]1 has been also found by others in cell culture models. In the presence of the NO donor, S-nitroso N-acetylpenicillamine, an increase of the level of the cytokine in the culture medium of the lung epithelial cell line A549 was already detected after 3 h of incubation. (32) Mehta et al (33) showed that the NO donor 3-morpholinosydnonimine and nitroglycerin reversed the I/R induced reduction of the level of active TGF-[beta]1 in the culture medium of myocardial myocytes. In both cases, long-term effects were measured, with exposure times and hypoxiareoxygenation cycles of up to 24 h. To our knowledge, the rapid effect of a short-term exposure to NO on the release of TGF-[beta]1 has not been described. It should be emphasized that there is no NO-only group in this study. Therefore, merely effects of NO in combination with I/R were observed.
The immediate response to NO inhalation suggests that TGF-[beta]1 was released from preformed stores rather than produced by de novo synthesis. It should be noted that the ELISA test that was used here detected TCF-[beta]1 only in its active form. The growth factor is present in plasma also in a latent form, meaning that it is bound to an inhibitory protein, latency-associated protein. (34) The finding of Vodovotz et al (35) that direct postranslational modification and inactivation of latency-associated protein by NO via S-nitrosylation can stabilize active TCF-[beta]1 in plasma may therefore be of functional relevance in this connection.
Evidence is accumulating that the cellular response of the lung to I/R is mediated by macrophages in the early phase of reperfusion, whereas neutrophil-dependent events are restricted to a later phase. (27,28,36) Since the present investigation focuses on the early phase of reperfusion and preconditioning, macrophages were counted using histochemical staining with DBL. This lectin has been established as a marker of macrophage activation and functional specification. (37,38) In the I/R groups, a pronounced increase of lectin-binding macrophages was observed, indicating major synthesis or remodeling of carbohydrate structures. In addition, an increase in cell number due to monocyte invasion or proliferation may have contributed to this effect. Preconditioning by NO inhalation did not prevent this finding. On the contrary, the stimulation of macrophage lectin binding shortly after NO inhalation was observed. Since the lectin-binding sites are not functionally characterized, the physiologic relevance of the latter result is not clear.
Macrophages are the main source of inflammatory cytokines during the early phase of I/L-induced inflammation in the lung. (25) The results of Figure 4 show that the efficient prevention of the cytokine release in the NO group cannot be attributed to the number of cells or their general activation state. We assume that the well-documented direct inhibitory effect of NO on the cytokine synthesis in macrophages (25,39-41) is responsible for this effect.
[FIGURE 4 OMITTED]
CONCLUSION
A brief episode of NO inhalation prior to an extended I/R treatment of the lung is sufficient to prevent I/R induced impairment of lung function. The I/R associated inflammation--indicated by the release of the inflammatory cytokines, IL-1[beta] and IL-6, during reperfusion--is also suppressed by the NO pretreatment. Since toxic effects of long-term NO administration are avoided, this treatment is potentially important to improve donor lung preservation or in other clinical situations in which lung ischemia is likely to occur. Future work will be needed to identify the underlying mechanisms, especially the problem in which way NO, a very short-lived compound in blood and tissues, can exert effects that are detectable for several hours after administration.
REFERENCES
(1) Meyers BF, Lych J. Trulock EP, et al. Lung transplantation: a decade of experience. Ann Surg 1999; 230:362-370
(2) DeMeo DL, Ginns LC. Clinical status of lung transplantation. Transplantation 2001; 72:1713-1724
(3) de Perrot M, Liu M, Waddell KT, et al. Ischemia-reperfusion-induced lung injury. Am J Respir Crit Care Med 2003; 167:490-511
(4) Tomai F, Crea F, Chiariello L, et al. Isehemic preconditioning in humans: models, mediators and clinical relevance. Circulation 1999;100:559-563
(5) Eppinger MJ, Ward PA, Jones ML, et al. Disparate effects of nitric oxide on lung ischemia-reperfusion injury. Ann Thorac Surg 1995; 60:1169-1176
(6) Hausen B, Muller P, Bahra M, et al. Donor pretreatment with intravenous prostacyclin versus inhaled nitric oxide in experimental lung transplantation. Transplantation 1996; 62: 1714-1719
(7) Murakami S, Bacha EA, Herve P, et al, Prevention of reperfusion injury by inhaled nitric oxide in lungs harvested from non-heart-beating donors. Ann Thorac Surg 1996; 62: 1632-1638
(8) Terada LS, Mahr NN, Jacobsen ED. Nitric oxide decreases lung injury after intestinal ischemia. J Appl Physiol 1996; 81:2456-2460
(9) Chetham PM, Sefton WD, Bridges JP, et al. Inhaled nitric oxide pretreatment but not post-treatment attenuates ischemia-reperfusion-induced pulmonary microvascular leak. Anesthesiology 1997; 86:895-902
(10) Hermle G, Schutte H, Walmrath D, et al. Ventilation-perfusion mismatch after lung ischemia-reperfusion: protective effect of nitric oxide. Am J Respir Crit Care Med 1999; 160:1179-1187
(11) Schutte H, Witzenrath M, Mayer K, et al. Short-term "pre-conditioning" with inhaled nitric oxide protects rabbit lungs against isehemia-reperfusion injury. Transplantation 2001; 72:1363-1370
(12) Kao SJ, Peng T-C, Lee RP, et al. Nitric oxide mediates lung injury induced by ischemia-reperfusion in rats. J Biomed Sci 2003; 10:58-64
(13) Waldow T, Roth-Eichhorn S, Herzog T, et al. Protective effect of NO inhalation on lung injury in an in vivo pig mode of warm pulmonary ischemia in association with decreased serum levels of reactive oxygen species [abstract]. Chest 2001; 120(suppl):169
(14) Chang D-M, Hsu K, Ding Y-A, et al. Interleukin-l in ischemia-reperfusion acute lung injury. Am J Respir Crit Care Med 1997; 156:1230-1234
(15) Wesselius LJ, Smirnow IM, O'Brien-Ladner AR, et al. Synergism of intratracheally administered tumor necrosis factor with interleukin-1 in the induction of lung edema in rats. J Lab Clin Med 1995; 125:618-625
(16) Krishnadasan B, Naidu BV, Byrne K, et al. The role of proinflammatory cytokines in hang ischemia-reperfusion injury. J Thorac Cardiovasc Surg 2003; 125:261-272
(17) Yen SF, Tritto I, Pinsky D, et al. Induction of interleukin 6 (IL-6) by hypoxia in vascular ceils: central role of the binding site for nuclear factor-IL-6. J Biol Chem 1995; 270:11463-11471
(18) Hiki N, Mimura Y, Hatao F, et al. Sublethal endotoxin administration evokes super-resistance to systemic hypoxia in rats. J Trauma 2003; 54:584-589
(19) Pham SM, Yoshida Y, Aeba R, et al. Interleukin-6, a marker of preservation injury in clinical lung transplantation, J Heart Lung Transplant 1992; 11:1017-1024
(20) Letterio JJ, Roberts AB. Regulation of immune responses by TGF-[beta]. Annu Rer Immunol 1998; 16:137-161
(21) Suda T, D'Ovidio F, Daddi N, et al. Recipient intramuscular gene transfer of active transforming growth factor-[beta]1 attenuates acute lung rejection. Ann Thorac Surg 2001; 71:1651-1656
(22) Daddi N, Suda T, D'Ovidio, et al. Recipient intramuscular cotransfection of naked plasmid transforming growth factor [beta]1 and interleukin 10 ameliorates lung graft ischemia-reperfusion injury. J Thorac Cardiovasc Surg 2002; 124:259-269
(23) Walley KR, McDonald TE, Higashimoto Y, et al. Modulation of proinflammatory cytokines by nitric oxide in murine acute lung injury. Am J Respir Crit Care Med 1999; 160:698-704
(24) Gnidot DM, Hybertson BM, Kitlowski RP. et al Inhaled NO prevents IL-1-induced neutrophil accumulation and associated edema in isolated rat hangs. Am J Physiol 1996; 271: L225-L229
(25) Meldrum DR, Shames BD, Meng X, et al. Nitric oxide downregulates lung macrophage inflammatory cytokine production. Ann Thorac Surg 1998; 66:313-317
(26) Wagner FM, Weber AT, Ploetze K, et al. Do vitamins C and E attenuate the effects of reactive oxygen species during pulmonary reperfusion and thereby prevent injury? Ann Thorac Surg 2002; 74:811-818
(27) Eppinger MJ, Deeb GM, Boiling SF, et al. Mediators of ischemia-reperfusion injury of rat lung. Am J Pathol 1997; 150:1773-1784
(28) Fiser MS, Tribble CG, Long MS, et al. Lung transplant reperfusion injury involves pulmonary macrophages and circulating leukocytes in a biphasic response. Cardiovasc Surg 2001; 121:1069-1075
(29) Kasper M, Rudolf T, Hahn R, et al. Immuno- and lectin histochemistry of epithelial subtypes and their changes in a radiation-induced lung fibrosis model of the mini pig. Histochemistry 1993; 100:367-377
(30) Biffl WL, Moore EE, Moore FA, et al. Interleukin-6 in the injured patient: marker of injury or mediator of inflammation? Ann Surg 1996; 224:647-664
(31) Harkin DW, Barros D'Sa AAB, McCallion K, et al. Ischemic preconditioning before lower limb ischemia-reperfusion protects against acute lung injury, J Vasc Surg 2002; 35:1264-1273
(32) Bellocq A, Azoulay E, Marullo S, et al. Reactive oxygen and nitrogen intermediates increase transforming growth factor-[beta]1 release from human epithelial alveolar ceils through two different mechanisms. Am J Respir Cell Mol Biol 1999; 21:128 136
(33) Mehta JL, Chen HJ, Li DY. Protection of myocytes from hypoxia-reoxygenation injury by nitric oxide is mediated by modulation of transforming growth factor-[beta]1. Circulation 2002; 105:2206-2211
(34) Koli K. Saharinen j, Hyytiainen M, et al. Latency, activation, and binding proteins of TGF-[beta]. Microsc Res Tech 2001; 52:354-362
(35) Vodovotz Y, Cbesler L, Chong H, et al. Regulation of transforming growth factor [beta] by nitric oxide. Cancer Res 1999; 59:2142-2149
(36) Naidu BV, Krishnadasan B, Farivar AS, et al. Early activation of the alveolar macrophage is critical to the development of lung ischemia-reperfusion injury. J Thorac Cardiovasc Surg 2003; 126:200-207
(37) Kasper M. Haroske G. Pollack K, et al. Heterogeneous Dolichos biflorus lectin binding to a subset of rat alveolar macrophages in normal and fibrotic lung tissue, Acta Histochem 1993; 95:1-11
(38) Kasper M, Haroske G, Muller M. Species differences in lectin binding to pulmonary cells: soybean agglutinin (SBA) as a marker of type I alveolar epithelial cells and alveolar macrophages in mini pigs. Acta Histochem 1994; 96:63-73
(39) Thomassen MJ, Buhrow LT, Conners MJ, et al. Nitric oxide inhibits inflammatory cytokine production by human alveolar macrophages. Am J Respir Cell Mol Biol 1997; 17:279-283
(40) Magnan A, Mege JL, Reynaud M, et al. Monitoring of alveolar macrophage production of tumor necrosis factor-[alpha] and interleukin-6 in lung transplant recipients: Marseille and Montreal lung transplantation group. Am J Respir Crit Care Med 1994; 150:684-689
(41) Wishah K, Malur A, Raychaudhuri B, et al. Nitric oxide blocks inflammatory cytokine secretion triggered by CD23 in monocytes from allergic, asthmatic patients and healthy controls. Ann Allergy Asthma Immunol 2002; 89:78-82
* From the Cardiovascular Institute (Drs. Waldow, Alexiou, Witt, Gulielmos, Matschke, and Knaut), University Hospital Dresden, Dresden; and the Department of Cardiovascular Surgery (Dr. Wagner), University Hospital Eppendorf Hamburg, Germany. This study was supported by a donation from Messer Griesheim GmbH, Obcrhausen, Germany.
Manuscript received April 14, 2003; revision accepted November 5, 2003,
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Thomas Waldow, MD, Herzzentrum Dresden, KIinik fur Kardiochtrurgie, Fetscherstr. 76, 01307 Dresden, Germany
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group