Study objectives: Although the sentinel lymph node (SLN) concept has traditionally been applied to solid organs, we hypothesized that the pleural space might drain into a specific SLN group. The identification of such a nodal group could assist in the staging and treatment of pleural-based diseases, such as mesothelioma, or other lung cancers with visceral pleural invasion. The purpose of this study was to determine whether the pleural space has an SLN group.
Design: Sixteen rats underwent right or left pleural space injection of a novel lymph tracer, quantum dots (QDs), which have a hydrodynamic diameter of 15 nm and fluoresce in the near-infrared (NIR) spectrum. Nodal uptake of the entire thorax was imaged with a custom system that simultaneously acquired color video, NIR fluorescence of the QDs, and a merged picture of the two in real-time. Six pigs underwent right or left pleural space injection of QDs and similar imaging.
Measurements and results: In the rat, the QDs drained solely to the highest superior mediastinal lymph node group, corresponding to lymph node station 1, according the regional lymph node classification for lung of the American Joint Committee on Cancer. In one rat, the injection of QDs in the left pleural space resulted in migration to the contralateral station 1 lymph node group. The injection of QDs in the right or left pleural space of the pig resulted in migration solely to the ipsilateral highest superior mediastinal lymph node group.
Conclusions: NIR fluorescence imaging in two species demonstrated that the highest superior mediastinal lymph nodes of station 1 are the SLNs of the pleural space. This study also provides intraoperative feasibility and proof of the concept for identifying lymph nodes communicating with the pleural space on a patient-specific basis, in real-time, and with high sensitivity.
Key words: lymphatic drainage; lymph node; mesothelioma; near-infrared fluorescence; pleural space; sentinel lymph node; visceral pleural invasion
Abbreviations: HSA-78 = IRDye78 conjugated to human serum albumin; NIR = near-infrared; QD = quantum dot; SLN = sentinel lymph node; VPI = visceral pleura] invasion
**********
Knowledge of pleural space lymph node drainage is critical for the accurate staging and treatment of malignant pleural mesothelioma and lung cancer with visceral pleural invasion (VPI). Both in patients with mesothelioma and in those with VPI, staging is dependent on the assessment of the lymph nodes draining the pleural space, (1-3) and in both diseases locoregional control has positive prognostic value. (4,5) Thus, the identification of a sentinel lymph node group may aid in the staging and treatment of both diseases.
Previous studies have mapped node groups communicating with the pleural space, but none have focused on the first group, the sentinel lymph node (SLN) group, to drain the pleural space. Pleural lymph node drainage patterns were first established through anatomic dissection in animal and human cadavers. Different studies (6,7) have suggested a connection of the pleural space with intercostal, superior mediastinal, and tracheobronchial nodes. We have previously reported (8) the temporal in vivo pattern of pleural lymph drainage in rats and pigs. A novel lymph tracer composed of recombinant human serum albumin covalently conjugated to the near-infrared (NIR) fluorophore IRDye78 conjugated to human serum albumin (HSA-78) demonstrated that the pleural space drained to the highest superior mediastinal lymph node group within 30 rain, followed by other intrathoraeic and extrathoracic lymph node groups over the course of 24 h. These findings suggested that there might actually be an SLN group for the pleural space; however, the hydrodynamic diameter of HSA-78 is such that flow through the first nodal group is possible.
The purpose of our study was to identify whether the pleural space has an SLN group. To answer this question, we use quantum dots (QDs), which are engineered to travel through lymph channels but stop within the first encountered lymph node. QDs are also engineered to provide highly sensitive intraoperative detection of SLNs using NIR fluorescent light.
MATERIALS AND METHODS
Intraoperative NIR Fluorescence Imaging System
The imaging system has been described in detail previously. (9) Briefly, it is composed of two wavelength-isolated excitation sources, one generating 400 to 700 nm "white" light (0.5 mW/ [cm.sup.2]) and another generating 725 to 775 nm NIR fluorescenceexcitation light (5 mW/[cm.sup.2]) over a field of view that is 15 cm in diameter. Photon collection is achieved with custom-designed optics that maintains the separation of the white light and NIR fluorescence (ie, > 795 nm) channels. After computer-controlled camera acquisition, anatomic (white light) and functional (NIR fluorescent light) images can be displayed separately and merged. All images are refreshed 15 times per second. The entire apparatus is suspended on an articulated arm over the surgical field, thus permitting noninvasive and nonintrusive imaging. Real-time video images and zooming capability allowed for precise localization and dissection as needed.
NIR Fluorescent Lymph Tracer
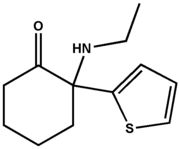
The chemical properties and optical character of QDs have been described in detail previously. (10) Briefly, these type-II core/shell QDs are semiconductor nanocrystals that contain an inorganic core of cadmium telluride, an inorganic shell of cadmium selenide, and an outer organic coating of solubilizing oligomeric phosphines. QDs are stable for in vivo applications, and are engineered with a hydrodynamic diameter of 15 to 20 nm to maximize both rapid uptake into the lymphatic system and retention in the first draining lymph node. These particular QDs were engineered to fluoresce in the NIR, with peak emission at 840 nm. A stock solution of 5.7 [micro]mol/L QDs in phosphate-buffered saline, pH 7.4 was used for all studies. QD fluorescence can be detected through 1 cm of solid tissue (10) and 5 cm of lung tissue. (11)
Small Animal Studies
Animal protocols were performed in accordance with Institutional Animal Care and Use Committee Guidelines including the "Guide for the Care and Use of Laboratory Animals" published by the National Institute of Health (publication 5-23). Adult male Sprague-Dawley rats that were 200 g in weight were anesthetized with xylazine, 10 mg/kg, and ketamine, 100 mg/kg, intraperitoneally. Twelve rats were shaved, prepped, and draped in the usual sterile fashion. A 2-cm midline laparotomy incision was made from the xyphoid to the mid-abdomen. The right pleura] space was visualized through the diaphragm. QDs (5.7 [micro]mol/L, 30 [micro]L per animal, 171 pmol per animal, 855 pmol/kg body weight) were administered in the right pleural space through a low, trans-thoracie injection using a 25-gauge needle. The injection of QDs was monitored in real time through the diaphragm with the NIR fluorescence imaging system to confirm even distribution throughout the desired pleural space, and not in the lung or subpleural tissue. (8) The injection of QDs in the pleural space through higher thoracic levels, or through the diaphragm, resulted in an equally even distribution of tracer throughout the pleural space; however, for this study, only low transthoracic injections were used. Four rats then underwent imaging at 4, 12, or 24 h after injection. Four additional rats received injections of QDs in the left pleural space and underwent imaging at 24 h. At the time of imaging, animals received redosing of anesthesia as necessary. Animals underwent intubation with a 16-gauge catheter and were ventilated appropriately. Thorough exposure and in vivo investigation of all lymph node groups of the thorax, chest wall, neck, axilla, and intraabdominal compartment was performed. Histology was performed on fluorescing tissue to confirm the presence of lymph nodes. Nonfluorescing lymph nodes routinely sampled in conventional cervical mediastinoscopy such as stations 4L, 4R, 7, and 10, and in hilar nodes were also sent for histologic testing for comparison.
Large Animal Studies
Animal protocols were performed in accordance with Institutional Animal Care and Use Committee Guidelines including the "Guide for the Care and Use of Laboratory Animals" published by the National Institute of Health (publication 5-23). Three Yorkshire pigs (E.M. Parsons and Sons; Hadley, MA) that weighed 35 kg were anesthetized with IM tiletamine/zolazopam (Telazol, Fort Dodge Labs, Fort Dodge, IA), 4.4 mg/kg, and xylazine, 2.2 mg/kg, for the induction of anesthesia. Once sedated, the animals received oxygen and isoflurane 0.5 to 5% to effect. Once the animals were under full anesthesia, the trachea was intubated using a 7-ram cuffed endotracheal tube. The animals were prepped and draped in the usual sterile fashion. Three pigs underwent a right subcostal incision to visualize the diaphragm. QDs at 855 pmol/kg body weight were injected into the right pleural space through a transthoracic approach and under direct image guidance, as described above. Three pigs underwent the same procedure, except the injection of QDs was into the left pleural space. Animals recovered for 24 h. Animals then underwent anesthesia and intubation as described above. Thorough exposure and in vivo investigation of all lymph node groups of the thorax, chest wall, neck, axilla, and intraabdominal compartment was performed. QD-positive lymph nodes in station 1 and QD-negative lymph nodes in stations 1, 4L, 4R, 7, and 10, and in hilar nodes were also sent for histologic testing.
Histology
Lymph nodes were placed in histology cassettes, were embedded (Tissue-Tek O.C.T. compound; Sakura Finetek U.S.A.; Torrance, CA), and were frozen in liquid nitrogen. The nodes were sectioned, and alternate cuts were examined by hematoxylin-eosin staining and NIR fluorescence imaging. The NIR fluorescence was visualized using a modified microscope with custom-designed optics, as described previously. (12)
RESULTS
Pleural Space Drainage of the Rat
QDs injected into the right pleura] space could not be detected within any lymph nodes at 4 or 12 h. At 24 h, QDs drained solely to the ipsilatera] station 1 lymph node group in four of four rats imaged (Fig 1, top, A). Four rats were injected with QDs in the left pleura] space and underwent imaging at 24 h. Again, only the station 1 lymph node group showed the uptake of QDs. Surprisingly, one rat receiving an injection in the left pleural space had QD uptake into the right station 1 lymph node group (Fig 1, top, A).
QD-positive tissue was sectioned and stained with hematoxylin-eosin to confirm that it was indeed lymph node tissue. As described previously, (10) QD fluorescence collected at the periphery of the node (Fig 1, bottom, B). Node group specimens that did not exhibit QD uptake were similarly harvested and analyzed. These included lymph nodes that were routinely sampled with conventional cervical mediastinoscopy such as those at stations 4L, 4R, 7, and 10, and in the hilar nodes. Hematoxylin-eosin staining confirmed that the QD-negative tissues were lymph node tissue, and NIR imaging confirmed the absence of QD fluorescence or autofluorescence (Fig 1, bottom, B).
[FIGURE 1 OMITTED]
Pleural Space Drainage of the Pig
The small animal data encouraged further investigation of pleural space SLN mapping in a larger model approaching file size of humans. Three pigs received a transthoracic injection of QDs in the right pleural space, and three pigs received transthoracic injection of QDs in the left pleural space. At 24 h after injection, QDs were detected solely in the ipsilateral station 1 lymph node group in all pigs (Fig 2, top, A).
[FIGURE 2 OMITTED]
QD-positive tissues in the lymph node basins were excised, and consecutive sections were either stained with hematoxylin-eosin or frozen-sectioned for NIR fluorescence imaging. The hematoxylin-eosinstained images confirmed that the brightly fluorescent specimens were lymph nodes, and NIR fluorescence imaging showed the collection of QDs within the periphery of the node. As a control, nonfluorescing lymph nodes that were routinely sampled in conventional cervical mediastinoscopy such as those at stations 4L, 4R, 7, and 10, and at hilar nodes were also sent for histologic examination for comparison. Hematoxylin-eosin staining confirmed that the specimens were lymph nodes. As expected, the NIR images showed no fluorescence within these nodes (Fig 2, bottom, B).
DISCUSSION
The SLN concept states that the first lymph node to receive lymphatic drainage from a tumor site will contain tumor cells in the setting of direct lymphatic spread. (13) The application of this concept to breast cancer and melanoma has revolutionized the management of these diseases. Instead of performing extended lymphadenectomy based on stage of disease, SLN mapping guides patient-specific lymphadenectomy based on the presence of tumor in the SLN. As this concept is gaining widespread use for the treatment of other solid tumors, it may also be applicable to mapping metastatic spread from the pleural space to the lymph nodes. The drainage of tumor cells in the pleural space to thoracic lymph nodes may explain the clinical finding of advanced nodal stage and poor survival in the setting of VPI. Similarly, mesothelioma that has spread to extrapleural lymph nodes is also associated with poorer survival. Thus, the identification of a pleural space SLN group could direct which nodal stations to biopsy during routine staging mediastinoscopy and which lymph nodes to excise for local control on a patient-specific basis.
Unfortunately, there is no accepted method for identifying SLNs of the pleural space. Lymphatic tracers for breast and melanoma, namely, vital blue dyes and/or [sup.99m]Tc, pose several technical obstacles in mapping the lymphatic drainage of the pleural space. The thorax often contains anthracotic lymph nodes that can easily be confused with vital blue dyepositive nodes. When using an intraoperative, handheld gamma probe, [sup.99m]Tc can often create a "shine-through" effect, whereby the injection site creates a confounding positive signal. If the injection site is the entire plural space, this shine-through effect would be even more troublesome in the identification of SLNs.
There are many advantages to using this novel method of NIR fluorescence imaging to identify SLNs of the pleural space. QDs, a type of NIR fluorescent lymph tracer, have a diameter of 15 to 20 rim, which is small enough to travel freely through lymph channels, but is large enough to be trapped within the first encountered lymph node. (10) QDs have been engineered to have robust photostability and large absorption cross-sections, resulting in a bright fluorescence against a low background in vivo. (10) Because QDs can be detected through up to 1 cm of tissue (10) and 5 cm of lung tissue, (11) their accurate administration into and even distribution throughout the pleural space could be seen through the diaphragm and chest wall. (8) Additionally, the entire operative field can be scanned for in situ QD-positive lymph nodes, thus minimizing sampling error. This system of real-time SLN detection also empowers the surgeon with image-guided dissection and excision of lymph nodes. Because the QDs withstand histologic processing, there is another degree of certainty in the detection of QDs in lymph nodes.
NIR fluorescence imaging provided a functional, in vivo, in situ model for the identification of the pleural space SLN. In both the rat and pig models, American Joint Committee on Cancer-defined station 1 lymph nodes proved to be the SLN of the pleural space. It is of interest that the pleural space can drain either into the ipsilateral or contralateral station 1 lymph node, a phenomenon that may be shared by humans. This finding emphasizes a need for the patient-specific identification of SLN of the pleural space. Our findings using QDs as a tracer corroborate the results of an earlier study (8) from our group that employed a smaller NIR-fluorescent lymph tracer called HSA-78. HSA-78, with hydrodynamic diameter of 7 nm, flows through smaller lymph channels and lymph nodes to identify all of the node groups communicating with the pleural space. The highest superior mediastinal lymph node group was the first group to receive pleural space drainage within minutes. Other lymph node groups had HSA-78 uptake at later time points. Given that the highest superior mediastinal lymph node group is the first group to receive the uptake of HSA-78 and the only group to receive the uptake of QDs, we propose that this group, corresponding to station I lymph nodes, is the SLN of the pleural space in the rat and the pig.
Although the lung lymphatic systems in the pig are similar to those in humans, (11,14) we cannot assume that station 1 lymph nodes are the SLN group of the pleural space in humans, nor can we assume that all patients will have the same SLN group. However, the current study establishes the proof of concept and the feasibility of an intraoperative approach to identifying the SLN on an individual basis.
At this point in time, the toxicity of the heavy metal-containing QDs used in this study is unknown. However, we observed no signs of acute toxicity, namely, changes in heart rate, rhythm, BP, or oxygen saturation. Studies directed at establishing the toxicity, if any, of QDs, or developing alternative formulations, will be required prior to human testing. Future studies should also be directed toward adapting the technology to fiberoscopy. Such a system could provide a patient-specific method for identifying SLNs of the pleural space, thus minimizing dissection and directing biopsies during staging mediastinoscopy. This advancement of the technology could, in turn, decrease patient risk and morbidity, and could increase accuracy in the staging of lung cancers.
ACKNOWLEDGMENT: We thank Edward G. Soltesz, MD, Frederick Y. Chen, MD, PhD, Peter M. Kang, MD, and Tomislav Mihaljevic, MD, for many helpful discussions, Alec M. DeGrand, BS, and Rita G. Laurence, BS, for technical assistance, and Grisel Rivera for administrative assistance.
* From the Divisions of Cardiac Surgery (Drs. Parungo and Cohn) Thoracic Surgery (Dr. Colson), Brigham & Women's Hospital, Boston, MA; the Department of Chemistry (Drs. S.-W. Kim, S. Kim, and Bawendi), Massachusetts Institute of Technology, Cambridge, MA; and the Division of Hematology/Oncology and Department of Radiology (Dr. Frangioni), Beth Israel Deaconess Medical Center, Boston, MA.
This work was supported in part by National Institutes of Health National Research Service Award F32 HL72568-01 (C.P.P.), US Department of Energy (Office of Biological and Environmental Research) grant DE-FG02-01ER63188 (J.V.F.), a Proof of Principle Award from the Center for Integration of Medicine and Innovative Technology (J.V.F.), and National Institutes of Health grant R21/R33 EB-000673 (J.V.F. and M.G.B.). The Frangioni boratory presently receives industrial support from General
Electric Corporation to develop a clinical version of the intraoperative NIR fluorescence imaging system described in this study. However, funding for the imaging system used in this study, and for the study itself, was strictly provided by the peer-reviewed grants listed above.
REFERENCES
(1) Sugarbaker DJ, Garcia JP, Richards WG, et al. Extrapleural pneumonectomy in the multimodality therapy of malignant pleural mesothelioma: results in 120 consecutive patients. Ann Surg 1996; 224:288-294
(2) Sugarbaker DJ, Strauss GM, Lynch TJ, et al. Node status has prognostic significance in the multimodality therapy of diffuse, malignant mesothelioma. J Clin Oncol 1993; 11:1172-1178
(3) Mountain CF, Dresler CM. Regional lymph node classification for lung cancer staging. Chest 1997; 111:1718-1723
(4) Kang JH, Kim KD, Chung KY. Prognostic value of visceral pleura invasion in non-small cell lung cancer. Eur J Cardiothorac Surg 2003; 23:865-869
(5) Manac'h D, Riquet M, Medioni J, et al. Visceral pleura invasion by non-small cell lung cancer: an underrated bad prognostic factor. Ann Thorac Surg 2001; 71:1088-1093
(6) Albertine KH, Wiener-Kronish JP, Roos PJ, et al. Structure, blood supply, and lymphatic vessels of the sheep's visceral pleura. Am J Anat 1982; 165:277-294
(7) Okiemy G, Foucault C, Avisse C, et al. Lymphatic drainage of the diaphragmatic pleura to the peritracheobronchial lymph nodes. Surg Radiol Anat 2003; 25:32-35
(8) Parungo CP, Ohnishi S, De Grand AM, et al. In vivo optical imaging of pleural space drainage to lymph nodes of prognostic significance. Ann Surg Oncol 2004; 11:1085-1092
(9) De Grand AM, Frangioni JV. An operational near-infrared fluorescence imaging system prototype for large animal surgery. Technol Cancer Res Treat 2003; 2:553-562
(10) Kim S, Lim YT, Soltesz EG, et al. Near-infrared fluorescent type II quantum dots for sentinel lymph node mapping. Nat Biotechnol 2004; 22:93-97
(11) Soltesz EG, Kim S, Laurence RG, et al. Intraoperative sentinel lymph node mapping of the lung using near-infrared fluorescent quantum dots. Ann Thorac Surg 2005; 79:269-277; discussion 269-277
(12) Zaheer A, Lenkinski RE, Mahmood A, et al. In vivo near-infrared fluorescence imaging of osteoblastic activity. Nat Biotechnol 2001; 19:1148-1154
(13) Uren RF, Hoefnagel CA. Lymphoscintigraphy. In: Thompson JF, Morton DM, Kroon BBR, eds. Textbook of melanoma. London, UK: Martin Dunitz, 2004; chapter 30, 339-364
(14) Riquet M, Souilamas R, Hubsch JP, et al. Lymphatic drainage of the heart and lungs: comparison between pig and man. Surg Radiol Anat 2000; 22:47-50
Manuscript received August 5, 2004; revision accepted November 11, 2004.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml).
Correspondence to: John V. Frangioni, MD, PhD, Division of Hematology/Oncology and Department of Radiology, Beth Israel Deaconess Medical Center, 330 Brookline Avenue, Room SL-B05, Boston, MA, 02215; e-mail: jfrangio@bidmc.harvard.edu
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group