Toradol
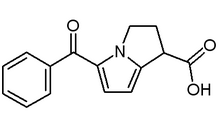
Ketorolac or ketorolac tromethamine (marketed as Toradol® - generics have been approved) is a non-steroidal anti-inflammatory drug (NSAID) in the family of propionic acids, often used as an analgesic, antipyretic (fever reducer), and anti-inflammatory. Ketorolac acts by inhibiting bodily synthesis of prostaglandins. Ketorolac in its oral and intramuscular preparations is a racemic mixture of R-(+)(which is the salt 1H-Pyrrolizine-1-carboxylic acid,5-benzoyl-2,3-dihydro- ketorolac) and S-(-) (which does not have the 1H-Pyrrolizine-1-carboxylic acid,5-benzoyl-2,3-dihydro group) ketorolac. more...
The brand name Toradol was coined by the Syntex company of the United States.
This article does not cover Acular® or ophthalmic ketorolac.
Chemistry
Ketorolac, like other 2-arylpropionate derivatives (including ketoprofen, flurbiprofen, naproxen, ibuprofen etc.) contains a chiral carbon in the β-position of the propionate moiety. As such there are two possible enantiomers of ketorolac with the potential for different biological effects and metabolism for each enantiomer.
NSAIDs are not recommended for use with other NSAIDs because of the potential for additive side effects.
The protein-binding effect of most non-aspirin NSAIDs is inhibited by the presence of aspirin in the blood.
Mechanism of action
The primary mechanism of action responsible for Ketorolac's anti-inflammatory/antipyretic/analgesic effects is the inhibition of prostaglandin synthesis by competitive blocking of the the enzyme cyclooxygenase (COX). Like most NSAIDs, Ketorolac is a non-selective cyclooxygenase inhibitor.
As with other NSAIDs, the mechanism of the drug is associated with the chiral S form. Conversion of the R enantiomer into the S enantiomer has been shown to occur in the metabolism of ibuprofen; it is unknown whether it occurs in the metabolism of ketorolac.
Image:Ketorolac bottles.jpg
Indications
Ketorolac is indicated for short-term management of pain (up to five days).
Contraindications
Ketorolac is contraindicated against patients with a previously demonstrated hypersensitivity to ketorolac, and against patients with the complete or partial syndrome of nasal polyps, angioedema, bronchospastic reactivity or other allergic manifestations to aspirin or other non-steroidal anti-inflammatory drugs (due to possibility of severe anaphylaxis).
Adverse effects
Similar to other NSAIDs. See inset "Ketorolac adverse effects."
Warnings and precautions
The most serious risks associated with ketorolac are, as with other NSAIDs, gastrointestinal ulcerations, bleeding and perforation; renal events ranging from interstitial nephritis to complete renal failure; hemorhage, and hypersensitivity reactions.
As with other NSAIDs, fluid and solute retention and edema have been reported with ketorolac; ketorolac elevated liver protein levels; it also inhibits platelet aggregation and may be associated with an increased risk of bleeding.
Notes
Ketorolac is not recommended for pre-operative analgesia or co-administration with anesthesia because it inhibits platelet aggregation.
Ketorolac is not recommended for obstetric analgesia because it has not been adequately tested for obstetrical administration and has demonstrable fetal toxicity in laboratory animals.
Read more at Wikipedia.org