Some pharmaceutical drugs are known to cause bone loss. In November 2004, Depo-Provera Contraception Injection became the latest to join the list that also includes glucocorticoid medications, chemotherapy drugs for prostate and breast cancers, and SSRI antidepressants. The new black-box warning for Depo-Provera says that the drug causes bone density loss the longer the woman uses it and that this loss "may be clinically relevant." Because the bone loss cannot always be reversed, the FDA does not recommend that women who have other options use Depo-Provera as a long-term birth control method (e.g., longer than two years).
People who take glucocorticoid medicine (e.g., prednisone, prednisolone, dexamethasone, and cortisone) for more than three months also run the risk of osteoporosis, according to the American College of Rheumatology. Glucocorticoid drugs slow the rate of bone formation. They also "interfere with the body's handling of calcium and affect levels of sex hormones, leading to increased bone loss."
Androgen deprivation therapy, given to prostate cancer patients, is another treatment that increases the risk of osteoporotic bone fractures. Like glucocorticoids, the risk increases the longer the therapy is used. Despite the therapy's known effect on bones, few patients receive any screening, preventive care, or bone-loss treatment, according to Tawee Tanvetyanon, MD, Loyola University Chicago Stritch School of Medicine.
Women who were pushed into early menopause by chemotherapy used to treat early-stage breast cancer showed unexpectedly high bone loss in a study published by the Journal of Clinical Oncology (15 July 2001). Doctors from Dana-Farber Cancer Institute, Brigham, and Women's Hospital in Boston found that some women who entered chemotherapy-induced early menopause "lost as much as 8% of their bone in just one year [about four times the normal postmenopausal bone loss]." The doctors halted their study early so that women could receive treatment to prevent further bone loss.
Most recently, bone loss in animal studies have raised concerns about the use of selective serotonin reuptake inhibitor (SSRI) antidepressants in adolescents and children. Lab studies have shown that serotonin pathways, which are hampered by SSRIs, are linked to bone growth. In an article by Stuart J. Warden, PT, PhD, et al. published in an online edition of Endocrinology (11 November 2004), bone development was measured in normal mice, normal mice who received Prozac early in life, and mice who were genetically bred to mimic SSRI exposure. Both the bioengineered mice and those who received Prozac developed narrower, less dense bones than the controls. Because peak bone mass develops during adolescence, this research indicates a potential need for caution in prescribing SSRIs to youngsters.
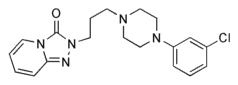
A human study, presented at the annual meeting of the American Society for Bone and Mineral Research (October 2004), linked SSRIs to bone loss in adults. The researchers found that mean bone-mineral density at the lumbar spine was 4.6% less among men taking SSRIs than for controls. In comparison, men taking glucocorticoids showed 2.9% less bone-mineral density than controls. Recognizing that depression is linked to other factors that contribute to bone loss (e.g., alcohol abuse, altered cortisol levels, etc.), the researchers also looked at participants who used tricyclic antidepressants or trazodone. The bone mineral density findings of men using these antidepressants did not differ significantly from controls.
Taking pharmaceutical drugs such as these is just part of the overall risk for brittle bones. Other recognized risk factors include old age; non-Hispanic white ethnic background; Asian ethnic background; small bone structure; family history of osteoporosis or osteoporosis-related fracture in a parent or sibling; previous fracture following a low-level trauma, especially after age 50; sex hormone deficiency; anorexia nervosa; cigarette smoking; alcohol abuse; low dietary intake or absorption of calcium and vitamin D; and sedentary lifestyle or immobility.
American College of Rheumatology. Glucocorticoid-Induced Osteoporosis. May 2004. www.rheumatology.org
Boyles, Salynn. Antidepressants May Affect Bone Growth. 11 November 2004 www.aolsvc.health.webmd.aol.com/content/Article/97/103972.htm
FDA issues Depo-Provera warning, testifies on Hill, 19 November 2004. www.medicalnewstoday.com
Kirn, Timothy F. Two studies Link SSRIs to Substantial Bone Loss. Ob.Gyn. News 1 December 2004
McKeown, L.A. Chemotherapy may Cause Some Women to Lose Bone. July 12, 2001 http://my.webmd.com
Reuters Health. Bone loss drug overused in breast cancer patients. 2000 March 13 www.personalmd.com
Stacy, Kelli Miller. Men Receiving Hormone Therapy Aren't Told About Prevention, Treatment. December 10, 2004. http://my.webmd.com
COPYRIGHT 2005 The Townsend Letter Group
COPYRIGHT 2005 Gale Group