Abstract
Intranasal corticosteroids are well known to be efficacious in the treatment of allergic rhinitis. Nasal irrigation with saline, including hypertonic saline, has long been recommended for the treatment of sinonasal disease, and it has been shown to have a positive effect on the physiology of the nasal mucosa. Until now, no study of the clinical efficacy of intranasal hypertonic Dead Sea saline as a monotherapyfor seasonal allergic rhinitis has been reported. We conducted a prospective, randomized, single-blind, placebo-controlled comparison of intranasal hypertonic Dead Sea saline spray and intranasal aqueous triamcinolone spray in 15 patients with seasonal allergic rhinitis. Results were based on a 7-day regimen. Based on Rhinoconjunctivitis Quality of Life Questionnaire scores, clinically and statistically significant (p < 0.0001) improvements were seen in both active-treatment groups; as expected, the corticosteroid spray was the more effective of the two treatments. No significant improvement occurred in the control group. Our preliminary results not only confirm the efficacy of intranasal corticosteroid therapy in moderate-to-severe allergic rhinitis, they also suggest that the Dead Sea saline solution can be an effective alternative in mild-to-moderate allergic rhinitis, particularly with respect to nasal and eye symptoms. The hypertonicity of the Dead Sea solution may have a positive effect on the physiology of the nasal mucosa by improving mucociliary clearance. In addition, the dominant cation in the Dead Sea solution--magnesium--probably exerts anti-inflammatory effects on the nasal mucosa and on the systemic immune response.
Introduction
Symptoms of seasonal allergic rhinitis are usually caused by tree, grass, and weed pollens. An important place to consider seasonal allergic rhinitis is Tulsa, Okla., which is located in the northeast region of the state and is known as "Green Country." The city lies at the threshold of two distinct zones--a deciduous forest area and a grasslands area--in which the population is exposed to a diversity of allergenic vegetation. (1) These two zones are populated by vegetation that accounts for 70% (127 of 181) of all allergenic species and by 79% (26 of 33) of the most allergenic species. (1)
The highest concentrations of airborne tree pollens are typically seen in the early spring. Genera include Quercus (oak), Juniperus (cedar), and Ulmus (elm). Quercus releases the most abundant pollen during any season. (2,3) Juniperus ashei (mountain cedar) pollen is carried upwind into the Tulsa area from southwest Oklahoma and west Texas during the fall and through the winter. (3,4)
In the late spring and early summer, pollens are released by other allergenic trees, such as Juglans regia (walnut) and Carya illinoensis (pecan). Also, a number of grasses pollinate from late spring through the summer; among the most allergenic are Cynodon dactylon (bermuda) and Phleum pratense (timothy). Fall is typically the season for Ambrosia trifida (giant ragweed), which is the second most abundant pollen in the Tulsa area; pollination usually peaks in mid-September and ends in early October.
In addition to allergen avoidance, proven treatments for seasonal allergic rhinitis include intranasal corticosteroids, oral and topical [H.sub.1] receptor antagonists (antihistamines), intranasal saline solutions, and occasionally immunotherapy; recently, treatment with leukotriene receptor antagonists has also been suggested. The superior effects of intranasal corticosteroids in sinonasal diseases have been established with respect to symptom resolution and quality of life. (5-12) Intranasal corticosteroids also have a significant effect on inflammatory mediators in allergic rhinitis. (13,14) In fact, when compared with oral antihistamines and with leukotriene receptor antagonists (with intranasal saline typically used as a control) for the treatment of seasonal allergic rhinitis, corticosteroids have been shown to be superior. (5,7,9,11,12)
The effects of intranasal hypertonic saline solutions are less clear. Some studies have shown that they exert beneficial effects on nasal physiology, mucociliary clearance in particular, (15-18) and that they help relieve symptoms and improve quality of life in patients with sinonasal disease. (19-21) Other studies, however, have shown that they have a negative effect on nasal physiology and no effect on symptoms of sinonasal disease. (22-24)
One such hypertonic saline solution is made from Dead Sea salts. The Dead Sea is the world's most saline lake body, and it contains proportionately more magnesium, calcium, bromine, and potassium and less sodium, sulfate, and carbonate than any ocean. (25) Magnesium is the dominant cation, accounting for approximately 35% of the composition of Dead Sea salts. This chemical composition makes Dead Sea salt unlike any other sea salt in the world. (26)
Treatment with Dead Sea salts has been shown to have positive effects on skin conditions such as psoriasis (27) and contact eczema. (28) The magnesium ion is believed to be primarily responsible for these positive effects. (27-30) Also, it is well established that magnesium in its intravenous, (31,32) inhaled and nebulized, (33-35) and dietary (36,37) forms plays a role in treating acute asthma, which is known to cause a reaction similar to an allergy.
A report from Italy revealed that intranasal hypertonic saline was beneficial in reducing the amount of as-needed antihistamines in a pediatric population with seasonal allergic rhinitis. (38) Until now, no study has been published regarding the effects of hypertonic saline as a monotherapy for seasonal allergic rhinitis. In this article, we describe what we believe is the first such preliminary study.
Patients and methods
Patient population. Our study population was originally made up of 21 patients who had presented to the family practice office of one of the authors (J.B.H.) seeking treatment for symptoms of seasonal allergic rhinitis. In order to be eligible for this study, patients had to be at least 18 years of age, had to have experienced at least two of six symptoms (nasal stuffiness, watery/itchy eyes, rhinorrhea, sneezing, postnasal drainage, and itchy throat/cough) at presentation, and had to have had a positive skin puncture test for seasonal allergens. Exclusion criteria included the presence of chronic sinusitis, nasal polyposis, a deviated nasal septum or history of nasal septal perforation, and recent nasal or sinus surgery; the use of an antihistamine, cromolyn, decongestant, or a topical or systemic corticosteroid within the preceding 2 weeks or an immunotherapeutic agent within the preceding 2 years; pregnancy and/or lactation; and chronic conditions such as head and neck cancer, human immunodeficiency virus-related nasal disease, cystic fibrosis, and renal, hepatic, pulmonary, and cardiovascular disease.
During the study, 6 of the 21 patients withdrew. Two patients withdrew because of adverse reactions, 2 did not return for the second of two scheduled visits, 1 was disqualified for antihistamine use during the study period, and 1 had stopped treatment prematurely. The final data analysis, therefore, was based on findings in the 15 patients--3 men and 12 women, aged 20 to 74 years (mean: 35.2 [+ or -] 16.05)--who completed both visits.
Written informed consent was obtained from all patients. The research protocol and the informed consent form were approved by the Institutional Review Board of Family Medical Care of Tulsa, Inc.
Study design. This randomized, single-blind, placebo-controlled study was conducted during 6 weeks of the spring allergy season in Tulsa, Okla. All patients were required to comply with the study protocol at two office visits. The treatment protocol was explained to them with both oral and written instructions.
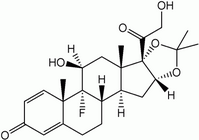
Patients were randomized into 3 groups of 5 each to receive either intranasal hypertonic Dead Sea saline spray (2 sprays into each nostril 3 times daily), aqueous triamcinolone spray (110 [micro]g into each nostril once daily), or a placebo nasal saline spray (2 sprays into each nostril 3 times daily) for 7 days.
At the first visit, each patient underwent skin-prick allergen testing for tree pollen (American elm, post oak, and mountain cedar), grass pollen (bermuda and timothy), short ragweed pollen, and Alternaria mold extract. Patients also completed the standardized version of the Rhinoconjunctivitis Quality of Life Questionnaire (RQLQ), once at the first visit and again at the completion of treatment. The RQLQ is a reliable, validated instrument with strong discriminative properties. (39,40) The survey contains 28 questions regarding 7 domains: activities, sleep, practical problems, nasal symptoms, eye symptoms, other symptoms, and emotional status. For each domain, patients rate themselves as to how much their symptoms have affected them during the previous week on a scale of 0 (no effect) to 6 (great effect).
Statistical analysis. Statistical analysis was performed with the assistance of the Excel statistical package (Microsoft; Redmond, Wash.) and confirmed by the Statistica 2003 package (StatSoft; Tulsa). Values analyzed were the mean RQLQ scores in each of the 7 domains and the overall composite scores. The Student's t test was figured from the composite scores. A one-sided hypothesis was used in anticipation of an expected reduction in composite scores after treatment; this helped obviate a type II error, which likely would have occurred in view of the small number of patients in this study.
Results
Following treatment, clinically and statistically significant improvements in mean composite RQLQ scores were seen in both the Dead Sea saline group and the corticosteroid group; no significant improvement occurred in the control group (table).
The Dead Sea saline group experienced a significant reduction in the mean composite RQLQ score, which fell from 3.38 to 2.02, a difference of 1.36 (p < 0.0001).
As expected, the corticosteroid group experienced the most marked overall improvement, as its mean composite RQLQ score declined from 3.24 to 1.03, a difference of 2.21 (p < 0.0001).
In the control group, the mean composite RQLQ score was 2.60 prior to treatment and 2.44 afterward, a difference of 0.16. The difference was not statistically significant (p = 0.6483). Likewise, there was no significant difference in any of the 7 domain scores pre- and posttreatment.
In both active-treatment groups, improvements were seen in all 7 individual domains. The greatest improvements in the Dead Sea saline group involved nasal symptoms (from 3.83 to 2.17, a difference of 1.66) and eye symptoms (from 3.00 to 2.04, a difference of 0.96). In the corticosteroid group, the greatest improvements involved eye symptoms (from 3.75 to 0.85, a difference of 2.90) and nasal symptoms (from 3.65 to 1.40, a difference of 2.25).
Discussion
Corticosteroids. Our expected finding that triamcinolone resulted in a statistically significant alleviation of severe symptoms and improvement in quality of life is consistent with the large body of evidence that intranasal corticosteroids are not only efficacious but superior for the treatment of seasonal allergic rhinitis. (5,7,9,11,12) It is interesting that of the 7 RQLQ domains, intranasal triamcinolone's greatest effect was on reducing eye symptoms (i.e., conjunctivitis). This suggests that allergic rhinitis is a disease of systemic immunologic response and that intranasal corticosteroids have a global effect rather than just a local effect.
Saline control. According to our analysis, nasal saline as the control preparation had no statistically significant effect on any RQLQ domain. Juniper et al, who developed the RQLQ, defined a clinically significant difference as "the smallest difference in score in the domain of interest which patients perceive as beneficial and would mandate a change in management," and they provided evidence that this difference is 0.5. (40) Based on this interpretation, the placebo in our study did lead to a clinically significant difference in three domains: sleep, eye symptoms, and emotional status. This finding supports the idea that although nasal saline is typically used as a control in studies of allergic rhinitis, it is not a genuine placebo. Ratner et al have suggested that oral nonsedative antihistamines have been shown to be no more effective than placebo aqueous nasal sprays in placebo-controlled studies in which the active comparator was an intranasal corticosteroid, but they have been shown to be superior to placebo tablets when the active comparator was another oral antihistamine. (11) In light of the findings by Ratner et al and their belief that intranasal saline washes the nasal mucosa of allergens and mucus, we suggest that the efficacy of intranasal saline might be equal to that of oral [H.sub.1] receptor antagonists for some patients with mild symptoms. Nasal saline may indeed play a role in the treatment of allergic rhinitis when it is delivered as a true irrigation agent rather than as just a simple moisturizer. One Tulsa allergist, Jane Purser, MD, recommends nasal saline irrigation with a minimum of 5 sprays in each nostril every morning, and she has observed some clinically significant improvements among her patients with chronic sinonasal disease (oral communication, February 2001). We believe that nasal saline spray as a placebo is probably adequate for research purposes, but it does provide some actual clinical benefit as an irrigant in some patients.
Dead Sea saline. The use of the intranasal hypertonic Dead Sea saline solution in our study resulted in some moderate but clinically and statistically significant improvement in posttreatment RQLQ scores. It was most effective in treating nasal symptoms. It was also significantly more effective than the placebo in all 7 domains. We believe ours is the first study to demonstrate the possible efficacy of intranasal hypertonic Dead Sea saline solution in alleviating symptoms and improving overall quality of life in patients with seasonal allergic rhinitis.
The Dead Sea solution's mechanism of action is unclear, but we can offer some possible explanations. Like the nasal saline placebo, it may act as a mild irrigant and physically clear mucus and inflammatory cells. It may also have positive effects on the physiology of the nasal mucosa and mucociliary clearance. (15,16) Finally, in view of its beneficial effect on eye symptoms, it may have global anti-inflammatory properties and affect the systemic immunologic response to allergic rhinitis.
Magnesium. Regarding the latter explanation, magnesium is the dominant cation in the Dead Sea saline solution, and it is reasonable to postulate that magnesium exerts some effect on inflammatory cells or inflammatory mediators. Asthma is known to be associated with increased amounts of eosinophils and has long been believed to cause a reaction similar to an allergy. Intravenous magnesium has been shown to be beneficial in the treatment of acute asthma, (31,32) and nebulized magnesium in combination with albuterol was shown to exert beneficial effects in a pediatric population in an emergency department in Detroit. (35) In another study, 36.8% of asthma patients who were treated for 4 weeks at the Dead Sea itself were able to discontinue their medications; even those who continued inhalation treatment were able to reduce the frequency of their puffs by 43%. (34) Dietary magnesium has positive effects, as well. Researchers in the United Kingdom found that a dietary regimen high in magnesium significantly improved lung function and lowered asthma symptom scores. (36,37) The role of magnesium in lung function is probably twofold: (1) Magnesium relaxes bronchial smooth muscle and thereby dilates airways, and (2) it may exert some influence on inflammatory cells and their subsequent release of inflammatory mediators.
Evidence of the positive effect that magnesium in Dead Sea salts has on some skin diseases was reported by Greiner and Diezel in Germany. (30) They administered water with a high concentration of magnesium ions to mice with allergenic contact dermatitis that had been induced by 1-chloro-2, 4-dinitrobenzene (DNCB). Mice that were challenged by DNCB plus magnesium chloride experienced significantly less inflammation than did mice that were challenged by DNCB alone and by DNCB plus sodium chloride. Greiner and Diezel confirmed these findings in 5 humans who had a known allergy to nickel; magnesium chloride suppressed nickel sulfate-induced contact dermatitis, and sodium chloride did not. (30) Another study from Germany by Ludwig et al revealed that high concentrations of magnesium ions inhibited the release of arachidonic acid (an important precursor of inflammatory mediators) and leukotriene B4 (a potent regulator in inflammatory reactions) in polymorphonuclear leukocytes. (41) Ludwig et al concluded that high concentrations of magnesium inhibit eicosanoid metabolism during the release of arachidonic acid by directly inhibiting the 5-lipoxygenase enzyme.
Magnesium probably stabilizes eosinophils (which under certain conditions degranulate major basic protein) and mast cells (which degranulate histamine). It has been demonstrated that when magnesium levels in the blood decrease, eosinophil and histamine levels subsequently increase. (42) It has also been shown that magnesium inhibits eosinophils from undergoing exocytosis and degranulation. (43) Allergic rhinitis typically begins with the exposure of IgE-bound mast cells to an allergen and progresses to subsequent mast cell degranulation and histamine release. Through a number of mechanisms, this activity causes symptoms of sneezing, rhinorrhea, nasal and ocular itchiness, eye watering, and cough. Chemotactic factors presumably modulate the influx of eosinophils, one of which is histamine. Magnesium administered intranasally via Dead Sea saline solution may inhibit eosinophil release of major basic protein and mast cell release of histamine, thereby inhibiting the local immune response and probably creating the anti-inflammatory effect of the systemic response.
Our data suggest that the use of intranasal hypertonic Dead Sea saline solution in a spray form results in a moderate reduction of symptoms and a moderate improvement in overall quality of life in patients with seasonal allergic rhinitis, and that it is probably useful in patients with mild-to-moderate symptoms. The Dead Sea solution also appears to be significantly better than nasal saline placebo in reducing symptoms and improving quality of life, and it probably exerts antiinflammatory effects on the nasal mucosa and the systemic inflammatory response. Patients with moderate-to-severe symptoms should probably be treated with an intranasal corticosteroid, with or without a nasal wash with Dead Sea saline solution. It is possible that a different delivery system--namely irrigation--may enhance the positive effects of the Dead Sea solution, and we hope that such a study can be undertaken.
In conclusion, it appears that the intranasal hypertonic Dead Sea saline solution is superior to plain saline solution in the treatment of seasonal allergic rhinitis. However, in view of the small number of patients in our study, these results are only preliminary. Fortunately, several studies are under way to help confirm or refute our conclusion.
References
(1.) Levetin E, Buck P. Hay fever plants in Oklahoma. Ann Allergy 1980;45:26-32.
(2.) Levetin E, Larsen-Purvis M. Tulsa Pollen Calendar. The University of Tulsa Aerobiology Laboratory.
(3.) Levetin E. A long-term study of winter and early spring tree pollen in the Tulsa, Oklahoma atmosphere. Aerobiologia 1998;14:21-8.
(4.) Levetin E, Buck P. Evidence of mountain cedar pollen in Tulsa. Ann Allergy 1986;56:295-9.
(5.) Kaszuba SM, Baroody FM, deTineo M, et al. Superiority of an intranasal corticosteroid compared with an oral antihistamine in the as-needed treatment of seasonal allergic rhinitis. Arch Intern Med 2001;161:2581-7.
(6.) Parikh A, Scadding GK, Darby Y, Baker RC. Topical corticosteroids in chronic rhinosinusitis: A randomized, double-blind, placebo-controlled trial using fluticasone propionate aqueous nasal spray. Rhinology 2001;39:75-9.
(7.) Weiner JM, Abramson MJ, Puy RM. Intranasal corticosteroids versus oral H1 receptor antagonists in allergic rhinitis: Systematic review of randomized controlled trials. BMJ 1998;317(7173):1624-9.
(8.) Mabry RL. Pharmacotherapy of allergic rhinitis: Corticosteroids. Otolaryngol Head Neck Surg 1995;113:120-5.
(9.) Jen A, Baroody F, deTineo M, et al. As-needed use of fluticasone propionate nasal spray reduces symptoms of seasonal allergic rhinitis. J Allergy Clin Immunol 2000;105:732-8.
(10.) Juniper EF, Kline PA, Hargreave FE, Dolovich J. Comparison of beclomethasone dipropionate aqueous nasal spray, astemizole, and the combination in the prophylactic treatment of ragweed pollen-induced rhinoconjunctivitis. J Allergy Clin Immunol 1989;83: 627-33.
(11.) Ratner PH, van Bavel JH, Martin BG, et al. A comparison of the efficacy of fluticasone propionate aqueous nasal spray and loratadine, alone and in combination, for the treatment of seasonal allergic rhinitis. J Fam Pract 1998;47:118-25.
(12.) Pullerits T, Praks L, Skoogh BE, et al. Randomized placebo-controlled study comparing a leukotriene receptor antagonist and a nasal glucocorticoid in seasonal allergic rhinitis. Am J Respir Crit Care Med 1999;159:1814-18.
(13.) Benson M, Strannegard IL, Strannegard O, Wennergren G. Topical steroid treatment of allergic rhinitis decreases nasal fluid TH2 cytokines, eosinophils, eosinophil cationic protein, and IgE but has no significant effect on IFN-gamma, IL-1beta, TNF-alpha, or neutrophils. J Allergy Clin Immunol 2000;106:307-12.
(14.) Nielsen LP, Bjerke T, Christensen MB, et al. Eosinophil markers in seasonal allergic rhinitis. Intranasal fluticasone propionate inhibits local and systemic increases during the pollen season. Allergy 1998;53:778-85.
(15.) Talbot AR, Herr TM, Parsons DS. Mucociliary clearance and buffered hypertonic saline solution. Laryngoscope 1997:107:500-3.
(16.) Homer JJ, England RJ, Wilde AD, et al. The effect of pH of douching solutions on mucociliary clearance. Clin Otolaryngol 1999;24: 312-15.
(17.) Tomooka LT, Murphy C, Davidson TM. Clinical study and literature review of nasal irrigation. Laryngoscope 2000;110:1189-93.
(18.) Homer JJ, Dowley AC, Condon L, et al. The effect of hypertonicity on nasal mucociliary clearance. Clin Otolaryngol 2000;25:558-60.
(19.) Shoseyov D, Bibi H, Shai P, et al. Treatment with hypertonic saline versus normal saline nasal wash of pediatric chronic sinusitis. J Allergy Clin Immunol 1998;101:602-5.
(20.) Heatley DG, McConnell KE, Kille TL, Levcrson GE. Nasal irrigation for the alleviation of sinonasal symptoms. Otolaryngol Head Neck Surg 2001;125:44-8.
(21.) Rabago D, Zgierska A, Mundt M, et al. Efficacy of daily hypertonic saline nasal irrigation among patients with sinusitis: A randomized controlled trial. J Faro Pract 2002;51:1049-55.
(22.) Min YG, Lee KS, Yun JB, et al. Hypertonic saline decreases ciliary movement in human nasal epithelium in vitro. Otolaryngol Head Neck Surg 2001;124:313-16.
(23.) Boek WM, Keles N, Graamans K, Huizing EH. Physiologic and hypertonic saline solutions impair ciliary activity in vitro. Laryngoscope 1999;109:396-9.
(24.) Adam P, Stiffman M, Blake RL, Jr. A clinical trial of hypertonic saline nasal spray in subjects with the common cold or rhinosinusitis. Arch Fam Med 1998;7:39-43.
(25.) Even-Paz Z, Shani J. The Dead Sea and psoriasis. Historical and geographic background. Int J Dermatol 1989;28:1-9.
(26.) Nissenbaum A. Minor and trace elements in Dead Sea water. Chem Geol 1977;19:99-111.
(27.) Goldberg LH, Sagher F. Psoriasis treatment at the Dead Sea. Cutis 1975;16:61-2.
(28.) Schiffner R, Schiffner-Rohe J, Gerstenhauer M, et al. Dead Sea treatment--Principle for outpatient use in atopic dermatitis: Safety and efficacy of synchronous balneophototherapy using narrow-band UVB and bathing in Dead Sea salt solution. Eur J Dermatol 2002;12:543-8.
(29.) Levi-Schaffer F, Shani J, Politi Y, et al. Inhibition of proliferation of psoriatic and healthy fibroblasts in cell culture by selected Dead Sea salts. Pharmacology 1996;52:321-8.
(30.) Greiner J, Diezel W. [Inflammation-inhibiting effect of magnesium ions in contact eczema reactions]. Hautarzt 1990;41:602-5.
(31.) Keen JH. Intravenous magnesium sulfate for acute asthma. J Emerg Nuts 1995;21:44-6.
(32.) Ciarallo L, Sauer AH, Shannon MW. Intravenous magnesium therapy for moderate to severe pediatric asthma: Results of a randomized, placebo-controlled trial. J Pediatr 1996;129:809-14.
(33.) Rolla G, Bucca C, Bugiani M, et al. Reduction of histamine-induced bronchoconstriction by magnesium in asthmatic subjects. Allergy 1987;42:186-8.
(34.) Harari M, Barzillai R, Shani J. Magnesium in the management of asthma: Critical review of acute and chronic treatments, and Deutches Medizinisches Zentrum's (DMZ's) clinical experience at the Dead Sea. J Asthma 1998;35:525-36.
(35.) Mahajan PV, Rosenberg N, Sethuraman U, Dimitri H. Comparison of nebulized magnesium plus albuterol to nebulized albuterol alone in children with mild to moderate asthma. Presented at the annual meeting of the American Academy of Pediatrics; Oct. 19-23, 2002; Boston.
(36.) Hill J, Micklewright A, Lewis S, Britton J. Investigation of the effect of short-term change in dietary magnesium intake in asthma. Eur Respir J 1997;10:2225-9.
(37.) Britton J, Pavord I, Richards K, et al. Dietary magnesium, lung function, wheezing, and airway hyperreactivity in a random adult population sample. Lancet 1994;344:357-62.
(38.) Garavello W, Romagnoli M, Sordo L, et al. Hypersaline nasal irrigation in children with symptomatic seasonal allergic rhinitis: A randomized study. Pediatr Allergy Immunol 2003;14:140-3.
(39.) Juniper EF, Thompson AK, Ferrie PJ, Roberts JN. Validation of the standardized version of the Rhinoconjunctivitis Quality of Life Questionnaire. J Allergy Clin Immunol 1999;104(2 Pt 1):364-9.
(40.) Juniper EF, Guyatt GH, Griffith LE, Ferrie PJ. Interpretation of rhinoconjunctivitis quality of life questionnaire data. J Allergy Clin Immunol 1996;98:843-5.
(41.) Ludwig P, Petrich K, Schewe T, Diezel W. Inhibition of eicosanoid formation in human polymorphonuclear leukocytes by high concentrations of magnesium ions. Biol Chem Hoppe Seyler 1995;376:739-44.
(42.) Chyrek-Borowska S, Obrzut D, Hofman J. The relation between magnesium, blood histamine level and eosinophilia in the acute stage of the allergic reactions in humans. Arch Immunol Ther Exp (Warsz) 1978;26:709-12.
(43.) Larbi KY, Gomperts BD. Complex pattern of inhibition by magnesium of exocytosis from permeabilised eosinophils. Cell Calcium 1997;21:213-19.
Dr. Cordray is an otolaryngologist in private practice. Dr. Harjo is a family physician in private practice. Dr. Miner is director of academic programs at Southern Nazarene University. All are located in Tulsa, Okla.
Reprint requests: Scott Cordray, DO, Hillcrest Physicians Bldg., 1145 S. Utica Ave., #513, Tulsa, OK 74104. Phone: (918) 582-8217; fax: (918) 582-8219; e-mail: scordray@cfaith.com
COPYRIGHT 2005 Medquest Communications, LLC
COPYRIGHT 2005 Gale Group