Experience from clinical and medicolegal practice has led us to question whether it is still reasonable to supplement an arthroscopic lavage or debridement operation with an intraarticular injection of steroid. We do not suggest that this is common practice but it is clear from new cases seen, and from discussions with trainees, that it occurs sporadically in the UK. A survey in the Trent and Yorkshire regions revealed that approximately 5% of surgeons are routinely using steroids after arthroscopy (Bickerstaff, personal communication). Are there any advantages to the use of intraarticular injections of steroid and are there increased risks of developing septic arthritis in these circumstances?
Osteoarthritis is primarily a disease of articular cartilage. Buckwalter and Mankin1 prefer the term osteoarthrosis, since this reflects more accurately our current understanding of the pathogenesis of this disorder. While synovitis is often present, inflammation is not a major component. Arthroscopic lavage and debridement, popularised by Burman, Finkelstein and Mayer and Sprague, are now widely practised for the treatment of mild to moderate osteoarthrosis and rates of success of between 50% and 75% are claimed. 3-9 These early outcomes deteriorate over time.10,11
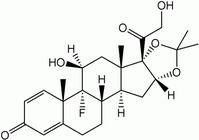
Intra-articular injections of corticosteroids have been used for the treatment of osteoarthritis of the knee for 30 years, but there is little controlled evidence to support their use. 12-14 Their adverse effects have been reported widely, particularly concerning the articular cartilage, the synovium and the host immune response. Rupture of tendons has been observed after local injections of corticosteroids,15 and in the knee there may be concern as to their effect on the cruciate ligaments.
Steroids and articular cartilage
In 1959 Chandler et al 16 described a patient with osteoarthritis of the hip who had received 900 mg of hydrocortisone over one year. They coined the term `Charcot arthropathy', since the affected joint resembled a Charcot joint radiologically and histologically. In 1969 Bentley and Goodfellow noted similar severe destructive changes in the knees of a 73-year-old woman with osteoarthritis after repeated injections of hydrocortisone. They commented that "the case against multiple injections is so strong that the practice should, in our opinion, be discarded, which implies that even a single injection requires strong justification".
Mankin and Conger 18 reported the deleterious effects of intra-articular injections of hydrocortisone acetate on the articular cartilage in rabbits. They demonstrated decreased uptake of [ 3H]-glycine by the cartilage after intra-articular injection of hydrocortisone acetate. In another study 19 they showed that cortisol, given either systemically or intraarticularly, produced a profound depression of incorporation of [14C]-glycine into cartilage. They concluded that intra-articular injections of steroids led to decreased synthesis of the matrix during the period of its effect, since incorporation of [3H]-glycine can be equated with protein synthesis and a decrease in its utilisation would indicate a decline in the rate of synthesis. Recovery was noted to be slow and dose-dependent. 20
Behrens, Shepard and Mitchell described a progressive loss of the endoplasmic reticulum, mitochondria and Golgi apparatus in chondrocytes from the knees of rabbits treated with intra-articular hydrocortisone acetate. Salter, Gross and Hall 21 demonstrated a loss of the normal lustre of the articular surface, thinning of the cartilage and the development of fissures and fibrillation after the intra-articular administration of hydrocortisone tertiary-butyl acetate into the knees of rabbits. They found multiple small white deposits within the substance of the articular cartilage which were found to represent cystic areas of degeneration within the middle zone of the cartilage matrix.
Moskowitz et al 22 also observed these lesions and found that the number of cysts seemed to parallel the number of injections of corticosteroids. These findings suggest that the clinical and radiological deterioration reported in human joints after intra-articular injections of corticosteroids may be due to the specific deleterious effect of the drug on the metabolism of articular cartilage. However, in the only study in primates, injections of steroid into the knees of monkeys produced only minimal, reversible changes.23
Pelletier and Martel-Pelletier found that glucocorticoid, administered orally or intra-articularly, is effective against the development of osteoarthritic lesions in the Pond-Nuki dog model of osteoarthritis. They studied 12 dogs in which the anterior cruciate ligament had been sectioned. Six were treated with oral prednisone and six with an intra-articular injection of triamcinolone hexacetonide, at operation and four weeks later. Twelve other dogs had the operation but no other treatment. All the animals were killed eight weeks after surgery. There was no evidence of increased cell degeneration or death associated with the steroids. In a separate study of experimental osteoarthritis in mongrel dogs, the anterior cruciate ligaments of which had been sectioned by a stab wound, Pelletier et al 25 observed a protective effect of the corticosteroid injections on osteoarthritic lesions by suppression of the synthesis of stromelysin in chondrocytes.
Steroids and the synovium
Steroid flare, an acute self-limiting synovitis, may follow the intra-articular injection of corticosteroid and lasts for up to 48 hours. It is seen in 1% to 10% of cases, depending on the dose, choice of agent, and the technique of administration.26
Immunosuppression
Corticosteroids impair local and systemic immune defences. Intra-articular injections have been observed to suppress the hypothalamus-pituitary-adrenal axis for up to seven days.27-29 Schurman, Johnson and Amstutz 30 demonstrated in a rabbit model that a single dose of 5 mg of prednisolone, given at the time of bacterial inoculation of the knee with micrococci, prolonged the period when organisms could be cultured from the knee and potentiated the destructive changes caused by the infection. Fuenfer, Olson and Polk 31 studied the effect of various corticosteroids on the phagocytic bactericidal activity of neutrophils. They concluded that hydrocortisone sodium phosphate and hydrocortisone sodium succinate significantly depressed bactericidal activity. Dexamethasone sodium phosphate had a marginal inhibitory effect and methylprednisolone sodium succinate failed to decrease neutrophil function below that of the control level. The mechanism for the increased risk of infection in patients given intra-articular steroids may be that those who receive a very low-dose inoculation of organisms during surgery usually overcome it, but may not achieve this in the presence of corticosteroids, which impair local and systemic immune defences.
Infection after arthroscopy
Septic arthritis after arthroscopy of the knee is a rare but serious complication. DeLee 32 reported a rate of infection of 0.08% in a study of over 100 000 arthroscopies. Johnson et al 33 and D'Angelo and Ogilvie-Harris,34 found infection in 0.04% of 12 505 arthroscopies, and in 0.23% of 4000 patients, respectively. None of these studies analysed the risk factors associated with the occurrence of infection. The most common organism was Staphlococcus aureus. Allum and Ribbans 35 reported one case of infection organ 96 patients after arthroscopy. This was in a patient with degenerative changes who had been given an injection of DepoMedrone. No intra-articular surgery was carried out. Four days later he played squash. At two weeks he developed septic arthritis seconday to infection with beta-haemolytic cases of septic arthritis in over 1500 arthroscopies in a tenyear period. All of their patients had had injections of steroids at the time of arthroscopy. They recommended that intra-articular steroids should not be given for some weeks after arthroscopy and endorsed the advice of Allum and Ribbans against vigorous activity during this time.
Armstrong, Bolding and Joseph had an infection rate of 0.42% in 4256 knee arthroscopies. They analysed the associated risk factors. The occurrence of infection was more common in patients with a longer operating time, an increased number of procedures during surgery, prior operations, and after chondroplasty or soft-tissue debridement, but the most significant factor was the intraoperative injection of methylprednisolone acetate. Five of the 18 infected patients had received corticosteroids. Some patients with septic arthritis presented within two days of operation, while in others there was a delay of up to 11 days. The early cases were almost all caused by Staphylococcus aureus, whereas the infecting organisms were more varied in the later cases. In a separate series, Armstrong and Bolding 38 found four cases of septic arthritis after 101 arthroscopic procedures, three in the knee and one in the shoulder. Although there were some environmental factors contributing to the high rates of infection, three of the four patients had received intraoperative injection of corticosteroid. They commented that the likelihood of infection was at least 20 times greater when corticosteroids were used. The three cases reported by Montgomery and Campbell,36 presented at 6, 11 and 24 days after operation. Staphylococcus aureus was the infecting organism in the first two cases and Pseudomonas aeruginosa in the later one.
Our recent experience
We have encountered six cases of septic arthritis of the knee in medicolegal practice over the last 18 months. All the patients had had intra-articular injection of steroid at the time of operation, and in all the diagnosis was mild to moderate osteoarthritis. The infective organism was
Staphylococcus aureus in each case. The presentation of septic arthritis was delayed for six to 12 days after the initial arthroscopy, which seems to be a feature of steroidrelated infection.
Conclusion
There is no clear evidence that steroids are beneficial to the osteoarthritic knee, but they may well be harmful. Experimental studies suggest that there is an increased risk of infection with the intraoperative use of steroids.37 This is supported by a small but increasing number of medicolegal cases involving infection after arthroscopy of the knee with injection of steroids.
Thirty years ago in an Editorial for the British volume of the Journal of Bone and Joint Surgery, Sweetnam 39 stated that "we now have evidence, both clinical and experimental, that apart from the well recognised hazard of infection, intra-articular injections of corticosteroids, certainly, if repeated, may be harmful", yet the practice has continued. We believe that it should now cease.
References
1. Buckwalter JA, Mankin HJ. Articular cartilage. Part II. Degeneration and osteoarthrosis, repair. regeneration, and transplantation. J Bone Joint Surg [Am] 1997;79-A:612-32.
2. Burman MS, Finkelstein H, Mayer L. Arthroscopy of the knee joint. J Bone Joint Surg 1934;16:255-68.
3. Sprague NF. Arthroscopic debridement for degenerative knee joint disease. Clin Orthop 198[;[60:118-23.
4. Jackson RW, Silver R, Marans J. Arthroscopic treatment of degenerative joint disease. J Arthroscopy 1986;2:114.
5. Jackson RW, Marans HJ, Silver RS. The arthroscopic treatment of degenerative arthritis of the knee. J Bone Joint Surg [Br] 1988;71-B: 332.
6. Bert JM, Maschka K. The arthroscopic treatment of unicompartmental gonarthrosis: a five-year follow-up study of abrasion arthroplasty plus arthroscopic debridement and arthroscopic debridement alone. JArthroscopy 1989;5:25-32.
7. Baumgaertner MR, Cannon WD Jr, Vittori JM, Schmidt ES, Maurer RC. Arthroscopic debridement of the arthritic knee. Clin Orthop 1990;253:197-202.
8. Gross DE, Brenner SL, Esformes I, Gross ML. Arthroscopic treatment of degenerative joint disease of the knee. Orthopedics 1991;14: 1317-21.
9. Rand JA. Role of arthroscopy in osteoarthritis of the knee. J Arthroscopy 1991;7:358-63.
10. Goldman RT, Scuderi GR, Kelly MA. Arthroscopic treatment of the degenerative knee in older athletes. Clin Sports Med 1997;16:51-68.
11. Livesley PJ, Doherty M, Needoff M, Moulton A. Arthroscopic lavage of osteoarthritic knees. J Bone Joint Surg [Br] 1991;73-B: 922-6.
12. Gray RG, Gottlieb NL. Intra-articular corticosteroids: an updated assessment. Clin Orthop 1983;177:235-63.
13. Dieppe PA, Sathapatayavongs B, Jones HE, Bacon PA, Ring EF. Intra-articular steroids in osteoarthritis. Rheumatoid Rehabil 1980;19: 212-7.
14. Friedman DM, Moore ME. The efficacy of intraarticular steroids in osteoarthritis: a double blind study. J Rheumatol 1980;7:850-6.
15. Ismail AM, Balakrishnan R, Rajkumar MK. Rupture of patellar ligament after steroid infiltration: report of a case. J Bone Joint Surg [Br] 1969;51-B:503-5.
16. Chandler GN, Jones DT, Wright V, Hartfall SJ. Charcot's arthropathy following intra-articular hydrocortisone. Br Med J 1959;1: 952-3.
17. Bentley G, Goodfellow JW. Disorganisation of the knees following intra-articular hydrocortisone injections. J Bone Joint Surg [Br] 1969; 51 -13:498-502.
18. Mankin HJ, Conger KA. The acute effects of intra-articular hydrocortisone on articular cartilage in rabbits. J Bone Joint Surg [Am] 1966;48-A:1383-8.
19. Mankin HJ, Conger KA. The effect of cortisol on articular cartilage of rabbits: effect of a single dose of cortisol on glycine C-14 incorporation. Lab Invest 1966;15:794-800.
20. Behrens F, Shepard N, Mitchell N. Alteration of rabbit articular cartilage by intra-articular injections of glucocorticoids. J Bone Joint Surg [Am] 1975;57-A:70-6.
21. Salter RB, Gross A, Hall JH. Hydrocortisone arthropathy: an experimental investigation. Can Med Assoc J 1967;97:374-7.
22. Moskowitz RW, Davis W, Sammarco J, Mast W, Chase SW. Experimentally induced corticosteroid arthropathy. Arthritis Rheum 1970;13:236-43.
23. Gibson T, Burry HC, Poswillo D, Glass J. Effect of intra-articular corticosteroid injections on primate cartilage. Ann Rheum Dis 1977; 36:74-9.
24. Pelletier JP, Martel-Pelletier J. Protective effects of corticosteroids on cartilage lesions and osteophyte formation in the Pond-Nuki dog model of osteoarthritis. Arthritis Rheum 1989;32:181-93.
25. Pelletier JP, Mineau F, Raynauld JP, et al. Intra-articular injections with methylprednisolone acetate reduce osteoarthritic lesions in parallel with chondrocyte stromelysin synthesis in experimental osteoarthritis. Arthritis Rheum 1994;37:414-23.
26. Stefanich RJ. Intraarticular corticosteroids in treatment of osteoarthritis. Orthop Rev 1986;15:65-71.
27. Armstrong RD, English J, Gibson T, Chakraborty J, Marks V. Serum methylprednisolone levels following intra-articular injection of methylprednisolone acetate. Ann Rheum Dis 1981;40:571-4.
28. Reeback JS, Chakraborty J, English J, Gibson T, Marks V. Plasma steroid levels after intra-articular injection of prednisolone acetate in patients with rheumatoid arthritis. Ann Rheum Dis 1980;39:22-4.
29. Shuster S, Williams IA. Adrenal suppression due to intra-articular corticosteroid therapy. Lancet 1961;2:17t-2.
30. Schurman DJ, Johnson BL, Amstutz HC. Knee joint infections with Staphylococcus aureus and micrococcus species: influence of antibiotics, metal debris, bacteremia, blood and steroids in a rabbit model. J Bone Joint Surg [Am] 1975;57-A:40-9.
31. Fuenfer MM, Olson GE, Polk HC. Effect of various corticosteroids upon the phagocytic bactericidal activity of neutrophils. Surgery 1975;78:27-33.
32. DeLee JC. Chairman, Committee on complications of Arthroscopy Association of North America: complications of arthroscopy and arthroscopic surgery: results of a national survey. Arthroscopy 1985; 1:214-20.
33. Johnson LL, Schneider DA, Austin MD, et al. Two per cent glutaraldehyde: a disinfectant in arthroscopy and arthroscopic surgery. J Bone Joint Surg [Am/ 1982;64-A:237-9.
34. D'Angelo GL, Ogilvie-Harris DJ. Septic arthritis following arthroscopy, with cost/benefit analysis of antibiotic prophylaxis. Arthroscopy 1988;4:10-4.
35. Allum RL, Ribbans WJ. Day case arthroscopy and arthroscopic surgery of the knee. Ann R Coll Sug Engl 1987;69:225-6.
36. Montgomery SC, Campbell J. Septic arthritis following arthroscopy and intra-articular steroids. J Bone Joint Surg [Br] 1989;71-B:540.
37. Armstrong RW, Bolding F, Joseph R. Septic arthritis following arthroscopy: clinical syndromes and analysis of risk factors. Arthroscopy 1992;8:213-23.
38. Armstrong RW, Bolding F. Septic arthritis after arthroscopy: the contributing roles of intraarticular steroids and environmental factors. Am J Infect Control 1994;22:16-8.
39. Sweetnam R. Editorial. Corticosteroid arthropathy and tendon rupture. J Bone Joint Surg [Brl 1969;51-13:397-8.
H. S. Gosal, FRCS, Specialist Registrar in Orthopaedics A. M. Jackson, FRCS, Consultant Orthopaedic Surgeon
Department of Orthopaedic Surgery, 5th Floor, St James's Wing, St George's Hospital, Blackshaw Road, London SW17 OQT. UK.
D. R. Bickerstaff, MD, FRCS, FRCS Ed, Consultant Orthopaedic Surgeon
Knee Surgery & Sports Trauma Unit, Northern General Hospital, Herries Road, Sheffield SS 7AU, UK.
Correspondence should be sent to Mr H. S. Gosal at 10 Gatley Drive, Bu Guildford. Surrey GU4 7JJ UK.
Copyright British Editorial Society of Bone & Joint Surgery Nov 1999
Provided by ProQuest Information and Learning Company. All rights Reserved