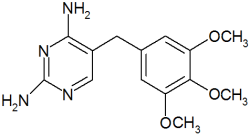
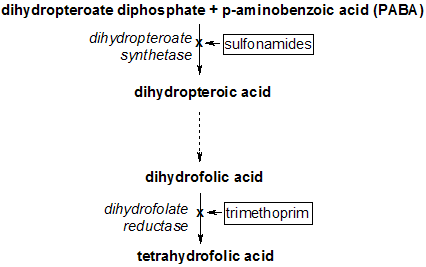
The effective empiric treatment of cystitis and the need to avoid unnecessarily promoting resistance to second-line antibiotics are competing priorities that challenge family physicians. Trimethoprim/sulfamethoxazole (TMP/SMX) has long been an effective choice for first-line therapy of uncomplicated cystitis, but concerns have been raised about growing resistance among urinary pathogens. Brown and colleagues performed a retrospective cohort study of women with acute uncomplicated cystitis and determined which clinical factors predict a higher likelihood of encountering a resistant urinary pathogen.
The investigators examined 601 isolates of Escherichia coli recovered from 1992 to 1999 during prospective studies of urinary tract infection (UTI) at a university hospital center and at primary care clinics in Michigan. All samples were from adult women, and most were collected at an outpatient hospital-based clinic. UTI was defined as at least one urinary symptom (e.g., dysuria) and at least 1,000 colonies per mL of E. coli from a clean-catch urine sample.
Resistance to TMP/SMX among the E. coli isolates increased from 8.1 to 15.8 percent over the seven years of the study. Women with a history of UTIs were no more likely to be resistant than patients with a first infection. A woman's age did not significantly affect the likelihood of resistance, nor did the use of oral contraceptives or hormone-replacement therapy, in contrast to the findings of other recent studies.
Recent antibiotic use, however, did affect the prevalence of resistance. Use of any antibiotic within the two weeks before the cystitis episode doubled the risk of TMP/SMX resistance. If TMP/SMX had been used, the likelihood of resistance increased 16-fold, although the subgroup of women who had previously used TMP/SMX comprised only seven patients. Laboratory determination of resistance correlated with clinical treatment failure, which was defined as a patient telephone call or repeat visit for persistent urinary symptoms within two weeks of the treatment start date. Women with a resistant pathogen had a clinical failure rate of 45.5 percent, versus a 4.2 percent failure rate in women without resistance. There was a trend toward higher failure rates for shorter antibiotic courses (e.g., three days), but it was not statistically significant.
The authors concluded that TMP/SMX resistance among E. coli urinary isolates increased over the seven years of their study, and that recent use of an antibiotic doubled the likelihood of a resistant pathogen, particularly if TMP/SMX had been used.
EDITOR'S NOTE: Before consigning TMP/SMX to obsolescence, family physicians will want to consider the very low likelihood of clinical failure leading to a serious complication (e.g., pyelonephritis). The greater goal of avoiding increased resistance to second-line antibiotics may be worth a quick telephone call to redirect antibiotic therapy for patients with persistent symptoms after first-line treatment. Even among women with resistant pathogens, TMP/SMX worked 55 percent of the time, although it may be a less wise empiric choice in patients with recent antibiotic use.--B.Z.
COPYRIGHT 2002 American Academy of Family Physicians
COPYRIGHT 2002 Gale Group